Abstract
The COVID-19 pandemic has significantly disrupted the lives of children and their caregivers. Recent research has examined the impact of the pandemic on child and caregiver functioning but there is a paucity of work examining the impact of the pandemic on the broader family system. The current study examined family resilience during the COVID-19 pandemic across three aims: Aim 1 tested whether meaning, control, and emotion systems form a unitary family adaption factor, Aim 2 evaluated a concurrent model of family resilience, and Aim 3 examined whether parent gender and vaccination status moderated paths in the final model. A nationally representative sample of U.S. parents (N = 796; 51.8% fathers, M age = 38.87 years, 60.3% Non-Hispanic White) completed a cross-sectional survey about themselves and one child (5–16 years old) between February-April 2021, including measures of COVID-19 family risk and protective factors, pre-existing family health vulnerabilities, race, COVID-19 stressors, and family adaptation. Confirmatory Factor Analysis demonstrated that the meaning (i.e., family making meaning of COVID-19), control (i.e., stability in routines), and emotional (i.e., family support) facets of family adaptation are unique but related. A path model revealed that there were concurrent effects from COVID-19 exposure, pre-existing vulnerabilities, and racial diversity status to the family protective, vulnerability, and adaptation variables. Additionally, parent COVID-19 vaccination status altered the association between pre-existing family health vulnerabilities and the family protective factor. Overall, results underscore the importance of examining pre-existing and concurrent risk and protective factors for family resilience during a stressful, global, and far-reaching event.
Highlights
-
A unitary factor of family adaptation comprised of meaning, control, and emotional support variables was not supported.
-
A concurrent path model of family resilience during the COVID-19 pandemic provided an acceptable fit to the data.
-
COVID-19 exposure, pre-existing vulnerabilities, and racial diversity status were associated with the adaptation variables.
-
COVID-19 emotional vulnerability and demographic protection were also concurrently associated with family adaptation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The COVID-19 pandemic resulted in school, work, and community closures and restrictions that have significantly disrupted the lives of children and their caregivers. These closures were essential in stopping the initial spread of the COVID-19 virus, but they have had a detrimental impact on child (Liu et al., 2021; Marques de Miranda et al., 2020) and caregiver (Taubman-Ben-Ari et al., 2021; Calvano et al., 2021; Ren et al., 2020) mental health. In this background, Prime and colleagues (2020) proposed a model of family risk and resilience during the COVID-19 pandemic that theorized that these disruptions have had a cascading influence to caregiver distress, which in turn has impacted overall family functioning, including parent-child relationships, spousal relationships, and sibling relationships. These changes to the family unit may lead to subsequent disruptions in child well-being (Prime et al., 2020). Moreover, family functioning may be particularly important during the COVID-19 pandemic given that in some instances family members remained the only social interaction for children and caregivers. Indeed, qualitative research demonstrated increased family strain during the pandemic (Evans et al., 2020). Interestingly, some families also reported positive changes, such as stronger relationships and more opportunities for appreciation (Evans et al., 2020). Identifying how families positively adapted to the pandemic can pinpoint areas of intervention for future family disruptions, including those related to the ongoing COVID-19 pandemic. The current study examined a concurrent model of family resilience using the family resilience model (Henry et al., 2015). This model was used to specify the direction of concurrent associations, such that COVID-19 stressors were theorized to influence family protective factors, family vulnerability factors, and overall family adaptation during the pandemic.
Family Resilience Model
Current research on family resilience converges on the understanding that when families experience a stressor, they can experience increased adaptation through protective factors or hindered adaptation through vulnerability factors (Henry et al., 2015; Walsh, 2016). Importantly, families may bounce back from challenging events and sometimes emerge stronger than ever (Walsh, 2016). The family resilience model (FRM) is one model that addresses family adaptation from stressors through four key characteristics: family risk, family protective factors, family vulnerability factors, and family adaptation (Henry et al., 2015). First, there is the presence of family risk, which draws on a family’s protective and vulnerability factors to predict adaptation within the family unit. Family protective and vulnerability factors are features that increase a family’s ability to cope with risk or enhance risk, respectively. Finally, family adaptation is the response to these risks, protection, and vulnerability factors (Henry et al., 2015). Families are conceptualized as a dynamic system in the FRM where there is not a clear delineation between a start and an end point for any factors in the model (Harrist et al., 2019). Instead, the model is focused around the presence of certain stressors, such as the COVID-19 pandemic, where protective factors can include existing strengths, and therefore, vertical risk factors, (e.g., marriage status and income) which are generally more stable, can still be specified as an ongoing protective factor that is activated in the presence of a certain stressor (Harrist et al., 2019).
Family adaptive systems (FAS) are “relationship patterns (p. 30)” and include the maintenance system, the meaning system, the control system, and the emotion system (Henry et al., 2015). The meaning system reflects how families contextualize and interpret the world around them. During the pandemic, this system may reflect a family’s attempt to make positive meaning of the pandemic, which is how we assessed meaning in the current study. The emotion system focuses on the emotional climate within a system, including how connected and supported the family feels to one another during the pandemic. The control system reflects the distribution of authority and power in the family and may encompass factors such as roles. Finally, the maintenance system, which is not examined in the current study, is related to a family’s ability to protect one another and have access to basic needs (Henry et al., 2015). These FAS modulate a family’s response to a stressor and therefore, have a downstream impact on protective factors, vulnerability factors, and subsequent adaptation to that stressor (Harrist et al., 2019).
Aim 1 of the current study was to conduct a factor analysis of the family protective, vulnerability, and adaptation domains to determine whether FAS within each of these domains would form a unified latent representation. Prior research has examined factor analyses of family resilience using the Walsh framework, which posits three dimensions of family resilience: family belief systems, family organization, and communication/problem solving processes (Walsh, 2016). There is evidence that these domains form independent scales with moderate to high correlations (e.g., rs 0.49-0.82; Rocchi et al., 2017). To the best of our knowledge, prior research has not tested a factor analysis of these domains, but FAS are conceptualized to be related but separate processes (Harrist et al., 2019; Henry et al., 2015). Given the paucity of research, no hypothesis was made as to whether each of these domains would be best represented by a single latent factor.
Family Resilience Model During the COVID-19 Pandemic
From a family resilience perspective, the COVID-19 pandemic required responses from the family system as roles, expectations, and relationships changed for all family members (Henry et al., 2015). Therefore, the second aim of the current study was to examine a model of family adaptation in response to COVID-19 stressors that concurrently considered multiple protective and vulnerability factors impacted by the pandemic, as well as pre-existing health factors (see Fig. 1). Congruent with the FRM, we examined these factors across multiple levels of analysis including individual family member factors (e.g., child and parent COVID stress) and family level factors (e.g., making meaning, family emotional support), which is a strength. However, it should be noted that one parent provided the report for all variables and therefore, the results reflect one caregiver’s perspective on the family unit, including the target child’s behavior. This caregiver’s perspective is also influenced by the family situational meaning (i.e., “perceptions of specific situations, involving family worldviews and identities,” p. 35) which arises jointly within all aspects of the FRM in the presence of a stressor (Henry et al., 2015). The COVID-19 pandemic elicited many facets of situational meaning across a number of domains. For example, identifying more strongly with one’s family during the pandemic was related to lower levels of stress and physical symptoms (Frenzel et al., 2022), indicating that a family’s cohesiveness informs how threatening they perceive the pandemic to be.
Conceptual Family Resilience Model. Note. Pre-existing vulnerabilities is defined by parent and child past mental health, parent and child COVID-19 physical health conditions, and the presence of a child trauma history. Covariance paths between COVID-19 related stressors, parent racial diversity status, and pre-existing vulnerabilities and family protective factors and family vulnerability factors were included but are not shown for ease of interpretation
Family protective factors were income during the pandemic, marriage status during the pandemic, and having children who experienced all in person schooling instead of combined or exclusive virtual learning. All of these factors are related to the maintenance system and reflect stability or changes in routines at the onset of COVID pandemic which likely had cascading effects to other FAS (Harrist et al., 2019). Recent research has demonstrated that financial stress, not being married, and online schooling demands are all related to increased stress or decreased mental health among adults during the COVID-19 pandemic (Adams et al., 2021; Jace & Makridis, 2020; Park et al., 2020). It was hypothesized that higher levels of COVID-19 stressors would be associated with lower levels of COVID-19 protective factors (e.g., lower income, not being married, virtual learning) which would subsequently be associated with lower levels of family adaptation, as defined in Aim 1.
Family vulnerability during the pandemic was evaluated with measures of child and parent COVID-19 acute stress symptoms and emotional impact and therefore, are most closely aligned with the emotion system of the FRM. Recent work that has found that COVID-19 stressors are associated with stress and mental health struggles in other domains (Brown et al., 2020). Similarly, stress experienced by parents relates to lower levels of family functioning in pediatric populations (Streisand et al., 2003) and in urban families (Sheidow et al., 2014). Accordingly, it was hypothesized that parent and child emotional vulnerability would predict lower levels of family adaptation.
COVID-19 Stressors
COVID-19 stressors refer to the stressful events that families may have experienced related to the pandemic, including COVID-19 illnesses, hospitalizations and deaths, as well as the impact of COVID-19 on disruptions in a family’s life (e.g., employment, child care; Kazak et al., 2021). Given the saliency of the COVID-19 pandemic and significant levels of stressors (Calvano et al., 202; Prime et al., 2020; Taubman-Ben-Ari et al., 2021), it was expected that COVID-19 stressors would be associated with family factors over and above these pre-existing health vulnerabilities. A previous study reported that on average families experienced approximately nine events or impacts related to COVID-19 (Kazak et al., 2021). In the current study, greater exposure to COVID-19 stressors were hypothesized to be related to fewer current family protective factors, greater emotional vulnerability, and less family adaptation. Additionally, consistent with a family model of risk and resilience (e.g., Prime et al., 2020), it was hypothesized that there would be an interaction between COVID-19 stressors and pre-existing health vulnerabilities in paths between family protective factors, family vulnerability factors, and family adaptation. These interaction analyses are included in the supplementary material.
Pre-Existing Family Health Vulnerabilities
Researchers have theorized that even when COVID-19 stressors are equal, some families may have had a harder time adapting to the stressors of the pandemic (Prime et al., 2020). In terms of the FRM, pre-existing health vulnerabilities may have impacted COVID-19 vulnerability and protective factors, as well as overall family adaption across the pandemic. Specifically, some families may be more vulnerable than others due to pre-pandemic factors, such as parent and child mental and physical health needs, and a history of trauma (Prime et al., 2020). Pre-pandemic parent and child mental health may also contribute to COVID-19 family adaptation (Fosco et al., 2022). With mental health concerns increasing during the pandemic in general (Pierce et al., 2020), families with higher initial levels of mental health concerns may be at a greater risk (Yang et al., 2020). Collectively, these pre-pandemic stressors may create a context leading to increased family vulnerabilities and decreased protective factors, which in turn may decrease overall family adaptation. Consequently, it was hypothesized that greater levels of pre-existing family health vulnerabilities would be associated with lower levels of family protective factors, higher levels of family vulnerability factors, and lower levels of family adaptation.
Another factor posited to be particularly relevant in relation to family resilience during the COVID-19 pandemic is race (Prime et al., 2020). Racial health disparities are present across numerous health outcomes, with various systemic issues influencing access to healthcare for racially diverse populations (Hammonds & Reverby, 2019). During the pandemic, racially diverse groups experienced disproportionate physical harm from COVID-19 relative to White individuals (Lopez et al., 2021) and more negative financial and mental health outcomes due to the COVID-19 pandemic (Fortuna et al., 2020; Trammell et al., 2023). Consequently, it was hypothesized that racially diverse parents may endorse fewer current protective factors, greater emotional vulnerability factors, and less family adaption given the myriad of systemic and cultural barriers that families of color face.
Moderators of Family Resilience
The FRM also posits that resilience is family specific (Henry et al., 2015), and therefore our third aim was to test moderators of the family resilience model tested in Aim 2. Vaccine status was tested as a moderator of the model given that vaccination status has implications for the impact of COVID-19 factors on the family system. Being vaccinated may mitigate the impact of vulnerability factors and increase the role of protective factors on family adaptation (e.g., allay concern over physical health risks; permit return to social activity). Based on the novelty of the literature, no hypothesis was made at this time.
Parent gender was also examined as a moderator of the model. Historically, fathers’ participation in pediatric or family psychology research has been lower than mothers’ participation (Davison et al., 2017) and there have been calls for more inclusion of fathers in psychology outcome research (Fabiano & Caserta, 2018). Emerging research suggests that mothers experienced higher general stress than fathers during the pandemic (Calvano et al., 2021). Further, the pandemic has increased the amount of unpaid care work (e.g., childcare, elder care), which is often covered by women, many of whom are mothers (Power, 2020). However, other researchers have found that fathers but not mothers experienced a higher level of parenting stress during the pandemic compared to a year prior (Taubman-Ben-Ari et al., 2021) and that fathers of older infants may be particularly at risk for COVID-19 related anxieties (Ben-Yaakov and Taubman-Ben-Ari, 2021). Based on this mixed evidence, no hypothesis was made.
Current Study
The COVID-19 pandemic offers a unique opportunity for researchers to study how families adapt to high levels of adversity that affect almost every domain of a family’s life. Identifying ways in which families draw on natural sources of resilience can help inform intervention efforts for future family disruptions (e.g., trauma, deaths, natural disasters). Therefore, the current study systematically tested a model of family resilience during the COVID-19 pandemic. The three aims included: determining whether the meaning, control, and emotion systems are best represented as single or multiple indicators of family adaptation (Aim 1); testing the aforementioned concurrent model of family resilience (e.g., Henry et al., 2015; Aim 2), and examining whether parent gender and parent vaccine status moderate associations within the family resilience model (Aim 3).
Method
Participants and Procedure
Recruitment and data collection of a nationally representative sample of the U.S. adult parent population was completed through the survey company Qualtrics. Parents (N = 796) participated as part of a study on parenting and family mental health during COVID-19. Nonprobability quota sampling was used to ensure that the sample distribution maintained known U.S. population parameters for parent race/ethnicity, household income, and regional distribution (auto-assigned to West, Midwest, South, or Northeast regions based on state), and to reflect equal participation of mothers and fathers and equal distribution across three child age groups (5- 8-year-olds, 9–12-year-olds, 13–16-year-olds). Online data collection took place between February 2nd and April 4th, 2021. This time frame is particularly useful for studying family resilience because pandemic risk was still prevalent but by this phase of the pandemic families also had time to utilize their protective resources. Specifically, families had a year to adapt to the COVID-19 pandemic and make use of resources already in place or develop new resources and the vaccine was a new resource that families could capitalize on.
Inclusion criteria for parents were >18 years old, having at least one child between 5–16- years-old, and living with the child >75% of the time. Parents were invited by Qualtrics via email to participate. If inclusion criteria were met, electronic consent was obtained prior to continuing. Parents answered survey questions about only one child, who was randomly selected if parents had multiple eligible children. Parents were excluded if they completed the survey in less than one-half the median time, did not complete the entire survey, showed inconsistent responding, or failed three quality check questions. Of 2754 invitations sent, 397 did not meet inclusion criteria, 83 did not complete screening questions, and 67 did not consent. Of 2207 individuals who consented, 1411 were excluded based on exclusion criteria, resulting in 796 in the final sample. See Penner et al., 2022 for more details on recruitment.
Median completion time for the final sample was 26.71 min. This study was carried out in accordance with the Declaration of Helsinki and approved by the university Institutional Review Board. Parents included fathers (51.8%) and mothers (48.2%) whose age ranged from 18–75 years (M(SD) = 38.87(8.96). Average child age was 10.35 (SD = 3.16). The sample was predominantly Non-Hispanic White (60.3% Non-Hispanic White, 18.1% Hispanic/Latinx, 13.2% Non-Hispanic Black/African American, 5.7% Asian, and 2.8% Other Race) and from the Southern area of the U.S. (39.9% South, 21.7% West, 19.3% Northeast, 19.0% Midwest).
Measures
Pre-COVID Family Health Vulnerabilities
Five dichotomous variables were summed across family vulnerabilities to create an overall Pre-COVID family vulnerability composite with higher scores indicating greater vulnerability.
Pre-existing Child and Parent Psychiatric Conditions
Parents reported whether they or their child have ever had the following psychiatric conditions: Neurodevelopmental Disorder, Behavioral Disorder, Emotional Disorder, Serious Mental Illness, and Substance or Alcohol Use Disorder (assessed for parents only). This was dichotomized into two variables to reflect either the presence (1) or absence (0) of one or more conditions for parents and children.
Pre-existing Child and Parent Physical Health Conditions
Parents reported whether they or their child had the following CDC-defined underlying health conditions that increase COVID-19 risk: Cancer, Chronic Kidney Disease, Chronic Obstructive Pulmonary Disease, Heart condition, Obesity, Sickle Cell Disease, Smoking, Type 2 Diabetes. These variables were dichotomized to reflect either the presence (1) or absence (0) of one or more risk conditions for parents and children.
Child History of Trauma
476 (59.8%) parents endorsed that their child has never experienced any type of trauma (e.g., child abuse, parent separation) with 320 (40.2%) parents endorsing a 1 to 10 on the Adverse Childhood Experiences Questionnaire (Felitti et al., 1998). This variable was dichotomized to reflect the presence (1) or absence (0) of trauma.
Racial Diversity Status
Parents self-reported their own race and ethnicity. This variable was dichotomized to reflect whether a parent was a Racially Diverse (1) or White (−1). This coding scheme was chosen to facilitate the probing of interactions, which are included in the supplementary materials.
COVID-19 Stressors
COVID-19 Exposure and Family Impact Survey (CEFIS)
The CEFIS is a caregiver report measure that was designed to examine both exposure and impact of the COVID-19 virus on families (Kazak et al., 2021). The current study used the 25-item Exposure scale, which includes items such as, “We had a stay-at-home order,” “We were unable to visit or care for a family member,” “We had difficulty getting food,” and “A member of our family lost their job permanently.” In addition, the measure asks whether any family members were (1) exposed to COVID-19, (2) had symptoms or were diagnosed with COVID-19, (3) were admitted to the Intensive Care Unit, or (4) died due to COVID-19. These items are coded Yes (1) or No (0) scale and summed to get an overall exposure score. The reliability was acceptable in the current sample (Cronbach’s α = 0.85).
Family Vulnerability Factors
Parent COVID-19 Stress
Parental acute stress symptoms related to COVID-19 were measured using nine items from the NIH Environmental influences on Child Health Outcomes (ECHO) COVID-19 questionnaire (Margolis et al., 2021). The nine items reflect the acute stress symptoms from the DSM-5, but are asked in the context of COVID-19. Item response categories range from 1 (not at all) to 5 (very often) and were summed for a total COVID-19 acute stress score. Higher scores on measures reflect greater mental health problems. The scale was reliable in this sample (α = 0.90)
Child COVID-19 Stress
Parents also completed the COVID-19 acute stress items from a parent-report child version of the ECHO COVID-19 questionnaire. The child set includes an extra question assessing whether the child had begun to behave in ways he/she had outgrown. The 10 item scores were summed for a total child COVID-19 acute stress score (α = 0.93).
CAIR-Pandemic Impact Questionnaire- Child
Parents completed the impact items from a parent-report version of the CAIR Pandemic Impact Questionnaire (Lang, 2020). The questionnaire assesses the emotional impact of the COVID-19 pandemic on their child. There are 5 questions (e.g., “How much does your child worry about your health or the health of family and friends,” “How much is your child reading, watching/listening, talking or thinking about coronavirus/COVID-19”) rated 1 (not at all) to 5 (extremely). Higher scores reflect greater impact. The scale was reliable in this sample (α = 0.86).
CAIR-Pandemic Impact Questionnaire- Parent
Parents completed the same CAIR- pandemic questionnaire that assessed their self-report of the emotion impact of the COVID-19 pandemic. The measure was reliable in this sample (α= 0.82).
COVID-19 Family Protective Factors
Income
Parents self-reported on their household income based on four categories. The majority of the sample had an income less than $50,000 (36.9%), followed by $50,000 to $99,999 (35.6%), $100,000 to $149,999 (15.1%), and $150,000 or more (12.4%).
School Format
Parents self-reported their child’s school format with 172 children attending school in person (21.6%), 209 using a hybrid format (26.3%), and 396 attending school in a completely virtual format (49.7%). Nineteen parents stated that this question was not applicable (2.4%). This variable was coded into one variable reflecting in person (0) or hybrid model and fully virtual (1) schooling, consistent with prior researching showing that children and parents who have children engaged in any form of virtual learning are at higher risk for negative outcomes (Verlenden et al. 2021).
Marriage status
Parents self-reported their own current marriage status. 586 participants were married (73.6%). Of those who were not married, 128 had never been married (16.1%), 11 were separated (1.4%), 60 were divorced (7.5%), and 11 were widowed (1.4%). This variable was dichotomized into a variable to represent not married (0) and married (1).
Family Adaptation
Stability in Routines
Parents completed the Child Routines Inventory (Sytsma et al., 2001). Parents were asked to rate how often their child engaged in each routine over the past month on a five-point Likert scale rated 1 (Never) to 5 (Nearly always). Items include routines such as, “My child takes turns with family members talking about their day” and “My child has a set routine for getting ready in the morning.” Items were summed and higher scores reflect greater adherence to routines. The scale was reliable in this sample (α = 0.88).
Family Making Meaning
Parents were asked “How much has your family been trying to find meaning from the COVID-19 pandemic?” on a five-point scale rated 1 (None at all) to 5 (A great deal; Park et al., 2008). Higher scores indicate more making meaning.
Family Emotional Support
Parents completed a short version of the McMaster Family Assessment Device (Boterhoven et al., 2015). The six items reflect emotional functioning, and asks parents to rate how they see their family with example items including “In times of crisis we can turn to each other for support,” “Individuals are accepted for what they are,” “We can express feelings to each other,” and “We confide in each other.” Items were rated on a four-point scale ranging from 1 (Strongly agree) to 4 (Strongly disagree) and then reverse coded and averaged so that higher values reflect higher levels of emotional support (α = 0.84).
Moderators
Vaccination Status
Parents were asked if they had received 0, 1, or 2 doses of a COVID-19 vaccine. Those having received 1 or 2 doses were collapsed into a “vaccinated” group (1) represented by 233 parents (29.3%) relative to an “unvaccinated” group (0) represented by 563 parents (70.7%). Based on vaccine allocation data from the CDC, by the end of the data collection period, allocations of the Janssen/Johnson & Johnson vaccine in all U.S. jurisdictions were approximately 10% of the combined allocations of Pfizer and Moderna vaccines (CDC, 2021). Therefore, it is likely that most of the parents in this sample who reported vaccination had received either Pfizer or Moderna. The percentage of U.S. adults having received one vaccination during this period ranged from 12.2% on February 7th to 30.7% on April 4th, 2021 (White House COVID-19 Team, 2021a, 2021b).
Parent Gender
Parents self-reported their own gender.
Data Analysis
Outliers were modified by adjusting the value to +/- three standard deviations from the mean, For key study variables, skew (−0.62 to 0.73) and kurtosis (−1.09 to −0.02) values were slightly skewed but within accepted ranges for normally distributed variables (Kline, 2016).
All analyses were estimated in Mplus version 8.6 (Muthén and Muthén 1998–2021). The weighted least squares mean and variance (WLSMV) estimator was used for analyses where there were continuous and categorical variables and the Maximum Likelihood with Robust Standard Errors (MLR) estimator was used for analyses with all continuous variables. The appropriate difference test was used based on the estimator (e.g., Difftest function in Mplus for WSLMV model comparisons). There was no missing data for any variable with the exception of school format (2.4% missing data) which was accommodated by using full information maximum likelihood (FIML).
Data analysis proceeded in a sequential fashion. First, a measurement model was examined to test whether factors for the family adaptation, family vulnerability and family protective constructs could be estimated to each represent their hypothesized single latent construct. In the event that model fit was poor or that factor loadings were less than 0.30 for a given factor, then a single latent factor was abandoned and correlated manifest variables were used instead.
Next, three structural models were examined. In the first model, family adaptation was regressed on the family protective and family vulnerability factors, pre-existing family health vulnerabilities and parent racial diversity status. The family protective and family vulnerability factors were regressed on pre-existing family health vulnerabilities and parent racial diversity status. In this initial model, the COVID-19 stressors variable was included in the model as a correlate of pre-existing conditions and racial diversity status but all paths between COVID-19 stressors and the family protective, vulnerability, and family adaption variables were constrained to zero. In the second model, these paths were freed and a χ2 difference test informed whether this resulted in improvement model fit. Pre-existing family health vulnerabilities, COVID-19 stressors, parent racial diversity status, and the family protection and vulnerability factors were regressed on covariates (i.e., parent age, parent vaccination status, and parent gender) in all models.
Prior to testing moderation of the structural paths, the measurement invariance of the measurement model was tested across parent gender and vaccine status to ensure that the parameters were similar across groups. To test the measurement invariance, two models were run: (1) a configural model where all loadings, intercepts/thresholds, and residual variances were freed across gender and (2) a metric model, where factor loadings were constrained to equivalence across gender but intercepts/thresholds and residual variances were free to vary. Model comparisons were tested using the appropriate statistical test.
Finally, multiple group analyses were used to test if hypothesized structural paths from the final resilience model varied by vaccine status. First, a model was tested where all hypothesized regression paths varied by vaccine status. Second, a model was tested in which the regression paths were constrained to equivalence across vaccine status. The same process was used to test moderation by parent gender. If there was a significant difference, modification indices were used to determine which parameters should be sequentially freed. A likelihood ratio χ2 test was used to test overall model fit where p > 0.05 indicates good model fit. The following alternative fit indices were also considered: (a) comparative fit index (CFI), where values greater than 0.95 suggest good fit, (b) standardized root mean-square residual (SRMR) where values less than 0.08 represent mediocre fit, and values less than 0.05 indicate close fit and (c) root mean square error of approximation (RMSEA), where values less than 0.08 suggest mediocre fit, and values less than 0.05 indicate close fit (Hu & Bentler, 1999).
Data from this study are available in the Open Science Framework (Perry et al., 2021) to facilitate peer review and analytic code is available upon request. The authors have no relevant financial or non-financial interests to disclose.
Results
Preliminary and Factor Analyses
Bivariate correlations and descriptive statistics are provided in Table 1. First, a confirmatory factor analysis was examined testing the three latent factors of family adaptation, family protection, and family vulnerability with correlations among the three factors. The model provided a poor fit to the data [χ2 (32) = 534.69, p < 0.001, CFI = 0.59, RMSEA = 0.14, SRMR = 0.12] and the factor loading for family meaning was very low (0.16; p < 0.001). Therefore, a model was tested where the family adaptation indicators (i.e., making meaning, family functioning, and routines) were entered as manifest variables and allowed to correlate with one another and the family protective and vulnerability latent factors. This model provided an acceptable fit to the data [χ2 (28) = 119.90, p < 0.001, CFI = 0.93, RMSEA = 0.06, SRMR = 0.05]. See Table 2 and Table 3 for factor loading values and correlations. Notably, a child being in some form of virtual schooling (i.e., hybrid or fully virtual schooling) rather than in person schooling was related to higher levels of the family protection factor, contrary to the theoretical conceptualization. Higher levels of the family protective factor were indicated by families with a higher income, being married, and having a child that was not attending school fully in person. The family emotional vulnerability factor was represented by higher levels of child and parent acute COVID stress and emotional impact. A positive correlation between the family emotional vulnerability and the family protective factor was observed, suggesting that during the COVID-19 family demographic protective factors may still be positively associated with parents reporting more emotional vulnerability factors.
Structural Model in the Entire Sample
Next, sequential structural models were examined. First, a model with COVID-19 protective and vulnerability factors, pre-existing variables, racial diversity status, and covariates was constructed to predict the family adaptation variables. The COVID-19 stressors was included in the model, but all paths between COVID-19 stressors and the family protective, vulnerability, and family adaption variables were constrained to zero. The model provided a poor fit to the data [χ2 (72) = 307.66, p < 0.001, CFI = 0.88, RMSEA = 0.06, SRMR = 0.09].
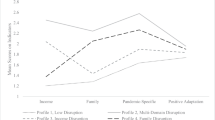
Next, paths from COVID-19 stressors to the family protective and family vulnerability factors and the family adaptation variables were added. This model provided an acceptable fit to the data [χ2 (67) = 202.00, p < 0.001, CFI = 0.93, RMSEA = 0.05, SRMR = 0.05; See Fig. 2] and a significantly better fit than the previous model [Δχ2 (5) = 134.86, p < 0.001], suggesting that COVID-19 stressors significantly impacted pandemic family protective, vulnerability, and adaptation variables over and above existing family health vulnerabilities and racial diversity status. There were direct associations from pre-existing family health vulnerabilities to stability in routines (β = −0.23, p < 0.001) and family emotional support (β = −0.14, p = 0.002), from COVID-19 stressors to family emotional support (β = 0.11, p = 0.048), and from racial diversity status to making meaning (β = 0.10, p = 0.02). There were also associations from pre-existing family health vulnerabilities to the current family protective (β = −0.12, p = 0.03) and family emotional vulnerability (β = 0.19, p < 0.001) factors and from COVID-19 stressors to the family emotional vulnerability factor (β = 0.55, p < 0.001). In turn, the current family protective factor was positively related to family emotional support (β = 0.15, p = 0.003) and making meaning (β = 0.18, p < 0.001) and the family emotional vulnerability factor was positively related to making meaning (β = 0.48, p < 0.001).
Concurrent Family Resilience Structural Model. Note. *p < 0.05, **p < 0.01. The covariance between family vulnerabilities and family protective factors and family vulnerability factors was estimated but is not shown. Pre-existing family health vulnerabilities is defined by parent and child past mental health, parent and child COVID-19 physical health conditions, and the presence of a child trauma history. The family vulnerability and protective latent factors and the COVID stressors, pre-existing health vulnerabilities, and parent racial diversity variables were regressed on the covariates (i.e., parent gender, parent vaccination status, and parent age)
Parent Gender and Vaccination Status Moderation
Parent Gender
Measurement invariance of the two-factor family protective and vulnerability measurement model was tested across gender. No difference in model fit was found for the configural and metric invariance models [Δχ2(5) = 6.28, p = 0.28; see supplementary materials].
Next, the equivalence of the structural paths was tested across parent gender. First, a model was tested where all of the structural paths were freed across parent gender. The model would not converge. When the paths from the covariates to racial diversity status, COVID-19 stressors, and pre-existing family health vulnerabilities were removed, the model did converge. This model provided a poor to acceptable fit to the data [χ2 (125) = 324.41, p < 0.001, CFI = 0.89, RMSEA = 0.06, SRMR = 0.08]. A model was then tested where all of the key structural paths were constrained across parent gender. This model provided an acceptable fit to the data [χ2 (146) = 326.42, p < 0.001, CFI = 0.90, RMSEA = 0.06, SRMR = 0.08] but there was a marginally significant difference in model fit between the two models [Δχ2 (21) = 32.42, p = 0.05].
Given this marginal difference in model fit and the less-than-ideal model fit, modification indices (MI) were examined to see if any specific paths would meaningfully and theoretically contribute to improvement in model fit. The MI for the paths from racial diversity status to the current family protective factor (MI = 17.04) and the family emotional vulnerability factor (MI = 16.29) were substantial. Freeing the path from racial diversity status to the current family protective factor provided an acceptable fit to the data [χ2 (145) = 315.35, p < 0.001, CFI = 0.91, RMSEA = 0.05, SRMR = 0.08] and a significantly better fit than the constrained model [Δχ2 (1) = 6.48, p = 0.01]. In this model, the MI for the path from racial diversity status to the family emotional vulnerability factor remained substantial (MI = 15.62). A model with the paths from racial diversity status to the family protective and vulnerability factors freed provided an acceptable fit to the data [χ2 (144) = 301.68, p < 0.001, CFI = 0.92, RMSEA = 0.05, SRMR = 0.08] and a significantly better fit than the previous model [Δχ2 (1) = 10.68, p = 0.001]. Additionally, there was no difference in model fit with the free to vary model [Δχ2 (19) = 13.78, p = 0.80].
In this final model, racially diverse fathers self-reported fewer current family protective factors (β = −0.22, p = 0.002) but also less family emotional vulnerability (β = −0.11, p = 0.006) than White fathers. For mothers, there was no difference in self-reported current family protective factors (β = 0.07, p = 0.37) or family emotional vulnerability (β = 0.03, p = 0.51) by racial diversity status. When interpreting these results caution is warranted given that the original difference in model fit between the constrained and the free to vary model was marginal.
Parent Vaccination Status
The measurement invariance of the two-factor family protective and vulnerability measurement model was tested across parent vaccination status. There was no difference in model fit between configural and metric models [Δχ2(5) = 6.98, p = 0.22, See supplementary materials].
Next, the equivalence of the structural paths across parent vaccination status was tested. First, a model was tested where all of the structural paths were freed across parent vaccination status. The model would not converge. Like the models above, the model converged when removing paths from the covariates to racial diversity, COVID stressors, and pre-existing health vulnerabilities.
This model provided a poor to acceptable fit to the data [χ2 (125) = 330.09, p < 0.001, CFI = 0.89, RMSEA = 0.06, SRMR = 0.11]. A model was then tested where all of the structural paths were constrained across parent vaccination status. This model provided a poor to acceptable fit to the data [χ2 (146) = 335.88, p < 0.001, CFI = 0.90, RMSEA = 0.06, SRMR = 0.12] and was a significantly worse fit than the free to vary model [Δχ2 (21) = 35.23, p = 0.03]. Modification indices were examined and the path from pre-existing family health vulnerabilities to family protective factors had the highest MI (MI = 8.03). The model with this path freed across vaccination status provided a poor to acceptable fit to the data [χ2 (145) = 319.07, p < 0.001, CFI = 0.91, RMSEA = 0.06, SRMR = 0.11] and no difference in model fit with the free to vary model [Δχ2 (20) = 24.03, p = 0.24]. For parents who were not vaccinated, there was a negative relation between pre-existing family health vulnerabilities and the current family protective factor (β = −0.23, p = 0.001). For parents who were vaccinated, there was no relation between pre-existing family health vulnerabilities and the current family protective factor (β = 0.23, p = 0.12). Given that SRMR was less than ideal, we tested a model with family protective and vulnerability factor scores and with all covariate paths included which replicated the moderation finding across vaccination status (See supplementary materials).
Discussion
The current study rigorously examined a concurrent model of family resilience in the context of the COVID-19 pandemic across three aims that included testing a unitary latent representation of family adaption, evaluated a formal model of family resilience during COVID-19 (Henry et al., 2015), and examined whether parent gender and vaccination moderated these associations. Data collection occurred between February 2nd and April 4th, 2021, which is a particularly useful time for studying resilience to the pandemic as families had time to utilize old and new resources allowing for a thorough test of pandemic resilience. Moreover, at this time vaccine availability was being offered which gave families a new resource to capitalize on. Overall, results underscore the utility of the Family Resilience Model (FRM; Henry et al., 2015) to contextualize family resilience during a stressful, global event with far reaching impact.
Unity of Family Adaptation, Protective, and Vulnerability Factors
The FRM proposes that the FAS (i.e., meaning, control, maintenance, and emotion systems) as indicators of a family protection, vulnerability, and adaptation factors. Results demonstrated that the family adaptation indicators did not represent a single factor composed of making meaning during the pandemic, family emotional support, and a family’s adherence to routines, respectively. Rather, results indicated that these are each unique but correlated family resilience characteristics, congruent with the conceptualization that the FAS domains are interrelated but separate (Harrist et al., 2019; Henry et al., 2015). The family protection variables and the family vulnerability variables each loaded on one factor, providing conceptual support for their representation of the family maintenance system and emotional system, respectively.
In regards to current family protection, higher family income, being married, and some form of virtual schooling for children (i.e., hybrid or fully virtual schooling) were related to higher family protection levels. Contrary to hypotheses and prior research (Adams et al., 2021; Freisthler et al., 2021; Verlenden et al., 2021) our results suggest that virtual learning was associated with caregivers with more resources (i.e., greater household income, two-parent household). Indeed, some research has shown that parents whose children are engaged in remote learning experienced less family safety stress than parents whose children were engaged in in-person learning (Sampige et al., 2021). Additionally, higher income and White parents endorsed greater stress about home structure during the pandemic (Yung-Chi Chen et al., 2021). Therefore, parents of children engaged in virtual schooling may have more stress related to parenting but less stress related to their children’s safety. This is congruent with our initially surprising finding that there was a positive correlation between the family emotional vulnerability factor and the current family protection factor. Parents with more resources may experience more long-term logistical changes in their everyday lives (e.g., transition to work from home) but have the ability to make these changes, and in turn, may experience less stress about their children’s safety.
Testing the Family Resilience Model
Pre-existing Family Health Vulnerabilities
Pre-existing family health vulnerabilities, defined by caregiver and child physical and mental health and previous child exposure to trauma, emerged as the greatest risk factor for a number of outcomes even when controlling for COVID-19 stressors. Specifically, this risk was directly associated with reduced family emotional support and less stability in routines during the pandemic. Pre-existing family health vulnerabilities were also concurrently related to fewer demographic resources during the pandemic and greater family COVID emotional vulnerability, which in turn were associated with higher levels family emotional support. These findings are congruent with the FRM (Henry et al., 2015), theoretical models of family functioning during the pandemic (i.e., Prime et al., 2020) and with recent research demonstrating that the presence of caregiver or child pre-pandemic mental health (Fosco et al., 2022) may exacerbate the impact of the pandemic on individual well-being. This study extends these findings by also showing that parent and child pre-existing family health vulnerabilities are associated with aspects of reduced overall family emotional well-being. Pre-existing family health vulnerabilities were also associated with fewer current protective factors, a likely bidirectional relationship given that factors, such as income, both predict and reflect poorer physical and mental health (Mullahy et al., 2011). Situational meaning and all factors of the FRM develop simultaneously (Henry et al., 2015) and therefore, parents who have a pre-existing health vulnerability or have a child with a vulnerability may be at risk for particularly negative or threat based situational response to the pandemic leading to lower levels of perceived protective factors.
We observed that parent vaccination status moderated the relation between pre-existing family health vulnerabilities and current family protection features. Unvaccinated parents who had more pre-existing family health vulnerabilities reported fewer current family protective resources. Conversely, there was no relation among vaccinated parents. Importantly, data collection took place relatively early in the vaccination process [i.e., between February 2nd and April 4th, 2021; U.S. national rates for one or more doses were 12.2% on February 7th to 30.7% on April 4th, 2021 (White House COVID-19 Team, 2021a, 2021b)]. At that time, parents with pre-existing family health vulnerabilities were eligible for the COVID-19 vaccine in many parts of the United States. When families with pre-existing family health vulnerabilities received the vaccine their family situational meaning of the pandemic may have become more positive leading to more perceived protective factors. Conversely, their counterparts who were not vaccinated likely experienced no change in their situational meaning of the pandemic, and therefore, still reported fewer perceived protective factors. It should also be noted that families with more demographic resources likely had greater access to the vaccine, a finding commonly observed in access to health care in general (Dubay & Lebrun, 2012), pointing to the importance of including factors related to the broader ecosystem congruent with the FRM (Henry et al., 2015). More specifically, in low resource U.S. communities, fewer adults received the COVID-19 vaccine within the first 2.5 months of vaccine distribution (Hughes et al., 2021). Current results fit with these findings and suggest that extra resources may be needed to ensure equitable vaccine access for families with fewer resources.
Parent Racial Diversity Status
Parent racial diversity status was also examined as a predictor of family resilience given research linking racially diverse populations to increased risk for negative physical health, mental health, and financial outcomes during the pandemic (Fortuna et al., 2020; Lopez et al., 2021; Trammell et al., 2023). Interestingly, racially diverse parents in this sample reported making more meaning during the pandemic relative to White parents. Prior research has found that individuals use different coping skills based on their racial and ethnic background. For example, Black Americans and Mexican citizens living in America are more likely to use religious-based coping strategies (Farley et al., 2005; Oates et al., 2013), although it should be noted that within these racial and ethnic groups, there is substantial variability coping techniques (Brenner et al., 2018). It is possible that the current findings regarding making meaning reflect parents’ helping their family cope with the stress of the pandemic. A key tenet of the FRM is one of individual resilience, or “protective variables in one circumstance may be risks or vulnerabilities in other circumstances” (Henry et al., 2015, p. 30). The relation between race and family adaptation is complex and broader systemic racism and intersectionality likely play roles too (Williams, 2018); these were not examined in the current study. Paths from parent racial diversity status to family protective factors and family COVID vulnerability factors were moderated by parent gender such that fathers who are racially diverse reported fewer current protective factors and fewer emotional vulnerability factors relative to White fathers. There was no difference in the amount of vulnerability and protective factors reported for racially diverse and White mothers. However, caution is warranted when interpreting these results given that the original difference in model fit was only marginal.
COVID-19 Stressors
Adding in concurrent paths from COVID-19 stressors to pandemic family protective, vulnerability, and adaptation variables significantly improved model fit over and above pre-existing family health vulnerabilities and racial diversity status. Specifically, congruent with hypotheses, COVID-19 stressors were positively associated with family COVID emotional vulnerability (COVID-19 emotional impact, COVID-19 acute stress). Contrary to hypotheses, higher levels of COVID-19 stressors were related to higher levels of family emotional support, suggesting that families are showing resilience in the face of an enormous stressor. Remarkably, prior work has found that in an adult Italian sample, 70% of individuals demonstrated resilience during the pandemic (Panzeri et al., 2021). As stated above, in the FRM a protective factor in one context may be a risk factor in another context (Henry et al., 2015). Emotional vulnerability during the COVID-19 pandemic may be related to higher levels of family emotional support, but in the context of other stressors or when examining other outcomes, emotional vulnerability may be a risk factor. For example, COVID-19 exposure and stress are associated with higher levels of individual anxiety (Gallagher et al., 2020). When considering other acute stressors, after a natural disaster bereaved parents who reported more emotional loneliness also reported reduced levels of family function, cohesion, and adaptability (Cao et al., 2013), suggesting that the protective effect of emotional vulnerability is not generalizable to all stressors. The COVID-19 pandemic is unique given that every parent in the world has been impacted by COVID-19. Statistically, we also partialled out the impact of pre-existing family health vulnerabilities which was moderately correlated with COVID-19 stressors and therefore, in this model COVID-19 stressors likely represents individuals who have exposure in the absence of other risk factors which may be indicative of a higher resource group.
Limitations and Future Directions
Despite several strengths of the study including the use of a nationally representative sample, strength-based theoretical approach, and rigorous quantitative approach, there are several limitations that should be noted. First, this data is cross-sectional and therefore, there are multiple alternative models that could be tested. The goal of the current study was to provide an initial and rigorous test of the family resilience model during the COVID-19 pandemic and therefore, the model was used to guide the direction of associations. Future research should evaluate whether these relations are present across time. Additionally, due to the cross-sectional nature of the data, indirect effects were not formally tested. A longitudinal model should formally test indirect effects.
Second, in terms of measurement, we measured several facets of family adaptation, but we only had one measure of the meaning, control, and emotion systems. Family making meaning was also assessed using one item, which is a significant limitation. Future research should include several different measures of the various systems across all aspects of the model (Henry et al., 2016). Additionally, there are several measures that have been created to specifically address specific facets of family resilience, such as the, Family Time and Routine Index (McCubbin et al., 1986) which can be used to more thoroughly asses the FRM (for a review, see Harrist et al., 2019) in future research. Regarding the current family protection latent variable, COVID family income and marriage status are generally stable in nature and therefore, may be more representative of protective factors before the pandemic. However, these variables were included in this part of the model because of their relevance to each other and school status, as evidenced by their formation as one latent factor and the FRM model’s conceptualization that protective factors follow family risk (e.g., can be activated under stress). It is critical that future research uses longitudinal data to track family income and marriage status as potential protective factors both pre and post pandemic to tease out the timing of these protective effects.
Multiple levels of influence were included in the study and provided information on the individual parent, individual child, and overall family system levels of influence. However, one limitation of using this multilevel approach is that were not able to determine which level of predictors were primarily driving effects. We were also unable to include information about sibling or parent-child relationships. Future research should use a broad systems level approach to evaluate the utility of the FRM as a theoretical model and an individual predictor approach to isolate which factors are most relevant for family functioning. Finally, one parent provided their report for all variables in the study, which likely increased the size of the associations and provides only one perspective on the family unit; therefore, future research should use multiple informants to further validate the model.
Third, the current research examined the role of parent racial diversity status in concurrent predictions of family resilience and how this intersects with other identities, such as parent gender, in predicting these outcomes, which is a strength. However, racially diverse parents were grouped together and factors that are likely important, such as the strength of an individual’s cultural or ethnic identity were not examined. Future research should evaluate these factors in relation to the family resilience model.
Conclusions and Implications
In sum, the current study tested the family resilience model in the midst of the COVID-19 pandemic, a salient stressor for families. Factor analytic results demonstrated that the meaning, control, and emotional facets of family resilience are unique but related aspects of family resilience. A path model demonstrated direct relations from pre-existing family health vulnerabilities, racial diversity status, and COVID-19 stressors to various aspects of family resilience, with pre-existing family health vulnerabilities emerging as a risk factor for lower levels of family adaptation during the pandemic similar to accumulating findings (Fosco et al., 2022). Additional concurrent links were found from pre-existing family health vulnerabilities, racial diversity status, and COVID-19 stressors to current family protective factors and family emotional vulnerability which in turn were related to family adaptation.
These results suggest that families with pre-existing health vulnerabilities may benefit most from intervention efforts during the COVID-19 pandemic. First, practitioners and scholars should assess functioning in the different family adaptive system domains to better understand resilience within the family system. These assessments can help inform the creation and implementation of prevention/intervention programs in research and practice. Moreover, results from this study demonstrate that the FRM can be used to facilitate the creation of prevention/intervention efforts at multiple levels, given that these efforts at one level often have cascading effects to other areas of the family unit (Cowan & Cowan, 2002). Specifically, since there was a relation between pre-existing health vulnerabilities and family emotional vulnerability (i.e., child and parent COVID-19 stress and impact), individual psychological interventions administered to parents and/or their children may have cascading effects to other aspects of the family system. Given the negative relation between pre-existing health vulnerabilities and current family protection which was subsequently associated with higher levels of family emotional support, providing economic or childcare support would be beneficial in improving overall family functioning. Overall, results help to increase our understanding of, and identify multiple paths to, family resilience during the COVID-19 pandemic.
Data availability
Data from this study are available in the Open Science Framework ([dataset] Perry et al., 2021).
Code availability
Analytic code is available upon request.
References
Adams, E. L., Smith, D., Caccavale, L. J., & Bean, M. K. (2021). Parents Are stressed! Patterns of parent stress across COVID-19. Frontiers in Psychiatry, 12, 626456–626456. https://doi.org/10.3389/fpsyt.2021.626456.
Ben-Yaakov, O., & Taubman - Ben-Ari, O. (2021). Personal growth in the transition to parenthood following recent parental loss. Psychological Trauma: Theory, Research, Practice, and Policy, 13(4), 496–504. https://doi.org/10.1037/tra0001005.
Boterhoven de Haan, K. L., Hafekost, J., Lawrence, D., Sawyer, M. G., & Zubrick, S. R. (2015). Reliability and validity of a short version of the general functioning subscale of the McMaster Family Assessment Device. Family Process, 54(1), 116–123. https://doi.org/10.1111/famp.12113.
Brenner, A. B., Diez-Roux, A. V., Gebreab, S. Y., Schulz, A. J., & Sims, M. (2018). The epidemiology of coping in African American adults in the Jackson Heart Study (JHS). Journal of Racial and Ethnic Health Disparities, 5(5), 978–994. https://doi.org/10.1007/s40615-017-0445-y.
Brown, S. M., Doom, J. R., Lechuga-Peña, S., Watamura, S. E., & Koppels, T. (2020). Stress and parenting during the global COVID-19 pandemic. Child Abuse & Neglect, 110(Pt 2), 104699 https://doi.org/10.1016/j.chiabu.2020.104699.
Calvano, C., Engelke, L., Di Bella, J., Kindermann, J., Renneberg, B., & Winter, S. M. (2021). Families in the Covid-19 pandemic: Parental stress, parent mental health and the occurrence of adverse childhood experiences - results of a representative survey in Germany. European Child & Adolescent Psychiatry. https://doi.org/10.1007/s0078702101739-0
Cao, X., Jiang, X., Li, X., Hui Lo, M. C. J., & Li, R. (2013). Family functioning and its predictors among disaster bereaved individuals in China: eighteen months after the Wenchuan earthquake. Plos One, 8(4), e60738 https://doi.org/10.1371/journal.pone.0060738.
Centers for Disease Control and Prevention (CDC) (2021). COVID Data Tracker. Atlanta, GA: US Department of Health and Human Services, CDC. https://covid.cdc.gov/covid-data-tracker.
Chen, C. Y.-C., Byrne, E., & Velez, T. (2021). Impact of the 2020 pandemic of COVID-19 on families with school aged children in the United States: Roles of income level and race. Journal of Family Issues, 19. https://doi.org/10.1177/0192513X21994153
Cowan, P. A., & Cowan, C. P. (2002). Interventions as tests of family systems theories: Marital and family relationships in children’s development and psychopathology. Development and Psychopathology, 14(4), 731–759.
Davison, K. K., Charles, J. N., Khandpur, N., & Nelson, T. J. (2017). Fathers’ perceived reasons for their underrepresentation in child health research and strategies to increase their involvement. Maternal and Child Health Journal, 21(2), 267–274. https://doi.org/10.1007/s10995-016-2157-z.
Dubay, L. C., & Lebrun, L. A. (2012). Health, behavior, and health care disparities: disentangling the effects of income and race in the United States. International Journal of Health Services : Planning, Administration, Evaluation, 42(4), 607–625. https://doi.org/10.2190/HS.42.4.c.
Evans, S., Mikocka-Walus, A., Klas, A., Olive, L., Sciberras, E., Karantzas, G., & Westrupp, E. M. (2020). From “It has stopped our lives” to “Spending more time together has strengthened bonds”: The varied experiences of Australian families during COVID-19. Frontiers in Psychology, 11, 588667–588667. https://doi.org/10.3389/fpsyg.2020.588667.
Fabiano, G. A., & Caserta, A. (2018). Future directions in father inclusion, engagement, retention, and positive outcomes in child and adolescent research. Journal of Clinical Child and Adolescent Psychology, 47(5), 847–862. https://doi.org/10.1080/15374416.2018.1485106.
Farley, T., Galves, A., Dickinson, L. M., & Perez, M. deJ. (2005). Stress, coping, and health: a comparison of Mexican immigrants, Mexican-Americans, and non-Hispanic whites. Journal of Immigrant Health, 7(3), 213–220. https://doi.org/10.1007/s10903-005-3678-5.
Felitti, V. J., Anda, R. F., Nordenberg, D., Williamson, D. F., Spitz, A. M., Edwards, V., Koss, M. P., & Marks, J. S. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine, 14(4), 245–258. https://doi.org/10.1016/s07493797(98)00017-8.
Fortuna, L. R., Tolou-Shams, M., Robles-Ramamurthy, B., & Porche, M. V. (2020). Inequity and the disproportionate impact of COVID-19 on communities of color in the United States: The need for a trauma-informed social justice response. Psychological Trauma, 12(5), 443–445. https://doi.org/10.1037/tra0000889.
Fosco, G. M., Sloan, C. J., Fang, S., & Feinberg, M. E. (2022). Family vulnerability and disruption during the COVID-19 pandemic: prospective pathways to child maladjustment. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 63(1), 47–57. https://doi.org/10.1111/jcpp.13458.
Freisthler, B., Gruenewald, P. J., Tebben, E., Shockley McCarthy, K., & Price Wolf, J. (2021). Understanding at the-moment stress for parents during COVID-19 stay-at-home restrictions. Social Science & Medicine, 279. https://doi.org/10.1016/j.socscimed.2021.114025
Frenzel, S. B., Junker, N. M., Avanzi, L., Bolatov, A., Haslam, S. A., Häusser, J. A., & Van Dick, R. (2022). A trouble shared is a trouble halved: The role of family identification and identification with humankind in well‐being during the COVID‐19 pandemic. British Journal of Social Psychology, 61(1), 55–82. https://doi.org/10.1111/bjso.12470.
Gallagher, M. W., Zvolensky, M. J., Long, L. J., Rogers, A. H., & Garey, L. (2020). The impact of Covid-19 experiences and associated stress on anxiety, depression, and functional impairment in American adults. Cognitive Therapy and Research, 44(6), 1043–1051. https://doi.org/10.1007/s10608-020-10143-y.
Hammonds, E. M., & Reverby, S. M. (2019). Toward a historically informed analysis of racial health disparities since 1619. American Journal of Public Health (1971), 109(10), 1348–1349. https://doi.org/10.2105/AJPH.2019.305262.
Harrist, A. W., Henry, C. S., Liu, C., & Morris, A. S. (2019). Family resilience: The power of rituals and routines in family adaptive systems. In B. H. Fiese, M. Celano, K. Deater-Deckard, E. N. Jouriles, & M. A. Whisman (Eds.), APA handbook of contemporary family psychology: Foundations, methods, and contemporary issues across the lifespan (pp. 223–239). American Psychological Association. https://doi.org/10.1037/0000099-013
Henry, C. S., Sheffield Morris, A., & Harrist, A. W. (2015). Family resilience: Moving into the third wave. Family Relations, 64(1), 22–43. https://doi.org/10.1111/fare.12106.
Hu, L. t., & Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling, 6(1), 1–55. https://doi.org/10.1080/10705519909540118.
Hughes, M. M., Wang, A., Grossman, M. K., Pun, E., Whiteman, A., Deng, L., Hallisey, E., Sharpe, J. D., Ussery, E. N., Stokley, S., Musial, T., Weller, D. L., Murthy, B. P., Reynolds, L., Gibbs-Scharf, L., Harris, L., Ritchey, M. D. & & Toblin, R. L. (2021). County-Level COVID-19 vaccination coverage and socialvulnerability - United States, December 14, 2020-March 1, 2021.MMWR. Morbidity and Mortality Weekly Report, 70(12), 431–436.
Jace, C. & Makridis, C. (2020) Will you be mine? Marriage as a protective factor during the pandemic. https://doi.org/10.2139/ssrn.3655856
Kazak, A. E., Alderfer, M., Enlow, P. T., Lewis, A. M., Vega, G., Barakat, L., Kassam-Adams, N., Pai, A., Canter, K. S., Hildenbrand, A. K., McDonnell, G. A., Price, J., Schultz, C., Sood, E., & Phan, T. L. (2021). COVID-19 Exposure and Family Impact Scales: Factor structure and initial psychometrics. Journal of Pediatric Psychology, 46(5), 504–513. https://doi.org/10.1093/jpepsy/jsab026.
Kline, R. B. (2016). Principles and practice of structural equation modeling (4th ed.). Guilford Press.
Lang, A. J. (2020). Complementary and integrative research (CAIR) lab. CAIR pandemic impact Questionnaire (C-piq). NIH public health emergency and disaster research response. Retrieved from: https://www.phenxtoolkit.org/toolkit_content/PDF/CAIR_PIQ.pdf
Liu, Q., Zhou, Y., Xie, X., Xue, Q., Zhu, K., Wan, Z., Wu, H., Zhang, J., & Song, R. (2021). The prevalence of behavioral problems among school-aged children in home quarantine during the COVID-19 pandemic in China. Journal of Affective Disorders, 279, 412–416. https://doi.org/10.1016/j.jad.2020.10.008.
Lopez, L., Hart, L. H., & Katz, M. H. (2021). Racial and ethnic health disparities related to COVID-19. JAMA: the Journal of the American Medical Association, 325(8), 719–720. https://doi.org/10.1001/jama.2020.26443
Margolis, A., Algermissen, M., Herbstman, J., Bush, N., Breton, C., Blackwell, C., & Bastain, T. (2021). Acute Stress Questions for ECHO COVID-19 Survey.
Marques de Miranda, D., da Silva Athanasio, B., Sena Oliveira, A. C., & Simoes-e-Silva, A. C. (2020). How is COVID-19 pandemic impacting mental health of children and adolescents? International Journal of Disaster Risk Reduction, 51, 101845–101845. https://doi.org/10.1016/j.ijdrr.2020.101845.
McCubbin, H. I., McCubbin, M. A., & Thompson, A. I. (1986). Family Time and Routines Index (FTRI). In: H. I. McCubbin, A. I. Thompson, & M. A. McCubbin (1996). Family assessment: Resiliency, coping and adaptation-Inventories for research and practice. (pp. 325–340). Madison: University of Wisconsin System.
Mullahy J., Robert S., & Wolfe B. (2011). Health, income, and inequality. In: D. Grusky, editor. The inequality reader. 2nd ed. Routledge; New York. pp. 622–635.
Muthén, L. K., & Muthén, B. O. (1998-2021). Mplus User’s Guide. Eighth Edition. Los Angeles, CA: Muthén & Muthén.
Oates, G. L., & Goode, J. (2013). Racial differences in effects of religiosity and mastery on psychological distress: Evidence from national longitudinal data. Society and Mental Health, 3(1), 40–58. https://doi.org/10.1177/2156869312455930.
Panzeri, A., Bertamini, M., Butter, S., Levita, L., Gibson-Miller, J., Vidotto, G., Bentall, R. P., & Bennett, K. M. (2021). Factors impacting resilience as a result of exposure to COVID-19: The ecological resilience model. PloS One, 16(8), e0256041–e0256041. https://doi.org/10.1371/journal.pone.0256041.
Park, C. L., Edmondson, D., Fenster, J. R., & Blank, T. O. (2008). Meaning making and psychological adjustment following cancer: The mediating roles of growth, life meaning, and restored just-world beliefs. Journal of Consulting and Clinical Psychology, 76(5), 863–875. https://doi.org/10.1037/a0013348.
Park, C. L., Russell, B. S., Fendrich, M., Finkelstein-Fox, L., Hutchison, M., & Becker, J. (2020). Americans’ COVID-19 stress, coping, and adherence to CDC guidelines. Journal of General Internal Medicine: JGIM, 35(8), 2296–2303. https://doi.org/10.1007/s11606-020-05898-9.
Penner, F., Elzaki, Y., Contreras, H. T., Santos, R. P., & Sarver, D. E. (2022). Behavioral, Affective, and Cognitive Parenting Mechanisms of Child Internalizing and Externalizing Problems during the COVID-19 Pandemic. Research on Child and Adolescent Psychopathology, 50(9), 1121–1138. https://doi.org/10.1007/s10802-022-00920-6.
Perry, K. J., Penner, F., Contreras, H. T, Santos, R. P., & Sarver, D. E. (2021). A U.S. National Study of Family Resilience During the COVID-19 Pandemic. Retrieved from https://osf.io/p875e.
Pierce, M., Hope, H., Ford, T., Hatch, S., Hotopf, M., John, A., Kontopantelis, E., Webb, R., Wessely, S., McManus, S., & Abel, K. M. (2020). Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. The Lancet. Psychiatry, 7(10), 883–892. https://doi.org/10.1016/S2215-0366(20)30308-4.
Power, K. (2020). The COVID-19 pandemic has increased the care burden of women and families. Sustainability: Science, Practice, & Policy, 16(1), 67–73. https://doi.org/10.1080/15487733.2020.1776561.
Prime, H., Wade, M., & Browne, D. T. (2020). Risk and resilience in family well-being during the COVID-19 pandemic. American Psychologist, 75(5), 631–643. https://doi.org/10.1037/amp0000660.
Ren, X., Huang, W., Pan, H., Huang, T., Wang, X., & Ma, Y. (2020). Mental health during the Covid-19 outbreak in China: A meta-analysis. The Psychiatric Quarterly, 91(4), 1033–1045. https://doi.org/10.1007/s11126-020-09796-5.
Rocchi, S., Ghidelli, C., Burro, R., Vitacca, M., Scalvini, S., Della Vedova, A. M., Roselli, G., Ramponi, J. P., & Bertolotti, G. (2017). The Walsh Family Resilience Questionnaire: the Italian version. Neuropsychiatric Disease and Treatment, 13, 2987–2999. https://doi.org/10.2147/NDT.S147315.
Sampige, R., Daijiazi, T., & Master, A. (2021). Analyzing the relationship between children’s schooling modality and parenting stress during the COVID-19 pandemic. Summer Undergraduate Research Fellowship. https://hdl.handle.net/10657/7776.
Sheidow, A. J., Henry, D. B., Tolan, P. H., & Strachan, M. K. (2014). The Role of Stress Exposure and Family Functioning in Internalizing Outcomes of Urban Families. Journal of Child and Family Studies, 23(8), 1351–1365. https://doi.org/10.1007/s1082601397933.
Streisand, R., Kazak, A. E., & Tercyak, K. P. (2003). Pediatric-specific parenting stress and family functioning in parents of children treated for cancer. Children’s Health Care, 32(4), 245–256. https://doi.org/10.1207/S15326888CHC3204_1.
Sytsma, S. E., Kelley, M. L., & Wymer, J. H. (2001). Development and initial validation of the child routines inventory. Journal of Psychopathology and Behavioral Assessment, 23(4), 241–251. https://doi.org/10.1023/A:1012727419873.
Taubman-Ben-Ari, O., Ben-Yaakov, O., & Chasson, M. (2021). Parenting stress among new parents before and during the COVID-19 pandemic. Child Abuse & Neglect, 117, 105080–105080. https://doi.org/10.1016/j.chiabu.2021.105080.
Trammell, J. P., Joseph, N. T., & Harriger, J. A. (2023). Racial and ethnic minority disparities in COVID-19 related health, health beliefs and behaviors, and well-being among students. Journal of American college health, 71(1), 242–248. https://doi.org/10.1080/07448481.2021.1890606.
Verlenden, J. V., Pampati, S., Rasberry, C. N., Liddon, N., Hertz, M., Kilmer, G., Viox, M. H., Lee, S., Cramer, N. K., Barrios, L. C., & Ethier, K. A. (2021). Association of children’s mode of school instruction with child and parent experiences and well-being during the COVID-19 pandemic - COVID experiences survey, United States, October 8-November 13, 2020. MMWR. Morbidity and Mortality Weekly Report, 70(11), 369–376. https://doi.org/10.15585/mmwr.mm7011a1.
Walsh, F. (2016). Applying a family resilience framework in training, practice, and research: Mastering the art of the possible. Family Process, 55(4), 616–632. https://doi.org/10.1111/famp.12260.
White House COVID-19 Team (2021a). Press briefing by White House COVID-19 Response Team and public health officials [press briefing]. https://www.whitehouse.gov/briefing-room/press-briefings/2021/02/08/press-briefing-by-white-house-covid-19-response-team-and-public-health-officials/.
White House COVID-19 Team (2021b). Press briefing by White House COVID-19 Response Team and public health officials [press briefing]. https://www.whitehouse.gov/briefing-room/press-briefings/2021/04/05/press-briefing-by-white-house-covid-19-response-team-and-public-health-officials-24/.
Williams, D. R. (2018). Stress and the mental health of populations of color: Advancing our understanding of race related stressors. Journal of Health and Social Behavior, 59(4), 466–485. https://doi.org/10.1177/0022146518814251.
Yang, H., Chen, W., Hu, Y., Chen, Y., Zeng, Y., Sun, Y., ... & Song, H. (2020). Pre-pandemic psychiatric disorders and risk of COVID-19: a UK Biobank cohort analysis. The Lancet Healthy Longevity, 1(2), e69–e79. https://doi.org/10.1016/S2666-7568(20)30013-1.
Acknowledgements
This study was funded by an Intradepartmental Discovery Opportunity Grant (no grant number) awarded to Penner (Co-PI) by the Pediatrics Discovery Council, Department of Pediatrics, University of Mississippi Medical Center (UMMC) and by research incentive funds (Sarver). The UMMC Pediatrics Discovery Council had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. Manuscript preparation was supported by a postdoctoral fellowship to the first author from the National Institute on Drug Abuse under award number T32DA017629-17.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research review board and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Perry, K.J., Penner, F., Contreras, H.T. et al. A U.S. National Study of Family Resilience During the COVID-19 Pandemic. J Child Fam Stud 32, 1627–1642 (2023). https://doi.org/10.1007/s10826-023-02581-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10826-023-02581-5