Abstract
Purpose
Male cancer survivors experience confusion about fertility following cancer treatment. The aims of this study were to evaluate survivors’ semen quality in different tumor type groups in China and to analyze the current situation and challenges of male cancer patients with sperm cryopreservation.
Methods
This was a multicenter retrospective study of male patients with cancer who underwent sperm cryopreservation in 16 regions of the national sperm banks over an 11-year period from 2010 to 2020.
Results
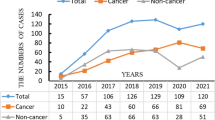
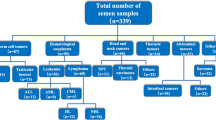
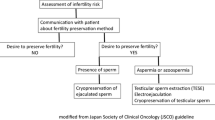
The number of male cancer patients with sperm cryopreservation showed an overall upward trend. The development of male cancer fertility preservation (FP) in the eastern, central, and western regions of Chinese displayed imbalance. There are seven tumor types for sperm preservation in the top incidence ten tumor types, including lymphoma, leukemia, nasopharyngeal carcinoma, sarcoma, thyroid cancer, and brain tumor. Moreover, nasopharyngeal carcinoma is a high incidence rate in China, which is related to high sperm preservation rate, different from other countries. The most percentage of males receiving sperm cryopreservation in the testicular cancers (15–39 years old) of China in 2020 was 5.55%, 1.29% in the lymphoma, and 0.39% in the leukemia. According to the type of cancer, a statistically significant lower pre-sperm density, total sperm output, and post-sperm density was observed in testicular cancers. It is worth noting that the prevalence of azoospermia 22.2% in leukemia patients attribute to urgent treatment before sperm cryopreservation. Disposition of cryopreserved sperm categories included continued storage (47.2%), discarded (9%), death (0.9%), and use (3.7%).
Conclusion
This study provides the first comprehensive national statistical census and review of fertility preservation in male cancer patients with respect to trends, prevalence, and cancer types. The development of male cancer fertility preservation in China is imbalanced and percentage of males receiving sperm cryopreservation in the adolescent and young adult cancers was low. Sixteen human sperm banks from China analyze current problems and challenges, and then prioritize steps toward the achievement of the FP strategy framework for Healthy China 2030.





Similar content being viewed by others
Data availability
The authors will supply the relevant data in response to reasonable requests.
References
Miller KD, Fidler-Benaoudia M, Keegan TH, Hipp HS, Jemal A, Siegel RL. Cancer statistics for adolescents and young adults, 2020. CA Cancer J Clin. 2020;70(6):443–59.
Winther JF, Kenborg L, Byrne J, Hjorth L, Kaatsch P, Kremer LC, et al. Childhood cancer survivor cohorts in Europe. Acta Oncol. 2015;54(5):655–68.
Jensen CFS, Dong L, Gul M, Fode M, Hildorf S, Thorup J, et al. Fertility preservation in boys facing gonadotoxic cancer therapy. Nat Rev Urol. 2022;19(2):71–83.
Ward ZJ, Yeh JM, Bhakta N, Frazier AL, Girardi F, Atun R. Global childhood cancer survival estimates and priority-setting: a simulation-based analysis. Lancet Oncol. 2019;20(7):972–83.
Ashizawa M, Kanda Y. Preservation of fertility in patients with hematological malignancies. Jpn J Clin Oncol. 2020;50(7):729–42.
Leader A, Lishner M, Michaeli J, Revel A. Fertility considerations and preservation in haemato-oncology patients undergoing treatment. Br J Haematol. 2011;153(3):291–308.
van Casteren NJ, Boellaard WP, Romijn JC, Dohle GR. Gonadal dysfunction in male cancer patients before cytotoxic treatment. Int J Androl. 2010;33(1):73–9.
Rueffer U, Breuer K, Josting A, Lathan B, Sieber M, Manzke O, et al. Male gonadal dysfunction in patients with Hodgkin’s disease prior to treatment. Ann Oncol. 2001;12(9):1307–11.
Tournaye H, Dohle GR, Barratt CL. Fertility preservation in men with cancer. Lancet. 2014;384(9950):1295–301.
Martinez F, International Society for Fertility Preservation E-AEWG. Update on fertility preservation from the Barcelona international society for fertility preservation-ESHRE-ASRM 2015 expert meeting: indications, results and future perspectives. Fertil Steril. 2017;108(3):407-15.e11.
Oktay K, Harvey BE, Loren AW. Fertility preservation in patients with cancer: ASCO clinical practice guideline update summary. J Oncol Pract. 2018;14(6):381–5.
Handelsman DJ. Optimal power transformations for analysis of sperm concentration and other semen variables. J Androl. 2002;23(5):629–34.
Daudin M, Rives N, Walschaerts M, Drouineaud V, Szerman E, Koscinski I, et al. Sperm cryopreservation in adolescents and young adults with cancer: results of the French national sperm banking network (CECOS). Fertil Steril. 2015;103(2):478-86.e1.
Borgmann-Staudt A, Michael S, Sommerhaeuser G, Fernandez-Gonzalez MJ, Friedrich LA, Klco-Brosius S, et al. The use of assisted reproductive technology by European childhood cancer survivors. Curr Oncol. 2022;29(8):5748–62.
Al-Jebari Y, Rylander L, Stahl O, Giwercman A. Risk of congenital malformations in children born before paternal cancer. JNCI Cancer Spectr. 2018;2(2):pky027.
Kourta D, Kanbar M, Amorim CA, Wyns C. Cancer cell contamination and decontamination methods for ovaries and testes: special focus on prepubertal gonads with a view to safe fertility restoration. Hum Reprod. 2023;38(5):780–98.
Pawlowski P, Zietara KJ, Michalczyk J, Fryze M, Buchacz A, Zaucha-Prazmo A, et al. Fertility preservation in children and adolescents during oncological treatment-a review of healthcare system factors and attitudes of patients and their caregivers. Cancers (Basel). 2023;15(17):4393.
Tam S, Puri N, Stephens D, Mitchell L, Giuliani M, Papadakos J, Gupta AA. Improving access to standardized fertility preservation information for older adolescents and young adults with cancer: using a user-centered approach with young adult patients, survivors, and partners to refine fertility knowledge transfer. J Cancer Educ. 2018;33(3):528–35.
Stigliani S, Massarotti C, De Leo C, Maccarini E, Sozzi F, Cagnacci A, et al. Fifteen year regional center experience in sperm banking for cancer patients: use and reproductive outcomes in survivors. Cancers (Basel). 2021;13(1):116.
Depalo R, Falagario D, Masciandaro P, Nardelli C, Vacca MP, Capuano P, et al. Fertility preservation in males with cancer: 16-year monocentric experience of sperm banking and post-thaw reproductive outcomes. Ther Adv Med Oncol. 2016;8(6):412–20.
Song SH, Kim DK, Sung SY, Her YS, Lee OH, Choi MH, et al. Long-term experience of sperm cryopreservation in cancer patients in a single fertility center. World J Mens Health. 2019;37(2):219–25.
Muller I, Oude Ophuis RJ, Broekmans FJ, Lock TM. Semen cryopreservation and usage rate for assisted reproductive technology in 898 men with cancer. Reprod Biomed Online. 2016;32(2):147–53.
Shankara-Narayana N, Di Pierro I, Fennell C, Ly LP, Bacha F, Vrga L, et al. Sperm cryopreservation prior to gonadotoxic treatment: experience of a single academic centre over 4 decades. Hum Reprod. 2019;34(5):795–803.
Liu X, Liu B, Liu S, Xian Y, Zhao W, Zhou B, et al. Male cancer patient sperm cryopreservation for fertility preservation: 10-year monocentric experience. Basic Clin Androl. 2021;31(1):24.
Ferrari S, Paffoni A, Filippi F, Busnelli A, Vegetti W, Somigliana E. Sperm cryopreservation and reproductive outcome in male cancer patients: a systematic review. Reprod Biomed Online. 2016;33(1):29–38.
van Casteren NJ, van Santbrink EJ, van Inzen W, Romijn JC, Dohle GR. Use rate and assisted reproduction technologies outcome of cryopreserved semen from 629 cancer patients. Fertil Steril. 2008;90(6):2245–50.
Agarwal A, Ranganathan P, Kattal N, Pasqualotto F, Hallak J, Khayal S, Mascha E. Fertility after cancer: a prospective review of assisted reproductive outcome with banked semen specimens. Fertil Steril. 2004;81(2):342–8.
Kawai K, Nishiyama H. Preservation of fertility of adult male cancer patients treated with chemotherapy. Int J Clin Oncol. 2019;24(1):34–40.
Dearing C, Breen D, Bradshaw A, Ramsay J, Lindsay K. Trends and usage in a London National Health Service Sperm Bank for cancer patients. Hum Fertil (Camb). 2014;17(4):289–96.
Ragni G, Somigliana E, Restelli L, Salvi R, Arnoldi M, Paffoni A. Sperm banking and rate of assisted reproduction treatment: insights from a 15-year cryopreservation program for male cancer patients. Cancer. 2003;97(7):1624–9.
Lackamp N, Wilkemeyer I, Jelas I, Keller U, Bullinger L, Stintzing S, le Coutre P. Survey of long-term experiences of sperm cryopreservation in oncological and non-oncological patients: usage and reproductive outcomes of a large monocentric cohort. Front Oncol. 2021;11:772809.
Hoffman A, Crocker L, Mathur A, Holman D, Weston J, Campbell S, et al. Patients’ and providers’ needs and preferences when considering fertility preservation before cancer treatment: decision-making needs assessment. JMIR Form Res. 2021;5(6):e25083.
Tseng LM, Lien PJ, Huang CY, Tsai YF, Chao TC, Huang SM. Developing a web-based shared decision-making tool for fertility preservation among reproductive-age women with breast cancer: an action research approach. J Med Internet Res. 2021;23(3):e24926.
Funding
This study is funded by the Sichuan Science and Technology Program (2022YFS0045), Dr. Fuping Li; Guangzhou Municipal Science and Technology Bureau (202002030480), Qiling Wang; Department of Natural Resources of Guangdong Province (2021A1515011544), Xinzong Zhang.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of West China Second University Hospital, Sichuan University (No: 2020–001).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, X., Wang, Q., Sheng, H. et al. Fertility preservation in males with cancer of trends, region development, and efficacy in mainland China from 16 regions Chinese sperm banks. J Assist Reprod Genet (2024). https://doi.org/10.1007/s10815-024-03121-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10815-024-03121-w