Abstract
Purpose
Some women undergoing stimulated cycles have elevated serum progesterone (P) on the day of ovulation trigger, but its effect on embryo quality is unclear. We analyze embryo quality among patients with high and low serum P undergoing preimplantation genetic testing for aneuploidy (PGT-A).
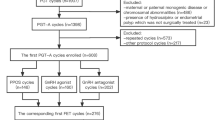
Methods
This retrospective study included 1597 patients divided into two groups by serum P values: < 1.5 ng/mL or ≥ 1.5 ng/mL. A gonadotrophin-releasing hormone (GnRH) antagonist protocol was established for each patient. Serum P levels were measured on the day of triggering. Propensity score matching and Poisson regression were done. Age, body mass index, and ovarian sensitivity index were also compared.
Results
Elevated serum P was not significantly associated with euploid embryo rate or other embryo-quality variables evaluated in our study. Age was the only variable associated with euploidy rate (per MII oocyte, P < 0.001; per biopsied embryo, P = 0.008), embryo biopsy rate (P < 0.001), absolute number of euploid embryos (P = 0.008), and top-quality embryo rate (P = 0.008). Categorical variables decreased in value for every year of increased age in patients with high serum P.
Conclusions
Elevated serum P did not affect the number of euploid and good-quality embryos for transfer in GnRH antagonist intracytoplasmic sperm injection (ICSI) cycles. Contrary to the clear influence of premature P elevation on endometrial receptivity based on literature, our results may help to tip the balance towards the absence of a negative effect of P elevation on embryo competence. More studies are needed to fully understand the effect of P elevation on reproductive outcomes.

Similar content being viewed by others
Data availability
The data that support the findings were stored in the IVI RMA Valencia computer system. The data collected are coded and pseudonymized so that no personal and clinical information of each patient can be identified.
References
Bosch E, Labarta E, Crespo J, Simón C, Remohí J, Jenkins J, et al. Circulating progesterone levels and ongoing pregnancy rates in controlled ovarian stimulation cycles for in vitro fertilization: analysis of over 4000 cycles. Hum Reprod. 2010;25:2092–100.
Hernandez-Nieto C, Lee JA, Alkon-Meadows T, Luna-Rojas M, Mukherjee T, Copperman AB, et al. Late follicular phase progesterone elevation during ovarian stimulation is not associated with decreased implantation of chromosomally screened embryos in thaw cycles. Hum Reprod. 2020;35:1889–99.
Venetis CA, Kolibianakis EM, Bosdou JK, Tarlatzis BC. Progesterone elevation and probability of pregnancy after IVF: a systematic review and meta-analysis of over 60 000 cycles. Hum Reprod Update. 2013;19:433–57.
Schoolcraft W, Sinton E, Schlenker T, Huynh D, Hamilton F, Meldrum DR. Lower pregnancy rate with premature luteinization during pituitary suppression with leuprolide acetate. Fertil Steril. 1991;55:563–6.
Fleming R, Jenkins J. The source and implications of progesterone rise during the follicular phase of assisted reproduction cycles. Reprod BioMed Online. 2010;21:446–9.
Shapiro BS, Daneshmand ST, Garner FC, Aguirre M, Hudson C, Thomas S. Embryo cryopreservation rescues cycles with premature luteinization. Fertil Steril. 2010;93:636–41.
Healy MW, Yamasaki M, Patounakis G, Richter KS, Devine K, DeCherney AH, et al. The slow growing embryo and premature progesterone elevation: compounding factors for embryo-endometrial asynchrony. Hum Reprod. 2017;32:362–7.
Labarta E, MartÍnez-Conejero JA, Alamá P, Horcajadas JA, Pellicer A, Simón C, et al. Endometrial receptivity is affected in women with high circulating progesterone levels at the end of the follicular phase: a functional genomics analysis. Hum Reprod. 2011;26:1813–25.
Xiong Y, Wang J, Liu L, Chen X, Xu H, Li TC, et al. Effects of high progesterone level on the day of human chorionic gonadotrophin administration in in vitro fertilization cycles on epigenetic modification of endometrium in the peri-implantation period. Fertil Steril. Elsevier Inc. 2017;108:269–276.e1.
Huang B, Ren X, Wu L, Zhu L, Xu B, Li Y, et al. Elevated progesterone levels on the day of oocyte maturation may affect top quality embryo IVF cycles. Sun Q-Y, editor. PLoS One. 2016;11:e0145895.
Racca A, Santos-Ribeiro S, De Munck N, Mackens S, Drakopoulos P, Camus M, et al. Impact of late-follicular phase elevated serum progesterone on cumulative live birth rates: is there a deleterious effect on embryo quality? Hum Reprod. 2018;33:860–8.
Vanni VS, Somigliana E, Reschini M, Pagliardini L, Marotta E, Faulisi S, et al. Top quality blastocyst formation rates in relation to progesterone levels on the day of oocyte maturation in GnRH antagonist IVF/ ICSI cycles. Kim S, editor. PLoS One. 2017;12:e0176482.
Ubaldi F, Smitz J, Wisanto A, Joris H, Schiettecatte J, Derde MP, et al. Oocyte and embryo quality as well as pregnancy rate in intracytoplasmic sperm injection are not affected by high follicular phase serum progesterone. Hum Reprod. 1995;10:3091–6.
Melo MAB, Meseguer M, Garrido N, Bosch E, Pellicer A, Remohí J. The significance of premature luteinization in an oocyte-donation programme. Hum Reprod. 2006;21:1503–7.
Lahoud R, Kwik M, Ryan J, Al-Jefout M, Foley J, Illingworth P. Elevated progesterone in GnRH agonist down regulated in vitro fertilisation (IVFICSI) cycles reduces live birth rates but not embryo quality. Arch Gynecol Obstet. 2012;285:535–40.
Xu B, Li Z, Zhang H, Jin L, Li Y, Ai J, et al. Serum progesterone level effects on the outcome of in vitro fertilization in patients with different ovarian response: an analysis of more than 10,000 cycles. Fertil Steril. Elsevier Inc. 2012;97:1321–7.
Racca A, De Munck N, Santos-Ribeiro S, Drakopoulos P, Errazuriz J, Galvao A, et al. Do we need to measure progesterone in oocyte donation cycles? A retrospective analysis evaluating cumulative live birth rates and embryo quality. Hum Reprod. 2020;35:167–74.
Fanchin R, Righini C, Olivennes F, De Ziegler D, Selva J, Frydman R. Premature progesterone elevation does not alter oocyte quality in in vitro fertilization. Fertil Steril. 1996;65:1178–83.
Shufaro Y, Sapir O, Oron G, Ben Haroush A, Garor R, Pinkas H, et al. Progesterone-to-follicle index is better correlated with in vitro fertilization cycle outcome than blood progesterone level. Fertil Steril. 2015;103:669–74.
Ovarian Stimulation TEGG on, Bosch E, Broer S, Griesinger G, Grynberg M, Humaidan P, et al. ESHRE guideline: ovarian stimulation for IVF/ICSI. Hum Reprod Open. 2020;2020:1–13.
Alpha Scientists in Reproductive Medicine and ESHRE Special Interest Group of Embryology. The Istanbul consensus workshop on embryo assessment: proceedings of an expert meeting. Hum Reprod. 2011;26:1270–83.
de los Santos MJ, Diez Juan A, Mifsud A, Mercader A, Meseguer M, Rubio C, et al. Variables associated with mitochondrial copy number in human blastocysts: what can we learn from trophectoderm biopsies? Fertil Steril. 2018;109:110–7.
Silverberg KM, Martin M, Olive DL, Burns WN, Schenken RS. Elevated serum progesterone levels on the day of human chorionic gonadotropin administration in in vitro fertilization cycles do not adversely affect embryo quality. Fertil Steril. 1994;61:508–13.
Urrego R, Herrera-Puerta E, Chavarria NA, Camargo O, Wrenzycki C, Rodriguez-Osorio N. Follicular progesterone concentrations and messenger RNA expression of MATER and OCT-4 in immature bovine oocytes as predictors of developmental competence. Theriogenology. 2015;83:1179–87.
Fair T, Lonergan P. The role of progesterone in oocyte acquisition of developmental competence. Reprod Domest Anim. 2012;47:142–7.
Papanikolaou EG, Kolibianakis EM, Pozzobon C, Tank P, Tournaye H, Bourgain C, et al. Progesterone rise on the day of human chorionic gonadotropin administration impairs pregnancy outcome in day 3 single-embryo transfer, while has no effect on day 5 single blastocyst transfer. Fertil Steril. 2009;91:949–52.
Roque M, Valle M, Guimarães F, Sampaio M, Geber S. Freeze-all cycle for all normal responders? J Assist Reprod Genet. 2017;34:179–85.
Xue Y, Tong X, Zhu H, Li K, Zhang S. Freeze-all embryo strategy in poor ovarian responders undergoing ovarian stimulation for in vitro fertilization. Gynecol Endocrinol. 2018;34:680–3.
Roque M, Nuto Nóbrega B, Valle M, Sampaio M, Geber S, Haahr T, et al. Freeze-all strategy in IVF/ICSI cycles: An update on clinical utility. Panminerva Med. 2019;61:52–7.
Lawrenz B, Labarta E, Fatemi H, Bosch E. Premature progesterone elevation: targets and rescue strategies. Fertil Steril. 2018;109:577–82.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Maria José De los Santos, Mar Nohales, and Maria Luisa Pardiñas. The first draft of the manuscript was written by Maria Luisa Pardiñas, and all authors commented on the previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was conducted retrospectively using data obtained for clinical purposes. It was approved by the Ethical Committee of Clinical Research IVI Valencia (1503-VLC-017-AM).
Consent to participate
This is research of general scientific interest and will be carried out in the same center where the data was obtained; therefore, it is not considered necessary to obtain the informed consent of the subjects. There is no opposition from the subjects to the use of the data for the intended purposes.s
Consent for publication
Authors are responsible for the correctness of the statements provided in the manuscript.
Conflicts of interest
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pardiñas, M.L., Nohales, M., Labarta, E. et al. Elevated serum progesterone does not impact euploidy rates in PGT-A patients. J Assist Reprod Genet 38, 1819–1826 (2021). https://doi.org/10.1007/s10815-021-02197-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-021-02197-y