Abstract
Objectives
This study aimed to evaluate the role of intracytoplasmic sperm injection (ICSI) in the treatment of non-male factor infertile patients aged ≥ 39.
Methods
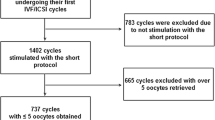
This is a single-center, prospective, randomized controlled clinical trial, between March 2018 and December 2019. Sixty-nine patients were recruited, and sixty patients participated in the study. Their ovaries were randomized prior to the beginning of the ovarian stimulation: the oocytes from one side (n = 257) were allocated to the ICSI (ICSI arm), while those of the contralateral side (n = 258) were allocated to conventional insemination (IVF arm). The fertilization rate per oocyte retrieved, number of zygotes (2PN), and cleavage-stage embryos were assessed and compared between the two study groups.
Results
The average number of zygotes (3.1 vs. 2.7 p = 0.45), the fertilization rate (72.4% vs. 65.1% p = 0.38), the average number of cleavage-stage (2.8 vs. 2.4 p = 0.29), and the average top-quality embryos (TQE) cleavage-stage embryos (1.7 vs. 1.6 p = 0.94) were comparable between the two groups. The TQE rate per randomized oocyte (41.2% vs. 41% p = 0.8) was also similar in both groups.
Conclusions
ICSI does not improve the reproductive outcomes of advanced-age patients undergoing conventional insemination for non-male factor infertility.
Trial registration
NCT03370068

Similar content being viewed by others
References
Boulet SL, Mehta A, Kissin DM, Warner L, Kawwass JF, Jamieson DJ. Trends in use of and reproductive outcomes associated with intracytoplasmic sperm injection. JAMA. 2015;313(3):255–63.
Dyer S, Chambers GM, de Mouzon J, Nygren KG, Zegers-Hochschild F, Mansour R, et al. International Committee for Monitoring Assisted Reproductive Technologies world report: assisted reproductive technology 2008, 2009 and 2010. Hum Reprod. 2016;31(7):1588–609.
Bhattacharya S, Hamilton MPR, Shaaban M, Khalaf Y, Seddler M, Ghobara T, et al. Conventional in-vitro fertilisation versus intracytoplasmic sperm injection for the treatment of non-male-factor infertility: a randomised controlled trial. Lancet. 2001;357(9274):2075–9.
De Munck N, et al. Intracytoplasmic sperm injection is not superior to conventional IVF in couples with non-male factor infertility and preimplantation genetic testing for aneuploidies (PGT-A). Hum Reprod. 2020;35(2):317–27.
Aboulghar MA, Mansour RT, Serour GI, Sattar MA, Amin YM. Intracytoplasmic sperm injection and conventional in vitro fertilization for sibling oocytes in cases of unexplained infertility and borderline semen. J Assist Reprod Genet. 1996;13(1):38–42.
Ruiz A, Remohí J, Minguez Y, Guanes PP, Simón C, Pellicer A. The role of in vitro fertilization and intracytoplasmic sperm injection in couples with unexplained infertility after failed intrauterine insemination. Fertil Steril. 1997;68(1):171–3.
Tournaye H, Verheyen G, Albano C, Camus M, van Landuyt L, Devroey P, et al. Intracytoplasmic sperm injection versus in vitro fertilization: a randomized controlled trial and a meta-analysis of the literature. Fertil Steril. 2002;78(5):1030–7.
Davies MJ, Moore VM, Willson KJ, van Essen P, Priest K, Scott H, et al. Reproductive technologies and the risk of birth defects. N Engl J Med. 2012;366(19):1803–13.
Maman E, Geva LL, Yerushalmi G, Baum M, Dor J, Hourvitz A. ICSI increases ongoing pregnancy rates in patients with poor response cycle: multivariate analysis of 2819 cycles. Reprod BioMed Online. 2012;25(6):635–41.
Farhi J, Cohen K, Mizrachi Y, Weissman A, Raziel A, Orvieto R. Should ICSI be implemented during IVF to all advanced-age patients with non-male factor subfertility? Reprod Biol Endocrinol. 2019;17(1):30.
Tannus S, Son WY, Gilman A, Younes G, Shavit T, Dahan MH. The role of intracytoplasmic sperm injection in non-male factor infertility in advanced maternal age. Hum Reprod. 2017;32(1):119–24.
Bar-Hava I, Orvieto R, Ferber A, Ashkenazi J, Dicker D, Ben-Rafael Z. Standard in vitro fertilization or intracytoplasmic sperm injection in advanced female age--what may be expected? Gynecol Endocrinol. 1999;13(2):93–7.
Ziebe S, Lundin K, Janssens R, Helmgaard L, Arce JC, for the MERIT (Menotrophin vs Recombinant FSH in vitro Fertilisation Trial) Group. Influence of ovarian stimulation with HP-hMG or recombinant FSH on embryo quality parameters in patients undergoing IVF. Hum Reprod. 2007;22(9):2404–13.
Kilani SS, Cooke S, Kan AK, Chapman MG. Do age and extended culture affect the architecture of the zona pellucida of human oocytes and embryos? Zygote. 2006;14(1):39–44.
Bertrand E, Van den Bergh M, Englert Y. Does zona pellucida thickness influence the fertilization rate? Hum Reprod. 1995;10(5):1189–93.
Sunderam S, Boulet SL, Kawwass JF, Kissin DM. Comparing fertilization rates from intracytoplasmic sperm injection to conventional in vitro fertilization among women of advanced age with non-male factor infertility: a meta-analysis. Fertil Steril. 2020;113(2):354–63 e1.
Batsry L, Orvieto R, Mor-Hadar D, Yung Y, Gitman H, Shimon C, et al. Can we predict oocyte maturation prior to denudation for intracytoplasmic sperm injection? Gynecol Endocrinol. 2020;36(3):265–7.
Haas J, Meriano J, Bassil R, Barzilay E, Casper RF. What is the optimal timing of embryo transfer when there are only one or two embryos at cleavage stage? Gynecol Endocrinol. 2019;35(8):665–8.
Racowsky C, Jackson KV, Cekleniak NA, Fox JH, Hornstein MD, Ginsburg ES. The number of eight-cell embryos is a key determinant for selecting day 3 or day 5 transfer. Fertil Steril. 2000;73(3):558–64.
Xiao JS, Healey M, Talmor A, Vollenhoven B. When only one embryo is available, is it better to transfer on day 3 or to grow on? Reprod BioMed Online. 2019;39(6):916–23.
Lee SH, Lee JH, Park YS, Yang KM, Lim CK. Comparison of clinical outcomes between in vitro fertilization (IVF) and intracytoplasmic sperm injection (ICSI) in IVF-ICSI split insemination cycles. Clin Exp Reprod Med. 2017;44(2):96–104.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by our institutional review board (IRB), and all participants provided a written informed consent before entry.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Jigal Haas and Tal Elkan Miller are joint first authors
Rights and permissions
About this article
Cite this article
Haas, J., Miller, T.E., Nahum, R. et al. The role of ICSI vs. conventional IVF for patients with advanced maternal age—a randomized controlled trial. J Assist Reprod Genet 38, 95–100 (2021). https://doi.org/10.1007/s10815-020-01990-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-020-01990-5