Abstract
Purpose
To study the incidence of tumor suppressor gene (TSG) mutations in men and women with impaired gametogenesis.
Methods
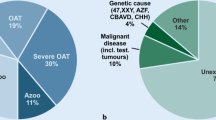
Gene association analyses were performed on blood samples in two distinct patient populations: males with idiopathic male infertility and females with unexplained diminished ovarian reserve (DOR). The male study group consisted of men with idiopathic azoospermia, oligozoospermia, asthenozoospermia, or teratozoospermia. Age-matched controls were men with normal semen analyses. The female study group consisted of women with unexplained DOR with anti-Müllerian hormone levels ≤ 1.1 ng/mL. Controls were age-matched women with normal ovarian reserve (> 1.1 ng/mL).
Results
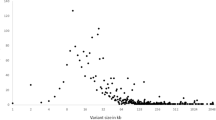
Fifty-seven male cases (mean age = 38.4; mean sperm count = 15.7 ± 12.1; mean motility = 38.2 ± 24.7) and 37 age-matched controls (mean age = 38.0; mean sperm count = 89.6 ± 37.5; mean motility = 56.2 ± 14.3) were compared. Variants observed in CHD5 were found to be enriched in the study group (p = 0.000107). The incidence of CHD5 mutation c.*3198_*3199insT in the 3′UTR (rs538186680) was significantly higher in cases compared to controls (p = 0.0255). 72 DOR cases (mean age = 38.7; mean AMH = 0.5 ± 0.3; mean FSH = 11.7 ± 12.5) and 48 age-matched controls (mean age = 37.6; mean AMH = 4.1 ± 3.0; mean FSH = 7.1 ± 2.2) were compared. Mutations in CHD5 (c.-140A>C), RB1 (c.1422-18delT, rs70651121), and TP53 (c.376-161A>G, rs75821853) were found at significantly higher frequencies in DOR cases compared to controls (p ≤ 0.05). In addition, 363 variants detected in the DOR patients were not present in the control group.
Conclusion
Unexplained impaired gametogenesis in both males and females may be associated with genetic variation in TSGs. TSGs, which play cardinal roles in cell-cycle control, might also be critical for normal spermatogenesis and oogenesis. If validated in larger prospective studies, it is possible that TSGs provide an etiological basis for some patients with impaired gametogenesis.
Similar content being viewed by others
References
Gunes S, Al-Sadaan M, Agarwal A. Spermatogenesis, DNA damage and DNA repair mechanisms in male infertility. Reprod BioMed Online. 2015;31(3):309–19.
Sanchez F, Smitz J. Molecular control of oogenesis. Biochim Biophys Acta Mol basis Dis. 2012;1822(12):1896–912.
O’Shaughnessy PJ. Hormonal control of germ cell development and spermatogenesis. Semin Cell Dev Biol. 2014;29:55–65.
Matzuk MM, Lamb DJ. Genetic dissection of mammalian fertility pathways. Nat Cell Biol. 2002;4:S33–40.
Kalro BN. Impaired fertility caused by endocrine dysfunction in women. Endocrinol Metab Clin N Am. 2003;32(3):573–92.
Harris SE, Kandil HMS, Niederberger CS. Endocrinopathies in male infertility. In: Sabanegh ES, editor. Male infertility: problems and solutions. Totowa, NJ: Humana Press; 2011. p. 47–55.
Hixon ML, Gualberto A. The control of mitosis. Front Biosci. 2000;5:D50–7.
Cohen PE, Pollack SE, Pollard JW. Genetic analysis of chromosome pairing, recombination, and cell cycle control during first meiotic prophase in mammals. Endocr Rev. 2006;27(4):398–426.
MacQueen AJ, Hochwagen A. Checkpoint mechanisms: the puppet masters of meiotic prophase. Trends Cell Biol. 2011;21(7):393–400.
Gorbsky GJ. The spindle checkpoint and chromosome segregation in meiosis. FEBS J. 2015;282(13):2471–87.
Collins JK, Jones KT. DNA damage responses in mammalian oocytes. Reproduction. 2016;152(1):R15–22.
Aitken RJ, Buckingham D, West K, Wu FC, Zikopoulos K, Richardson DW. Differential contribution of leucocytes and spermatozoa to the generation of reactive oxygen species in the ejaculates of oligozoospermic patients and fertile donors. J Reprod Fertil. 1992;94(2):451–62.
Sharma R, Masaki J, Agarwal A. Sperm DNA fragmentation analysis using the TUNEL assay. In: Methods in molecular biology (Clifton, NJ). 2013. p. 121–136.
Tamburrino L, Marchiani S, Montoya M, Elia Marino F, Natali I, Cambi M, et al. Mechanisms and clinical correlates of sperm DNA damage. Asian J Androl. 2012;14(1):24–31.
Meistrich ML, Mohapatra B, Shirley CR, Zhao M. Roles of transition nuclear proteins in spermiogenesis. Chromosoma. 2003;111(8):483–8.
Rousseaux S, Boussouar F, Gaucher J, Reynoird N, Montellier E, Curtet S, et al. Molecular models for post-meiotic male genome reprogramming. Syst Biol Reprod Med. 2011;57(1–2):50–3.
Sakkas D, Mariethoz E, Manicardi G, Bizzaro D, Bianchi PG, Bianchi U. Origin of DNA damage in ejaculated human spermatozoa. Rev Reprod. 1999;4(1):31–7.
Sakkas D, Mariethoz E. St. John JC. Abnormal sperm parameters in humans are indicative of an abortive apoptotic mechanism linked to the Fas-mediated pathway. Exp Cell Res. 1999;251(2):350–5.
Ménézo Y, Dale B, Cohen M. DNA damage and repair in human oocytes and embryos: a review. Zygote. 2010;18(4):357–65.
Oktay K, Kim JY, Barad D, Babayev SN. Association of BRCA1 mutations with occult primary ovarian insufficiency: a possible explanation for the link between infertility and breast/ovarian cancer risks. J Clin Oncol. 2010;28(2):240–4.
Wang ET, Pisarska MD, Bresee C, Chen Y-DI, Lester J, Afshar Y, et al. BRCA1 germline mutations may be associated with reduced ovarian reserve. Fertil Steril. 2014;102(6):1723–8.
Phillips K-A, Collins IM, Milne RL, McLachlan SA, Friedlander M, Hickey M, et al. Anti-Müllerian hormone serum concentrations of women with germline BRCA1 or BRCA2 mutations. Hum Reprod. 2016;31(5):1126–32.
Fraga LR, Dutra CG, Boquett JA, Vianna FSL, Gonçalves RO, Paskulin DD, et al. p53 signaling pathway polymorphisms associated to recurrent pregnancy loss. Mol Biol Rep. 2014;41(3):1871–7.
Chan Y, Zhu B, Jiang H, Zhang J, Luo Y, Tang W. Influence of TP53 Codon 72 Polymorphism alone or in combination with HDM2 SNP309 on human infertility and IVF outcome. PLoS One. 2016;11(11):e0167147.
Lu NX, Xia YK, Gu AH, Liang J, Wang SL, Wang XR. Lack of association between polymorphisms in p53 gene and spermatogenetic failure in a Chinese population. Andrologia. 2007;39(6):223–8.
Chan Y, Jiang H, Ma L, Chen J, Li D, Meng Y, et al. No association of TP 53 codon 72 SNP with male infertility: a study in a Chinese population and a meta-analysis. Syst Biol Reprod Med. 2015;61(4):222–7.
de Morais MP, Curado RF, e Silva KSF, Moura KKVO, Arruda JT. Male idiopathic infertility and the TP53 polymorphism in codon 72. Genet Mol Res 2016;15(4).
World Health Organization, editor. WHO Laboratory Manual for the Examination and Processing of Human Semen. 5th ed. Geneva: WHO Press; 2010.
Cohen J, Chabbert-Buffet N, Darai E. Diminished ovarian reserve, premature ovarian failure, poor ovarian responder--a plea for universal definitions. J Assist Reprod Genet. 2015;32(12):1709–12.
Ferraretti AP, La Marca A, Fauser BCJM, Tarlatzis B, Nargund G, Gianaroli L, et al. ESHRE consensus on the definition of “poor response” to ovarian stimulation for in vitro fertilization: the Bologna criteria. Hum Reprod. 2011;26(7):1616–24.
R Core Team. R: A language and environment for statistical computing. 2017;
Benjamini Y, Hochberg Y. Controlling the False discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Ser B. 1995;57(1):289–300.
Schwartz D, Goldfinger N, Kam Z, Rotter V. p53 controls low DNA damage-dependent premeiotic checkpoint and facilitates DNA repair during spermatogenesis. Cell Growth Differ. 1999;10(10):665–75.
Yang QE, Gwost I, Oatley MJ, Oatley JM. Retinoblastoma protein (RB1) controls fate determination in stem cells and progenitors of the mouse male germline. Biol Reprod. 2013;89(5):113.
Li W, Wu J, Kim S-Y, Zhao M, Hearn SA, Zhang MQ, et al. Chd5 orchestrates chromatin remodelling during sperm development. Nat Commun. 2014;5:3812.
Zhuang T, Hess RA, Kolla V, Higashi M, Raabe TD, Brodeur GM. CHD5 is required for spermiogenesis and chromatin condensation. Mech Dev. 2014;131:35–46.
Spiess A-N, Feig C, Schulze W, Chalmel F, Cappallo-Obermann H, Primig M, et al. Cross-platform gene expression signature of human spermatogenic failure reveals inflammatory-like response. Hum Reprod. 2007;22(11):2936–46.
Agarwal V, Bell GW, Nam J-W, Bartel DP. Predicting effective microRNA target sites in mammalian mRNS. Elife. 2015;4.
Mayr C. What are 3' UTRs doing? Cold Spring Harb Perspect Biol. 2018.
De La Fuente R, Viveiros MM, Burns KH, Adashi EY, Matzuk MM, Eppig JJ. Major chromatin remodeling in the germinal vesicle (GV) of mammalian oocytes is dispensable for global transcriptional silencing but required for centromeric heterochromatin function. Dev Biol. 2004;275(2):447–58.
Luciano AM, Franciosi F, Dieci C, Lodde V. Changes in large-scale chromatin structure and function during oogenesis: a journey in company with follicular cells. Anim Reprod Sci. 2014;149(1–2):3–10.
Marfella CGA, Imbalzano AN. The Chd family of chromatin remodelers. Mutat Res. 2007;618(1–2):30–40.
Bagchi A, Papazoglu C, Wu Y, Capurso D, Brodt M, Francis D, et al. CHD5 is a tumor suppressor at human 1p36. Cell. 2007;128(3):459–75.
Li W, Mills AA. Packing for the journey: CHD5 remodels the genome. Cell Cycle. 2014;13(12):1833–4.
Acknowledgments
Research reported in this publication was supported by the National Cancer Institute of the National Institutes of Health under Award Numbers R01CA190997, R01CA190997 Supplement, R21OD018332 and P30CA045508. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Funding
This study was funded by Cooper Genomics LLC.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hershlag, A., Peyser, A., Bristow, S.L. et al. The potential impact of tumor suppressor genes on human gametogenesis: a case-control study. J Assist Reprod Genet 37, 341–346 (2020). https://doi.org/10.1007/s10815-019-01634-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-019-01634-3