Abstract
Disruptive behaviors (DBs) are common in children with autism, affecting child and family quality of life. Parent-mediated interventions (PMIs) are a cost-effective and accessible way to decrease DBs. COVID-19 increased need for telehealth interventions. This study explored a group delivery of an evidence-based PMI (RUBI), delivered face-to-face and virtually in Israel, before and during the pandemic. Fifty-five families of children with autism and DB participated, 24 receiving face-to-face intervention and 31 receiving virtual. Outcome measures included the Aberrant Behavior Checklist and Home Situations Questionnaires. Results indicate reduction of DBs across groups, with > 50% of treatment-responders showing reliable change. This study is the first to assess RUBI outside the US among a sociodemographically diverse population, in both in-person and virtual contexts.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Autism spectrum disorder (henceforth “autism”; (Kenny et al., 2016) is a pervasive and lifelong neurodevelopmental condition characterized by impairment in social communication and interaction, and restricted, repetitive patterns of behavior, interests and activities (American Psychiatric Association, 2013). In addition to the core symptoms, children with autism often exhibit a range of behavioral problems including tantrums, aggression, self-injury, hyperactivity, impulsiveness, and/or noncompliance with routine demands and daily tasks (Lecavalier, 2006). These disruptive behaviors (DBs) interfere with the child’s performance of daily living skills, increase parental stress, and affect family quality of life (Dabrowska & Pisula, 2010; Williams et al., 2006).
A growing body of research demonstrates that early intervention can significantly improve cognitive functioning, adaptive behavior, social, developmental and behavioral outcomes in many children with autism (Reichow, 2012; Sinai-Gavrilov et al., 2020; Smith & Iadarola, 2015; Vinen et al., 2018). Specifically, early intensive behavior interventions (EIBIs) based on applied behavior analysis (ABA) have been successful in reducing DBs and improving daily living skills in children with autism (Beavers et al., 2013). EIBIs are typically delivered for multiple years at an intensity of 20 to 40 h per week, demanding a considerable investment of time, money and energy. Notably, while the vast majority of children with autism receive their treatment through community-based services, EIBIs are not readily available in all communities (Schreibman, 2000; Vivanti et al., 2018).
Parent-mediated interventions
Given the challenges that parents face in raising a child with autism and DBs, the field has seen increased interest in the application of parent training (PT) in this population (Postorino et al., 2017). PT is a form of parent-mediated intervention (PMI), wherein the goal is to provide parents with skills to effectively cope with challenges faced by their child (Oono et al., 2013). PTs have been found to be effective in lowering child DBs across labs and clinicians (Michelson et al., 2013; Bearss et al., 2013a, b).
Application of PT is typically cost effective and time-limited, which suggests that it is implementable on a larger scale than more intensive and costly interventions (Bearss et al., 2013a, b). Additionally, a parent-mediated approach to intervention enables to create therapeutic experiences spread out across the child’s day and natural environments (Oono et al., 2013), which encourages sustained effects following the intervention (Pickles et al., 2016). Such interventions can also be provided in groups (Burrell et al., 2020), which is a cost-effective way to reach more families and may have psychological benefits for participating parents. Results from a comprehensive review indicate that group-based parenting programs are effective in producing short-term improvements in several aspects of parental psychosocial functioning such as parental stress, anxiety and depression (Barlow et al., 2012). A systematic review and synthesis of qualitative research examining parents’ experience and perceptions of parenting programs suggests that gaining knowledge and skills, together with perceived acceptance and support from other parents, led to reduced feelings of guilt and social isolation, increased empathy with their children and confidence in dealing with their behavior (Kane et al., 2007).
Telehealth
Even preceding the covid-19 pandemic, telehealth was rising in popularity in clinical practice (Dorsey & Topol, 2016). Telehealth involves supplying health care remotely by using telecommunication tools, such as video calls in place of clinic visits. This provides greater flexibility to clinicians and patients regarding their location and availability (Dorsey & Topol, 2016) and could play a significant role in PT by connecting families to services, training of staff, and in serving as the primary delivery source of PT (Jones et al., 2013; Sourander, 2015).
An evolving body of research indicates the positive effects of virtual parental counseling and coaching for families of children with autism. Such interventions have been linked to improvement in child social-communication skills (e.g. Ura et al., 2021), parental responsiveness (Garnett et al., 2022), and parental behavior management skills (Bearss et al., 2018). These studies also indicate promising levels of delivery feasibility and parental acceptance of this intervention delivery modality (Ellison et al., 2021).
RUBI
The Research Unit for Behavioral Intervention (RUBI) Autism Network developed a parent-mediated intervention protocol for children with autism designed to address DBs and adaptive skill deficits (Bearss et al., 2015a, b). This protocol consists of 11 core sessions and up to two optional sessions. In these sessions, parents are taught to analyze the function of DBs and are presented with strategies for managing these behaviors, as well as generalizing and maintaining improvements over time (Bearss et al., 2015a, b). Several studies have shown that the RUBI protocol can be reliably delivered by trained clinicians and is an effective intervention for reducing disruptive behavior in children with autism, showing greater results then parent education. Parents who received individual PT based on the RUBI protocol reported increases in child compliance and decreases in DBs as measured by parent-report measures (Bearss et al., 2013a, b, 2015a, b). Recent findings also indicate positive secondary outcomes following the RUBI protocol such as improvements in parental stress, caregiver strain and parental competence as reported by parents (Iadarola et al., 2018).
A recent pilot trial of the RUBI protocol was delivered clinic-to-clinic via telehealth. In the telehealth format, slight modifications were required such as elimination of the home visits. Nevertheless, the intervention was effective and delivered reliably by therapists with high rates of parental engagement and satisfaction (Bearss et al., 2018).
RUBI in the Community
Most studies examining the efficacy of interventions for children with autism are conducted under optimal conditions in lab-based settings (Nahmias et al., 2019). Unfortunately, such interventions rarely make their way into the community and there is a significant gap between outcomes reported in efficacy trials and those observed in community settings (Nahmias et al., 2019). Research on the community delivery of PT for parents of children with autism is lacking (Dawson et al., 2020). In the current paper, “community delivery” refers to a context in which families participate in the intervention either from their homes (online) or at local community service providers, as opposed to in a university-based lab context. Without such community-based research, it is impossible to assess the effectiveness of such interventions when applied outside specialized research centers, in real world settings, delivered by community practitioners (Smith, 2007).
Additionally, demonstrating the effectiveness of a structured, manualized PT program for children with autism and DBs outside the U.S. could have important public health and research implications. The exploration of these programs in international settings, with varied populations, can provide us with evidence regarding the effectiveness of the intervention in a range of sociodemographic contexts, and the potential of reaching more families.
In addition to the research supporting the use of RUBI in one-on-one, clinic-based settings, Edwards et al., (2019) found initial support for the efficacy of the implementation of a group adaptation of the RUBI protocol delivered in community clinics. A demonstration pilot (Burrell et al., 2020) reported on the efficacy of a community-implementation of the RUBI protocol in a group format, using a modest sample size (N = 18) to provided initial evidence for its efficacy in a community setting. In that study, parents reported significant improvement with moderate to large effects in children’s disruptive behaviors 12 weeks after completing the intervention.
Autism Intervention in Israel
The State of Israel is home to multiple ethnic and cultural groups. The current population of Israel consists of approximately 75% Jews, 17% Muslim Arabs; and 8% additional minorities (Clarfield et al., 2017). Recent work (Koller et al., 2021) noted disparities in the diagnosis of autism between sociodemographic communities in the Jerusalem municipality, finding that Arab children with verbal abilities are less likely to receive a timely diagnosis. In general, there is a significantly lower rate of demand for, and availability of, medical specialists in the Arab population (Rosen et al., 2015). In sum, while the different populations in Israel are entitled to the same health services, differences in the receipt of this service clearly exist (Koller et al., 2021).
Current Study
The current study examines the efficacy of the RUBI protocol in a community-delivered, group format provided to Jewish and Arab families in Israel. The outbreak of COVID-19 near the close of the pilot period resulted in an unplanned transition from face to face (FTF) to an online format. Here, we report findings from both the FTF and online delivery, assessing primary outcomes at the close of the intervention as well as at two-month follow up. The question explored in the current study was the effect of participation in both RUBI intervention modalities on child DBs. We hypothesized that participation in both the FTF and online RUBI format would be associated with decreased DBs from pre- to post-intervention, an effect which will be maintained at follow-up, perhaps with some changes in effect size.
Method
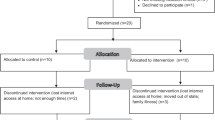
Participants included 55 parents, 24 of whom participated in the FTF groups and 31 parents who participated in online groups (See Table 1). All parents had a child between the ages of three and nine years old with a diagnosis of autism recognized by Israeli Social Security, which is dependent on a prior evaluation by both a physician and a psychologist. Parents confirmed the presence of DBs, and children could not be concurrently attending another parent-focused or behavioral intervention specifically targeting DBs. Children had receptive language age equivalent of ≥ 18 months to ensure that they could comprehend simple one-step demands, as was necessary for the intervention sessions on compliance training and teaching skills (Scahill et al., 2012). We relied on parents report regarding child’s receptive language.
Design
This study was approved by the university-affiliated Ethics Committee for Research as well as by the ethics committee of the Israeli Ministry of Education’s Office of the Chief Scientist. Parents were recruited by partner organizations in the community, including special education schools and preschools as well as community centers providing services to individuals with autism and their families. All parents provided documented informed consent to participate in the study. After initial enrollment, a study coordinator spoke with each family on the phone to confirm that inclusion criteria were met. Once the partner site recruited a sufficient number of parents, we assigned a therapist from the research team to the group who then coordinated directly with the families and travelled to the community site to deliver the intervention (in FTF groups).
This was a 12-weeks open trial of the RUBI protocol that included 11 core sessions, one optional session, and one home visit. We conducted nine groups of three to four participants in FTF settings. The second wave of groups commenced after the onset of the COVID-19 pandemic. Therefore, the intervention sessions were conducted virtually over Zoom, including the home visit, which took place virtually. Thirteen groups were conducted online. A primary clinician led each group, with support from a secondary clinician. Clinicians were advanced students either in an ABA training program or in graduate programs in clinical child/school psychology or special education. Clinicians were trained by a clinical psychologist with expertise in autism and early childhood, and by a board-certified behavior analyst (BCBA). Weekly supervision took place with the BCBA where session content was reviewed. We assessed fidelity to the RUBI protocol with a weekly checklist detailing the required elements for each session and, after each session, the primary clinician indicated the degree to which the in-session’s goals were achieved by responding to a set of 10 questions on a Likert-type scale of 1–4, indicating to what degree each topic was covered. In addition, another set of questions, also on Likert-type scale of 1–4, addressed to what degree the parents understood and participated in the session. A randomly selected session from each group was video-recorded and an independent rater compared the video to that week’s fidelity checklist. We administered outcome measures at baseline, week 4, 8, 12, and then 4 and 8 weeks after the last session.
Measures
Participant Characterization
Demographic questionnaire: Parents completed a demographic questionnaire at the home visit prior to beginning the intervention, which provided information regarding the child’s sex, age, diagnoses, siblings, educational placement, medical history, use of medications, services and treatments received, and previous parent training and behavior management consultations the parents had participated in. In addition, parents were asked to relay any information regarding relevant family history, including psychiatric disorders or other developmental concerns in the extended family, in order for us to be aware of factors that may impact the family’s ability to participate in the study.
Social Responsiveness Scale (SRS; Constantino & Gruber 2005): The SRS is a caregiver - and teacher-report measure of child social competence with 65 items, each rated on a four-point Likert scale (1–4), with higher scores indicative of elevated difficulty in social-related behaviors, in the domains of social awareness, social cognition, social communication, social motivation, and restricted and repetitive behaviors (RRBs). In this studies, the SRS scales were found to have good internal consistency (α = 0.79–0.85) and test–retest reliability (Constantino et al., 2003). A translation (Hebrew/Arabic) of the SRS was administered to parents at baseline, at 12 weeks (endpoint) and again 8 weeks after the last session.
Adaptive Behavior Assessment System-Second Edition (ABAS-II) Parent Form: The ABAS-II (Harrison & Oakland, 2003) is a comprehensive multidimensional assessment tool used to assess the functional skills necessary for daily living, covering the ten adaptive behavior deficit areas defined by the DSM-5 (APA, 2013), and it is recommended for use as part of the standard autism diagnostic evaluation process, by the Ministry of Health in Israel. The ABAS-II consists of 232 items, each rated on a four-point Likert scale (0–3), with higher scores indicative of more adaptive functioning, on the following specific skill areas: Communication; Use of 16 Community Resources; Academic/Pre-Academic Functional Skills; Daily Living Skills; Health and Safety; Leisure; Self-Care; Self-Direction; Social and Work or Motor Skills (for children under the age of five), as well as a General Adaptive Behavior Composite Score (GAC). Reported average internal consistency reliability estimates range from 0.86 to 0.93 and corrected test-retest reliabilities are ≥ 0.87 for all skill area scores. Validity is supported in age-difference sensitivities (i.e., increased scores for each skill area as age increases). Concurrent validity is supported by moderate-to-strong correlations with other measures of adaptive functioning (e.g., VABS). The ABAS-II was administered to participating parents at baseline, 12 weeks (endpoint) and 8 weeks after last session.
Primary Outcome Measures
Aberrant Behavior Checklist (ABC): The ABC Aman et al., 1985a) is a caregiver - and teacher-report measure of DBs with 58 items, each rated on a four-point Likert scale (0–3), with higher scores indicative of more severe problem behavior, on five subscales: Irritability (tantrums, aggression and self-injury, 15 items); Social Withdrawal (16 items); Stereotypic Behavior (7 items); Hyperactivity/Noncompliance (16 items); and Inappropriate Speech (4 items). In children with autism, the ABC subscales demonstrate adequate internal consistencies (α = 0.77–0.94) and convergent validity (Kaat et al.,2014). The ABC was administered to parents and teachers at baseline, 12 weeks after baseline (endpoint), and 8 weeks after last session.
Home Situations Questionnaire (HSQ;Barkley & Murphy 1998): The HSQ is a caregiver-rated scale for child noncompliance across 24 everyday situations. Each item is rated as a problem: “yes” or “no”; “yes” items are then scored from one (mild) to nine (severe), on two subscales: ‘Demand-Specific’ - inflexible adherence to specific routines and ‘Socially Inflexible’ -impairments in social interaction. The situations described in these two subscales identify distinctly different environmental antecedents of noncompliance (Chowdhury et al., 2010). The total severity score is divided by 24 to obtain a per item mean. A translation (Hebrew/Arabic) of the slightly modified version of the HSQ, which includes five items to make the instrument more pertinent to children with autism was administered to parents at baseline, 12 weeks and again 8 weeks after last session. This version was also used in the RUPP Autism Network trial (Aman et al., 2009) and found to have adequate reliability (Chowdhury et al., 2010). The HSQ Total score was an additional primary outcome measure in the study.
Intervention
The RUBI Protocol was developed for children with autism and co-occurring DBs and was originally conducted in a one-on-one, clinic-based setting (Bearss et al., 2015b). For the current study, the core sessions from the RUBI manual were translated to Hebrew and Arabic, and delivered to groups of three to four parents. 43.6% of the groups (n = 24) were in FTF format and the others were delivered online. The RUBI is a structured protocol in which therapists follow a preset script that includes the different session objectives. The intervention includes one protocol-based home visit, 11 core sessions, and one optional session in which the topic is chosen collectively from a list according to the parents’ needs. The core sessions covered the following topics: Behavioral principles, functional behavioral analysis and the Antecedent-Behavior-Consequence model; Antecedents and prevention strategies; Use of daily schedules; Reinforcements; Extinction strategies and planned ignoring; Child compliance training; Teaching the child functional communication; Teaching skills through task analysis; Prompting strategies; Working on skill generalization and maintenance (see Appendix for the content of the protocol). The optional session dealt with crisis management. Each session lasted approximately 90 min and employed direct instruction, practice activities, role-playing and accompanying video vignettes (from the original protocol) for further illustration of skill implementation or to assess parents’ understanding of the materials. Homework was given and reviewed weekly, and included activities such as behavioral monitoring, using reinforcements, planning free-play times with the child, and more. At the beginning of each session caregivers shared the results from any homework or data collected at home during the previous week. All session activities and discussions included in the manual were completed during the session.
Results
To assess the change in parents’ reports of child DBs between pre intervention and after the last intervention session, paired sample t-tests were conducted for the online and FTF groups separately (see Table 2).
FTF intervention
The analysis showed a significant decrease in the ABC Hyperactivity scale (t[23] = -3, p < .01) and the overall ABC score (t [23] = -3.27, p < .01), indicating to a decrease in mean DBs between the two time points. A significant decrease was also found in the HSQ overall score (t[15] = -2.99, p < .01). The effect for the ABC Irritability score was not significant (t[23] = -1.53, p = .14).
The current analysis also revealed a significant decrease in teacher-reported ABC Irritability scores (t [16] = -3.36, p < .01), Hyperactivity scores (t[16] = -3.31, p < .01), and the total ABC score (t[16] = -3.76, p < .01).
Online intervention
The analysis showed a significant effect for the parent reported ABC Hyperactivity, (t[31] = -2.84, p < .01) Irritability (t[31] = -2.44, p < .05) and, and the overall ABC scale (t[30] = -2.22, p < .05) indicating to a decrease in DB. A significant decrease was also shown in the HSQ overall score (t[25] = -3.55, p < .01). Table 2 presents the means and standard deviations for the effects described above. Figure 1 presents the distributions of parent reports on the outcome measures in FTF and online intervention formats.
Reliable Change Index:
To explore individual effects of the intervention, we calculated reliable change index (RCI) for the overall ABC scales for the FTF and online intervention modalities, separately. The RCI was calculated for every participant using two different methods. The first was the change in the ABC Hyperactivity score, with 25% change being the cutoff for reliable change, as was the case in the original RCT examining RUBI (Bearss et al., 2015b). The second method was based on Bauer et al., (2004), in which the difference between the post and pre intervention scores is divided by the standard error of the respective subscales (\(RC= \frac{{Y}_{t4}-{Y}_{t1}}{ {SE}_{Difference}}\)), based on the measure’s norms (Kaat et al., 2014). A change of 1.96 or higher is considered a reliable change that is not attributed to measurement error.
In the FTF group, 15 (62.5%) of the children showed a decrease in ABC Hyperactivity scores, of which 12 (80%) demonstrated a 25% decrease and 11 (73.33%) demonstrated a 1.96 reliable change. At follow-up (8 weeks after the intervention), out of the seven participants whose data was available, four (57.1%) demonstrated a 25% decrease in symptoms, and five (71.4%) demonstrated a decrease at the 1.96 level.
In the online intervention group, 19 (61.29%) showed a decrease in ABC Hyperactivity group. Of these, 14 (73.7%) demonstrated a 25% decrease and 10 (52.6%) demonstrated a 1.96 reliable change at post-intervention. At follow-up, of the 15 participants whose data was available, six (40%) demonstrated a 25% decrease in Hyperactivity symptoms, and six (40%) demonstrated a 1.96 reliable change.
Notably, two children (8.33%) from the FTF group and one child (3.23%) from the online group demonstrated a reliable 1.96 increase in Hyperactivity symptoms, and six children (25%) from the FTF group and five children (16%) from the virtual group showed a 25% increase in Hyperactivity symptoms.
Discussion
The current study is the first to examine the effectiveness of a community-based delivery of the RUBI protocol in a group format in Israel. This study extends preliminary findings indicating the feasibility of a group adaptation of RUBI in the community (Edwards et al., 2019), providing evidence for its efficacy in community settings, with the two main ethnic groups in Israel.
This study was not conceptualized in order to compare FTF and virtual delivery of the RUBI protocol but rather to examine the efficacy of the RUBI protocol in a community-delivered, group format provided to Jewish and Arab families in Israel. As a result of pandemic-related restrictions, the study included two groups of participants: those who received RUBI Face to Face (FTF) prior to the onset of the COVID-19 pandemic, and those who received the intervention virtually during the pandemic. The current results show that both groups demonstrated an overall decrease in most of the outcome measures. Approximately 60% of participants across groups showed a decrease in ABC Hyperactivity scores, while more than 70% of those “improvers” in the FTF condition and half of the improvers in the online condition demonstrated a reliable change. Findings from the current study strengthen the notion that time-limited, symptom-focused, parent training programs such as RUBI can decrease DBs in children with autism, in both group and one-on-one formats, in the short term (Edwards et al., 2019; Burrell et al., 2020; Bearss et al., 2013a, b, 2015a, b).
Given the lack of a control group in the current study, we approached the analysis with a combination of methods in the hopes of attaining as nuanced an understanding of the outcomes as possible. In the first approach, we examined the difference between group means, beyond the individual participants. This nomothetic approach enables us to explore trends or group effects. The second approach we followed was idiographic, exploring changes in each individual participant after intervention.
We addressed the question of clinically significant improvement using three, non-mutually exclusive methods: (1) Calculating the number of children who demonstrated a decrease in DBs. The rationale behind this approach is that any numerical change reported by parents portrays a subjectively noticeable behavioral change; (2) Calculating the number of children who demonstrated a 25% decrease in DBs (Bearss et al., 2015a, b). This method of enables us to detect clinically meaningful improvement among children with high and low initial DB scores. For example, a child who shows a decrease from a score of 4 to 3, and a child who showed a decrease from 40 to 30 are considered to have made comparably significant improvement; (3) Calculating the number of children who demonstrated reliable change using the \(RC= \frac{{Y}_{t4}-{Y}_{t1}}{ {SE}_{Difference}}\)formula. This method acknowledges measurement errors as possible explanations of change in DBs, and defines reliable change as decreases that surpass the range of random measurement errors.
In addition to parent-report measures, we examined generalizability of the outcomes using teacher reports of disruptive behaviors (ABC). While not actively blinded to the child’s participation in the intervention, teachers were not informed regarding the content or goals of the treatment. At the close of the intervention, teachers reported significant improvements in disruptive behaviors with large effects, indicating that improvements in disruptive behaviors generalized to the educational setting. Notably, teacher reports were available only for the FTF group, due to prolonged lockdown periods and school closures after the onset of the COVID-19 pandemic.
Our findings buttress preliminary reports (Bearss et al., 2018) that clinicians can deliver RUBI online with outcomes similar to those observed in FTF delivery. Online delivery of parent training can make high quality, evidence-based intervention accessible to a broader swath of the global population, lowering or eliminating barriers such as geographic distance, lack of transportation, limited time availability and need for child care (Comer, 2016). Specifically in the context of the COVID-19 pandemic, the transition from FTF to online delivery of the intervention, while unplanned, allowed families to participate in the program during a time in which in-person services were largely unattainable or inconsistently delivered due to lockdown and quarantine restrictions.
This is the first study to assess the efficacy of RUBI in any format outside the United States, doing so among both Jewish and Arab families in Israel. The vast majority of early intervention models for children with ASD have been developed and tested in English-speaking countries (Colombi et al., 2018). This study shows that the RUBI protocol can be delivered effectively in international settings, in non-English-speaking communities with promising results. It is important to note that the online delivery groups had a modest number of Arab speaking participants. This might be largely attributable to difficulties in access to internet, digital literacy, telehealth awareness, and mistrust of digital services (Weber et al., 2020). These barriers highlight the limitations of telehealth in certain sociodemographic groups.
The current study is among the first to deliver RUBI in a group format. We elected this format in order to assess our ability to reach as many families as possible in as brief a time as possible. Our findings support results from a comprehensive review indicating that group-based parenting programs are effective in producing short-term improvements in a number of aspects of parental psychosocial functioning (Barlow et al., 2012). Participating in the intervention along with other parents may have secondary positive effects, in line with work showing that the acquisition of knowledge, skills and understanding, together with feelings of acceptance and support from other parents in the group, can help parents feel more able to cope (Kane et al., 2007).
In light of the challenges associated with parenting a child with autism DBs, a time-limited, group-based, PMI delivered in the community represents an accessible and, in some areas, more cost-effective means of supporting these parents. Such an approach has the potential to reach families living in distant areas who would not typically have access to expert services Relatedly, the current study indicates that RUBI has applicability outside of the United States, and that it can be delivered to the benefit of families from varied sociodemographic, cultural and ethnic backgrounds.
While the described results indicate positive outcomes for a substantial subgroup within both intervention modalities, a group of children did not show any improvement in DB. We might hypothesize any one of several factors as explanations. For instance, parental stress has been shown to interfere with parental ability to implement learned strategies (Dabrowska & Pisula, 2010). In addition, some of the participating parents may benefit from additional support or modifications to the RUBI protocol. Since the intervention was delivered weekly in a group format, however, these personal adaptations were not possible. Lastly, demographic characteristics, such as ethnicity, socioeconomic status and geographical location, might influence treatment efficacy (Raulston et al., 2019).
Limitations and Future Research
The primary and obvious methodological challenge of the current study is the lack of a control group. The end of the pilot phase (i.e. the FTF groups) coincided with the onset of the COVID-19 pandemic. Given the uncertain nature of the times, we switched to a virtual modality and made minimal other modifications to the study. Despite that, the lack of control group limits our ability to draw stronger conclusions regarding intervention effects. Another main limitation is the small sample size, which needs to be taken into consideration when contextualizing the findings. This was exacerbated in the follow-up data, where we predictably experienced difficulties with retention. Other limitations relate to the primary and secondary measures used in the study. The reliance on non-blinded parent-ratings, filled out by the same parents who participated and implemented the intervention in order to measure change in child behavior is certainly rife with potential bias. Future studies would benefit from direct assessment of the children prior to and following the intervention. In addition, RUBI does not offer a parental fidelity system. In future studies this should be added in order to assess parental implementation and its’ effects on intervention outcomes.
It is important to note that global, local, and personal stressors present during the online groups (i.e., after the onset of the pandemic) make any comparison between the FTF and the online groups moot. Future direct comparisons outside the context of global pandemics would be valuable (Dabrowska & Pisula, 2010. Finally, long-term follow-up is essential in order to determine the lasting impact of the intervention on participating children, as the current study assessed only short-term effects.
In addition to the above points, future research should focus on true implementation of RUBI and other evidence-based interventions in the community. Given these findings, supporting the delivery of RUBI in the community by trained research staff, a next step would be to train community practitioners and public service providers in the hopes of a broader deployment of the intervention. Another important question to address in future studies is that of outcome mediators and specific “active ingredients” in the RUBI that play the greatest role in its’ outcomes. Finally, a larger sample would allow for analyses focused on outcome predictors, shedding light on the ever-present question of what works for whom.
References
Aman, M. G., Mcdougle, C. J., Scahill, L., Handen, B., Arnold, L. E., Johnson, C. … Sukhodolsky, D. D. (2009). Medication and parent training in children with pervasive developmental disorders and serious behavior problems: results from a randomized clinical trial. Journal of the American Academy of Child & Adolescent Psychiatry, 48(12), 1143–1154
Aman, M. G., Singh, N. N., Stewart, A. W., & Field, C. J. (1985a). The aberrant behavior checklist: a behavior rating scale for the assessment of treatment effects. American Journal of Mental Deficiency, 89, 485–491
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (DSM-5®). American Psychiatric Pub
Barkley, R. A., & Murphy, K. R. (1998).Home Situations Questionnaire
Barlow, J., Smailagic, N., Huband, N., Roloff, V., & Bennett, C. (2012). Group-based parent training programs for improving parental psychosocial health. Campbell Systematic Reviews, 8(1), 1–197
Bauer, S., Lambert, M. J., & Nielsen, S. L. (2004). Clinical significance methods: A comparison of statistical techniques. Journal of Personality Assessment, 82(1), 60–70
Bearss, K., Burrell, T. L., Challa, S. A., Postorino, V., Gillespie, S. E., Crooks, C., & Scahill, L. (2018). Feasibility of Parent Training via Telehealth for children with autism spectrum disorder and disruptive behavior: A demonstration pilot. Journal of Autism and Developmental Disorders, 48(4), 1020–1030
Bearss, K., Burrell, T. L., Stewart, L., & Scahill, L. (2015a). Parent Training in Autism Spectrum Disorder: What’s in a Name? Clinical Child and Family Psychology Review, 18(2), 170–182
Bearss, K., Johnson, C., Handen, B., Smith, T., & Scahill, L. (2013a). A pilot study of parent training in young children with autism spectrum disorders and disruptive behavior. Journal of Autism and Developmental Disorders, 43(4), 829–840
Bearss, K., Johnson, C., Smith, T., Lecavalier, L., Swiezy, N., Aman, M. … Scahill, L. (2015b). Effect of parent training vs parent education on behavioral problems in children with autism spectrum disorder: a randomized clinical trial. JAMA, 313(15), 1524–1533
Bearss, K., Lecavalier, L., Minshawi, N., Johnson, C., Smith, T., Handen, B. … Scahill, L. (2013b). Toward an exportable parent training program for disruptive behaviors in autism spectrum disorders. Neuropsychiatry, 3(2), 169
Beavers, G. A., Iwata, B. A., & Lerman, D. C. (2013). Thirty years of research on the functional analysis of problem behavior. Journal of Applied Behavior Analysis, 46(1), 1–21
Burrell, T. L., Postorino, V., Scahill, L., Rea, H. M., Gillespie, S., Evans, A. N., & Bearss, K. (2020). Feasibility of Group Parent Training for Children with Autism Spectrum Disorder and Disruptive Behavior: A Demonstration Pilot.Journal of Autism & Developmental Disorders, 50(11)
Clarfield, A. M., Manor, O., Nun, G. B., Shvarts, S., Azzam, Z. S., Afek, A. … Israeli, A. (2017). Health and health care in Israel: an introduction. The Lancet, 389(10088), 2503–2513
Chowdhury, M., Aman, M. G., Scahill, L., Swiezy, N., Arnold, L. E., Lecavalier, L. … McDougle, C. J. (2010). The Home Situations Questionnaire-PDD version: Factor structure and psychometric properties. Journal of Intellectual Disability Research, 54(3), 281–291
Comer, J. S., & Myers, K. (2016). Future directions in the use of telemental health to improve the accessibility and quality of children’s mental health services. Journal of Child and Adolescent Psychopharmacology, 26(3), 296–300
Colombi, C., Narzisi, A., Ruta, L., Cigala, V., Gagliano, A., Pioggia, G., & Prima Pietra Team. (2018). Implementation of the early start denver model in an Italian community. Autism, 22(2), 126–133
Constantino, J. N., & Gruber, C. P. (2005). Social responsive scale (SRS) manual. Los Angeles, CA: Western Psychological Services
Constantino, J. N., Davis, S. A., Todd, R. D., Schindler, M. K., Gross, M. M., Brophy, S. L. … Reich, W. (2003). Validation of a brief quantitative measure of autistic traits: comparison of the social responsiveness scale with the autism diagnostic interview-revised. Journal of Autism and Developmental Disorders, 33(4), 427–433
Dabrowska, A., & Pisula, E. (2010). Parenting stress and coping styles in mothers and fathers of pre-school children with autism and down syndrome. Journal of Intellectual Disability Research, 54(3), 266–280
Dawson-Squibb, J. J., Davids, E. L., Harrison, A. J., Molony, M. A., & de Vries, P. J. (2020). Parent education and training for autism spectrum disorders: scoping the evidence. Autism, 24(1), 7–25
Dorsey, E. R., & Topol, E. J. (2016). State of telehealth. New England Journal of Medicine, 375(2), 154–161
Edwards, G. S., Zlomke, K. R., & Greathouse, A. D. (2019). RUBI parent training as a group intervention for children with autism: A community pilot study. Research in Autism Spectrum Disorders, 66, 101409
Ellison, K. S., Guidry, J., Picou, P., Adenuga, P., & Davis, T. E. (2021). Telehealth and autism prior to and in the age of COVID-19: a systematic and critical review of the last decade. Clinical Child and Family Psychology Review, 24(3), 599–630
Garnett, R., Davidson, B., & Eadie, P. (2022). Parent perceptions of a group telepractice communication intervention for autism. Autism & Developmental Language Impairments
Harrison, P. L., & Oakland, T. (2003). Adaptive behavior assessment system (2nd ed.). Los Angeles, CA: Western Psychological Services
Iadarola, S., Levato, L., Harrison, B., Smith, T., Lecavalier, L., Johnson, C. … Scahill, L. (2018). Teaching parents behavioral strategies for autism spectrum disorder (AUTISM): Effects on stress, strain, and competence. Journal of Autism and Developmental Disorders, 48(4), 1031–1040
Jones, D. J., Forehand, R., Cuellar, J., Kincaid, C., Parent, J., Fenton, N., & Goodrum, N. (2013). Harnessing innovative technologies to advance children’s mental health: Behavioral parent training as an example. Clinical Psychology Review, 33(2), 241–252
Kaat, A. J., Lecavalier, L., & Aman, M. G. (2014). Validity of the aberrant behavior checklist in children with autism spectrum disorders. Journal of Autism and Developmental Disorders, 44, 1103–1116
Kane, G. A., Wood, V. A., & Barlow, J. (2007). Parenting programmes: a systematic review and synthesis of qualitative research. Child Care, Health and Development, 33(6), 784–793
Kenny, L., Hattersley, C., Molins, B., Buckley, C., Povey, C., & Pellicano, E. (2016). Which terms should be used to describe autism? Perspectives from the UK autism community. Autism, 20(4), 442–462
Koller, J., Shalev, R., Schallamach, C., Gumpel, T. P., & Begin, M. (2021). The role of demographics in the age of autism diagnosis in Jerusalem. Journal of Autism and Developmental Disorders, 51(3), 769–777
Lecavalier, L. (2006). Behavioral and emotional problems in young people with pervasive developmental disorders: Relative prevalence, effects of subject characteristics, and empirical classification. Journal of Autism and Developmental Disorders, 36(8), 1101–1114
Michelson, D., Davenport, C., Dretzke, J., Barlow, J., & Day, C. (2013). Do evidence-based interventions work when tested in the “real world?” A systematic review and meta-analysis of parent management training for the treatment of child disruptive behavior. Clinical Child and Family Psychology Review, 16(1), 18–34
Nahmias, A. S., Pellecchia, M., Stahmer, A. C., & Mandell, D. S. (2019). Effectiveness of community-based early intervention for children with autism spectrum disorder: a meta‐analysis. Journal of Child Psychology and Psychiatry, 60(11), 1200–1209
Oono, I. P., Honey, E. J., & McConachie, H. (2013). Parent-mediated early intervention for young children with autism spectrum disorders (AUTISM). Evidence‐Based Child Health: A Cochrane Review Journal, 8(6), 2380–2479
Pickles, A., Le Couteur, A., Leadbitter, K., Salomone, E., Cole-Fletcher, R., Tobin, H., & Byford, S. (2016). Parent-mediated social communication therapy for young children with autism (PACT): Long-term follow-up of a randomised controlled trial. The Lancet, 388(10059), 2501–2509
Postorino, V., Sharp, W. G., McCracken, C. E., Bearss, K., Burrell, T. L., Evans, A. N., & Scahill, L. (2017). A systematic review and meta-analysis of parent training for disruptive behavior in children with autism spectrum disorder. Clinical Child and Family Psychology Review, 20(4), 391–402
Raulston, T. J., Hieneman, M., Caraway, N., Pennefather, J., & Bhana, N. (2019). Enablers of behavioral parent training for families of children with autism spectrum disorder. Journal of Child and Family Studies, 28(3), 693–703
Reichow, B. (2012). Overview of meta-analyses on early intensive behavioral intervention for young children with autism spectrum disorders. Journal of Autism and Developmental Disorders, 42(4), 512–520
Rosen, B., Waitzberg, R., & Merkur, S. (2015). Israel: Health System Review. Health Systems in Transition, 17 (6). World Health Organization, Copenhagen, on behalf of the European Observatory on Health Systems and Policies
Scahill, L., McDougle, C. J., Aman, M. G., Johnson, C., Handen, B., Bearss, K. … Stigler, K. A. (2012). Effects of risperidone and parent training on adaptive functioning in children with pervasive developmental disorders and serious behavioral problems. Journal of the American Academy of Child & Adolescent Psychiatry, 51(2), 136–146
Schreibman, L. (2000). Intensive behavioral/psychoeducational treatments for autism: Research needs and future directions. Journal of Autism and Developmental Disorders, 30(5), 373–378
Sinai-Gavrilov, Y., Gev, T., Mor-Snir, I., Vivanti, G., & Golan, O. (2020). Integrating the Early Start Denver Model into Israeli community autism spectrum disorder preschools: Effectiveness and treatment response predictors. Autism, 24(8), 2081–2093
Smith, T., & Iadarola, S. (2015). Evidence base update for autism spectrum disorder. Journal of Clinical Child & Adolescent Psychology, 44(6), 897–922
Smith, T., Scahill, L., Dawson, G., Guthrie, D., Lord, C., Odom, S. … Wagner, A. (2007). Designing research studies on psychosocial interventions in autism. Journal of Autism and Developmental Disorders, 37(2), 354–366
Sourander, A. (2015). Challenges in children’s enrolment to psychosocial services. European Child & Adolescent Psychiatry, 24(4), 361–363
Ura, S. K., Liao, C. Y., Ganz, J. B., Stein, K., & Clark, S. (2021). Parent-coaching telehealth intervention for youth with autism spectrum disorder: A pilot program. Child & Family Behavior Therapy, 43(2), 86–102
Vinen, Z., Clark, M., Paynter, J., & Dissanayake, C. (2018). School age outcomes of children with autism spectrum disorder who received community-based early interventions. Journal of Autism and Developmental Disorders, 48(5), 1673–1683
Vivanti, G., Kasari, C., Green, J., Mandell, D., Maye, M., & Hudry, K. (2018). Implementing and evaluating early intervention for children with autism: Where are the gaps and what should we do? Autism Research, 11(1), 16–23
Weber, E., Miller, S. J., Astha, V., Janevic, T., & Benn, E. (2020). Characteristics of telehealth users in NYC for COVID-related care during the coronavirus pandemic. Journal of the American Medical Informatics Association, 27(12), 1949–1954
Williams, S. K., Scahill, L., Vitiello, B., Aman, M. G., Arnold, L. E., McDougle, C. J., & Posey, D. J. (2006). Risperidone and adaptive behavior in children with autism. Journal of the American Academy of Child & Adolescent Psychiatry, 45(4), 431–439
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Tobi Graucher and Yana Sinai-Gavrilov contributed equally to this manuscript.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Graucher, T., Sinai-Gavrilov, Y., Mor, Y. et al. From Clinic Room to Zoom: Delivery of an Evidence-Based, Parent-mediated Intervention in the Community Before and During the Pandemic. J Autism Dev Disord 52, 5222–5231 (2022). https://doi.org/10.1007/s10803-022-05592-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-022-05592-1