Abstract
Depressive symptoms and personality traits covary in adolescents, but our understanding of the nature of this relation is limited. Whereas a predisposition explanation posits that specific personality traits increase the vulnerability for developing depression, a scar explanation proposes that depression may alter premorbid personality. Attempts to test these explanatory models have relied on analyses that conflate within-person changes and between-person differences, which limits the implications that can be drawn. Moreover, research on the early adolescent years is lacking. The present study therefore examined within-person associations between depressive symptoms and Big Five personality traits across ages 10 to 16. Children (n = 817; 49.9% boys) and parents from two birth cohorts in Trondheim, Norway, were assessed biennially with clinical interviews capturing symptoms of major depressive disorder and dysthymia, and self-reported Big Five personality traits. Analyses were conducted using a random intercept cross-lagged panel model, which accounts for all unmeasured time-invariant confounding effects. Increased Neuroticism predicted an increased number of depressive symptoms—and increased depressive symptoms predicted increased Neuroticism—across ages 10 to 14. Moreover, increased depressive symptoms forecast reduced Extraversion across ages 10 to 16, and reduced Conscientiousness from ages 12 to 14. Increases in Neuroticism may contribute to the development of depressive symptoms—in line with the predisposition model. As regards the scar model, depression may have an even wider impact on personality traits: increasing Neuroticism and reducing Extraversion and Conscientiousness. These effects may already be present in the earliest adolescent years.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Depressive disorders typically manifest during adolescence (e.g., Merikangas et al., 2010) and subsequently become among the most common mental disorders (World Health Organization, 2019). Even subclinical levels of depressive symptoms are associated with current and future adverse outcomes, including impaired functioning in family, school, and peer contexts, comorbid psychiatric disorders, and suicide (Bertha & Balázs, 2013; Gibb, 2014; Rudolph & Flynn, 2014). Clearly, it is crucial to identify factors involved in the development of adolescent depression, which could inform preventative and treatment efforts.
Among such factors, personality traits have been linked with psychopathology in general, and depression in particular, even in adolescents (Klimstra et al., 2010), which is the current focus. Personality traits, as measured using the Five Factor Model (FFM: John et al., 2008), encapsulate the higher-order traits of Neuroticism, Extraversion, Conscientiousness, Agreeableness, and Openness. These traits, which are also measured in the present study, have been identified in youths as young as 10 years of age (John et al., 2008; Soto et al., 2008).
The relation between personality traits and psychopathology is considered to be complex (see, e.g., Ormel et al., 2020; Tackett, 2006). From a theoretical perspective, six explanatory models have been proposed (e.g., De Bolle et al., 2012; Tackett, 2006). First, personality traits may be a risk factor for psychopathology (i.e., the vulnerability/predisposition model) or influence how a given disorder manifests itself (i.e., the pathoplasty/exacerbation model) (e.g., Ormel et al., 2013, 2020). The first model implies that personality initiates processes that increase the risk of developing a particular disorder. For example, low scorers on Extraversion tend to experience less social support (Swickert et al., 2002), which increases the risk of depression (Rueger et al., 2016). The second model targets developmental aspects of the disorder itself, such as severity or duration (see Klein et al., 2011).
By contrast, the scar model posits that an existing Axis 1 disorder may cause changes in personality that persist when the depression is no longer present (De Bolle et al., 2012; Laceulle et al., 2014; Ormel et al., 2013, 2020; Tackett, 2006). A scar example may be an increased tendency to ruminate even after depression has subsided (Krause et al., 2018), and rumination is associated with higher levels of Neuroticism (Slavish et al., 2018). Notably, if an individual in remission from a major depressive episode does not return to their baselevel of, for example, Neuroticism after a certain period, the disorder may have left a scar, although not necessarily a permanent scar. Alternatively, depression may cause more temporary changes, as in the fourth, complication model (e.g., Ormel et al., 2020).
The two final models target third variables causing both personality traits and psychopathology, thus producing spurious correlations. The fifth model is the spectrum/continuity model, which implies that psychopathology and personality traits are different manifestations along the same continuum (De Bolle et al., 2012). For example, high levels of Neuroticism have been equated with depressive symptoms (Ormel et al., 2013). Closely related, although methodologically difficult to separate (Ormel et al., 2020), the sixth and final model—the common-factor model— highlights that psychopathology and personality traits have the same causal factors.
In the present study, we focus on the predisposition and scar explanations for the relation between depressive symptoms and the Big Five personality traits in adolescence. From a methodological standpoint, when examining longitudinal predictions as we aim to do in this study, several developmentalists recommend statistical methods that distinguish between- and within-person information (e.g., Hamaker et al., 2015; Hamaker et al., 2020; Lervåg, 2020). We argue that the predisposition and scar models are indeed within-person questions of nature (see Hamaker et al., 2020, for a conceptual discussion). Whereas between-person information concerns the extent to which adolescents’ personality traits covary with their depression level (e.g., if those who score high on Neuroticism also score high on depression), within-person information concerns whether an adolescent whose personality changes will experience a change in depression (or vice versa). Numerous scholars have highlighted the potential pitfalls of using between-person information to test hypotheses about within-person changes. This practice, known as the ecological fallacy, can lead to incorrect results because associations observed at the population level may not hold true at the individual level (Curran & Bauer, 2011). One commonly used approach in developmental research is the Cross-Lagged Panel Model (CLPM). However, the cross-lagged paths in CLPM represent a conflation of between-person and within-person information, which makes interpretation challenging (Berry & Willoughby, 2017). Moreover, because time-invariant between-person effects can confound the estimates of cross-lagged parameters, the use of CLPM to examine developmental questions, has been advised against (see, e.g., Lervåg, 2020).
Confounding effects may stem from, for example, the shared genetic vulnerability for depression and Neuroticism (e.g., Kendler et al., 2019), or trait-like parenting factors such as emotional warmth, associated with both depression (Yang et al., 2008) and Extraversion (Li et al., 2021).
In contrast, more recent statistical advancements allow the disentangling of the between- and within-person information (Usami, 2023). These methods, including the Random Intercept Cross-Lagged Panel Model (RI-CLPM: Hamaker et al., 2015) applied herein, use the participants as their own controls, thus accounting for time-invariant confounding effects (Berry & Willoughby, 2017). Evidently, however, observational studies, including those using within-person methods, do not meet all the assumptions for a causal relation (Mund & Nestler, 2019). For example, time-varying confounding remains (Berry & Willoughby, 2017). Therefore, within-person predictions may only inform on the likelihood of etiology and cannot be causally interpreted. Nevertheless, to advance research on the personality-depression models, within-person approaches are called for, but no such study exists.
Further, due to the significant increase in the prevalence of depression around the ages of 12 to 13 (see, e.g., Morken et al., 2020), it is important to assess potential precursors of depression before this increase occurs. However, previous studies mainly include participants from age 12. One exception is a study that followed a sample from age 10 over the course of 18 months (Zhang et al., 2020). To bridge these gaps in the literature, we therefore apply the RI-CLPM to four waves of data from a cohort that was followed biannually from ages 10 to 16. Moreover, with one exception (Goldstein et al., 2018, 2020), prior research has relied on self-report questionnaires for both depressive symptoms and personality traits, which is likely to have inflated the prospective relations between the two (Klein et al., 2011). We, however, use clinical interviews for capturing depressive symptoms and self-reports of personality traits, thus limiting the risk of common method bias.
To inform on the predisposition and scar models, which are the focus of the present study, existing prospective research—on both adolescents and adults—has applied CLPMs (e.g., Hakulinen et al., 2015; Klimstra et al., 2010). A meta-analysis of longitudinal studies on adult samples concluded that high Neuroticism, low Extraversion, and low Conscientiousness predicted depression (Hakulinen et al., 2015), which is in line with the predisposition model. The evidence indicating support for the scar model was even stronger, as depression predicted changes in all traits: higher Neuroticism and lower Extraversion, Conscientiousness, Agreeableness, and Openness (Hakulinen et al., 2015). In contrast to relatively stable rates in adulthood (Richards, 2011), the prevalence of depression changes from being infrequent in childhood to substantially increasing in adolescence (Morken et al., 2020). Moreover, adolescence is a time for considerable personality development (Soto et al., 2011). For example, Neuroticism temporarily increases in early to middle adolescence—at least in girls—and Conscientiousness and Agreeableness decline from late childhood into early adolescence, before increasing in later adolescence (Soto et al., 2011). Given these developmental changes in personality and depression, evidence in line with the predisposition and scar models in adults may not generalize to adolescents—or even across adolescence. Therefore, we aim to investigate reciprocal associations between depression and personality traits in adolescents while testing for developmental differences. This will be carried out in this 4-wave longitudinal study, following a cohort from ages 10 to 16.
There are fewer studies that investigate the association between depression and personality in adolescence. Some of these focus on internalizing symptoms that are measured more broadly and temperamental traits (e.g., Laceulle et al., 2014; Ormel et al., 2020). In the following, we will review studies that analyze the relation between depressive symptoms and the Big Five personality traits. To the best of our knowledge, there are seven such longitudinal studies on adolescents that are relevant for the predisposition model. All apply the CLPM approach. Whereas six of these reported that higher levels of Neuroticism predicted higher levels of depression (Calvete et al., 2016; Goldstein et al., 2020; Kercher et al., 2009; Klimstra et al., 2010; Yang et al., 2008; Zhang et al., 2020), one found that higher Neuroticism predicted lower levels of depression (Williams et al., 2021). With regard to Extraversion and Conscientiousness, one study chronicled adolescents with low scores on these traits to be at increased risk of depression (Klimstra et al., 2010). However, others have not found that Extraversion (Calvete et al., 2016; Goldstein et al., 2018; Yang et al., 2008) or Conscientiousness (Goldstein et al., 2018) predicted depression. Neither Agreeableness nor Openness have been found to predict depression (Goldstein et al., 2018; Klimstra et al., 2010). Because the Big Five personality traits have been shown to correlate (Van der Linden et al., 2010), some have partialled out the common variance by examining several traits in multivariate models, finding that only Neuroticism uniquely predicted depression (Goldstein et al., 2018; Yang et al., 2008). As such, Neuroticism should be accounted for when examining the other four traits, which will be done in the present study.
Two studies on adolescents have examined predictions from depression on the Big Five personality traits—thus informing the scar model. One of these investigated all five traits in separate models, and reported that depressive symptoms predicted higher levels of Neuroticism, and lower degrees of Extraversion, Conscientiousness, and Agreeableness (Klimstra et al., 2010). The other study only included neuroticism and found that depression predicted higher levels of this (Zhang et al., 2020).
Current Study
This study examines the predisposition and scar explanations for the relation between depressive symptoms and the Big Five traits by—for the first time—applying a within-person approach and including participants younger than age 12. We measure symptoms of major depressive disorder (MDD) and dysthymia by means of clinical interviews in biennial follow-ups of a birth cohort sample from ages 10 to 16. To the extent that prior CLPM findings hold for within-person changes, as analyzed with RI-CLPM, we hypothesize that increased depression will predict increased neuroticism and decreased extraversion, conscientiousness, and agreeableness. Although the meta-analysis on adults found that depression predicted lower levels of openness (Hakulinen et al., 2015), the only study to investigate this in adolescents did not find this prediction (Klimstra et al., 2010). Collectively, we pose no specific scar hypotheses for openness. The present study is the first to explore potential developmental differences across adolescence in the predisposition and scar explanations.
Methods
Participants and Procedure
The Trondheim Early Secure Study (TESS) (Steinsbekk & Wichstrøm, 2018) comprises children from the 2003 and 2004 birth cohorts in Trondheim, Norway (N = 3,456). A letter of invitation, together with the Strengths and Difficulties Questionnaire (SDQ) version 4–16 (Goodman et al., 2000), was sent to the children’s homes prior to the age-4 routine health check-up. Almost all parents and their children attended the check-up (n = 3,358). Parents were informed orally and in writing about the TESS by a health nurse, and written consent was obtained. At age 12 the children were specifically informed about the study, and at age 16 they provided their own consent. Study procedures were approved by the Regional Committee for Medical and Health Research Ethics, Mid-Norway (approval number 2009/994).
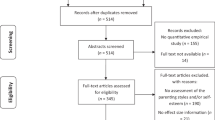
To increase statistical power, children with emotional and behavioral problems were oversampled at baseline. To accomplish this, children were divided into four strata based on their SDQ score (0–4, 5–8, 9–11, 12–40), and the probability of being selected increased with increasing scores (37%, 48%, 70%, and 89%, from the respective strata). This oversampling was accounted for in the analyses. The drop-out rate after the provision of consent at the well-child clinic did not differ across the four SDQ strata (χ2(3) = 5.70, p = 0.127) or by sex (χ2(1) = 0.23, p = 0.973). Of the 1,250 children randomly selected for the study, 1,007 were successfully enrolled at Time 1 (Mage = 4.59, SD = 0.25; 49.1% boys) (for a flowchart of recruitment and follow-ups, see Online Supplemental Material Fig. S1). Given that our research questions pertained to explaining depression during adolescence, we included data from ages 10 (T4: Mage = 10.51, SD = 0.17), 12 (T5: Mage = 12.50, SD = 0.14), 14 (T6: Mage = 14.35, SD = 0.14), and 16 (T7: Mage = 16.98, SD = 0.31). Participants with information from at least one data wave comprised the analytical sample (n = 817).
Overall, attrition was unrelated to the study variables, with the exception that more symptoms of MDD (OR = 1.39, 95% CI [1.15, 1.70]) and dysthymia (OR = 1.35, 95% CI [1.12, 1.64]) at age 12 predicted attrition at age 14. Although the analyses suggested some selective attrition, they should be interpreted according to the number of attrition analyses conducted. An overall test—the Little Missing Completely at Random (MCAR) test (Little, 1988)—was therefore conducted. The results confirmed that data was not missing completely at random: χ2(1286.46, df = 935, p < 0.001). The normed test was 1.38, which is below the suggested cut-off of 2 (Ullman et al., 2001), and this indicates that data was missing at random (MAR). Demographic characteristics of the sample are presented in Table 1. Mean levels of symptoms of depression and mean levels of personality traits are presented in Table 2. The percentage of children and adolescents at each wave with x number of symptoms is presented in Online Supplemental Tables S1 and S2. Most participants (> 60%) in each wave were symptom-free, and most of those with depressive symptoms had a subclinical number of symptoms.
Measures
Depressive symptoms were measured as symptoms of MDD and dysthymia, as defined by the Diagnostic and Statistical Manual of Mental Disorders (DSM) and by using semi-structured psychiatric interviews. Symptoms of MDD were defined according to DSM-IV (American Psychiatric Association [APA], 1994) (the first data-wave) and DSM-5 (APA, 2013) (the following data-waves). Symptoms of dysthymia were defined according to DSM-IV in the first wave. In the last three waves, when DSM-5 had been introduced, the diagnosis Persistent Depressive Disorder (PDD) was introduced. PDD includes dysthymia, but also, for example, the possibility that MDD may be continuously present. DSM-5 allows for specification of “pure dysthymic syndrome”, and the symptoms described are the same as those described as dysthymia in DSM-4. We therefore measured the same symptoms across ages, and use the term dysthymia throughout this paper. Children and parents were interviewed separately. A symptom was considered present if it was reported to occur during the last three months by either respondent. To capture dysthymia, which should have an onset at least one year prior, we also asked for the first onset of these symptoms. The core symptoms had to be present concurrently with the other symptoms for the latter to be coded as present. At ages 10, 12, and 14, the Child and Adolescent Psychiatric Assessment (CAPA: Angold & Costello, 2000) was applied. Inter-rater reliabilities among blinded coders of 15% of audiotapes of CAPA interviews at age 10 were ICC = 0.87 for MDD symptoms and ICC = 0.85 for dysthymia symptoms. At age 16, the Schedule for Affective Disorders and Schizophrenia for School-Age Children (K-SADS: Kaufman et al., 2016) was applied. A symptom was considered present at the threshold (coded as 3), as this coincides with the DSM. Inter-rater reliabilities among blinded coders of 17% of audiotapes of K-SADS interviews were ICC = 0.81 for MDD symptoms and ICC = 0.76 for dysthymia symptoms. Symptom count scores based on the CAPA and the K-SADS were created as the sum of MDD and dysthymia symptoms.
Personality traits were measured by the Norwegian version of the self-reported Big Five Inventory (BFI: Soto et al., 2008), which consists of 44 items capturing Neuroticism (8 items), Extraversion (8 items), Conscientiousness (9 items), Agreeableness (9 items) and Openness (10 items). Response options range from 1 (disagree) to 5 (agree). In the present sample, the internal consistencies at ages 10, 12, 14, and 16, respectively, were as follows: Neuroticism: α = 0.59, 0.72, 0.81, 0.83; Extraversion: α = 0.54, 0.67, 0.75, 0.81; Conscientiousness: α = 0.65, 0.72, 0.77, 0.76; Agreeableness: α = 0.64, 0.71, 0.72, 0.71; Openness: α = 0.69, 0.74, 0.74, 0.76.
Sociodemographic information on child and parent was reported by the parent during the CAPA-interview. Sex assignment was 0 = boy and 1 = girl based on the child’s national identification number, in which the child’s biological sex at birth is registered.
Statistical Analyses
Prospective relations were examined with a Random-Intercept Cross-Lagged Panel Model (RI-CLPM), in which within-person variance is separated from between-person variance (Hamaker et al., 2015). As regards measurement variance, the level of depression (Merikangas et al., 2010) and personality traits (Soto et al., 2011) are reported to change during adolescence. Hence, scalar invariance was neither envisioned nor analyzed. Metric invariance for depression has previously been documented in the current sample from ages 4 to 14 (Morken et al., 2020). We therefore only examined the metric invariance from ages 14 to 16, setting factor loadings to be equal over time. We also investigated metric invariance of the BFI. Given that all factors across all ages did not converge, each factor was examined separately. We applied Chen’s (2007) criteria for metric invariance (i.e., ΔCFI ≥ -0.010, ΔRMSEA ≥ 0.015, ΔSMR ≥ 0.030).
DSM-5 conceptualizes depressive disorders to be one-dimensional; thus for depression, configural invariance was not considered. A complete test of configural invariance for the Big Five across all time points did not converge. We therefore examined whether the 5-factor solution had an adequate fit at all ages, as others have found an adequate fit for the 10-year-olds, but only when adjusting for acquiescence bias (Soto et al., 2008). Therefore, we also considered the factor structure after adjusting for acquiescence bias, according to the procedure described by Soto et al. (2008).
At each wave, the observed depressive symptoms and personality trait scores were decomposed into a stable between-person part and a varying within-person part. In each model, one random intercept factor for depression and one for the personality trait in question were created, thereby capturing the participants’ overall levels of the two constructs. The factor loadings to the respective observed variables were set at 1. One latent variable was defined for each observed variable with the variance in the observed variable set to 0 and with a factor loading of 1, thereby transferring the variance to the corresponding latent variable. In effect, the latent depression and personality trait variables at each time point (t) capture the adolescent’s deviation from her or his own mean score across time. These latent deviations at t were regressed on the latent changes at t-1. Concurrent correlations between the error terms of these latent variables were allowed.
Because the RI-CLPM is power-demanding (e.g., Masselink et al., 2018), we examined the relation between depressive symptoms and each of the personality traits in five separate models. However, previous studies that have examined several traits in multivariate models have found that only Neuroticism uniquely predicted depression (Goldstein et al., 2018; Yang et al., 2008). We therefore examined the paths to and from Extraversion, Conscientiousness, Agreeableness, and Openness, adjusting for Neuroticism. Importantly, prior research has identified a female preponderance in depression by at least age 12 (Salk et al., 2017), and in early adolescence neuroticism increases in girls and may slightly decrease in boys (e.g., Soto et al., 2011). Because our sample size (n = 817) was somewhat lower than the recommended size for an RI-CLPM (Masselink et al., 2018), we were not positioned to analyze girls and boys separately.
To examine developmental effects in the predisposition and scar models, we tested whether a model where the cross-lagged paths were set to be equal across all ages fitted the data worse than a model where the paths between depression and personality traits were freely estimated, using the Satorra-Bentler Scaled Chi-square Difference Test (Satorra & Bentler, 2001). If a model in which cross-lagged paths were set to be equal did not deteriorate the model fit, we would prefer such a constrained model for parsimonious reasons. This would indicate no difference in the strength of the cross-lagged paths across age, regardless of whether the paths were statistically significant or not.
Note that in order to facilitate comparison between our results and former inquiries in which Neuroticism was not accounted for, we also estimated RI-CLPMs without this covariate. Finally, to compare our findings with previous CLPM-results—and thus inform on the impact of time-invariant confounding effects—we reran the main models using a CLPM.
All analyses were performed in Mplus 8.5, using a robust maximum likelihood estimator and population weights to correct for the oversampling of children with mental health issues. Missing data was handled using a Full Information Maximum Likelihood (FIML) procedure under the assumption that data was MAR.
Results
Across all ages, depressive symptoms correlated positively with Neuroticism, and negatively with Extraversion, Conscientiousness, and Agreeableness (see Online Supplemental Tables S3–S17). These four traits also correlated with each other. The bivariate associations were mostly of weak effect sizes. There were, however, a few exceptions at single measurement points, and the associations between Conscientiousness and Agreeableness were positive and of moderate effect sizes across ages 10 to 14, and weak at age 16. The correlations between the random intercepts between the latent depression constructs and the five personality traits respectively were as following: Neuroticism r = 0.43 (p = 0.011), Extraversion r = -0.39 (p = 0.006), Conscientousness r = -0.49 (p = 0.009), Agreeableness r = 0.38 (p = 0.042) and Openness r = 0.12 (p = 0.545). See Online Supplemental Table S18 for the correlated time-specific residual terms. MDD evinced metric invariance, except that suicidality was more of a defining feature of MDD at age 16 than at age 14. As for dysthymia and the BFI, full metric invariance was achieved. The BFI did not demonstrate full configural invariance. As the appropriateness of a 5-factor model for 10-year-olds was of most concern, the model fit of this solution was examined with a Confirmatory Factor Analysis (CFA) at age 10. All items loaded significantly on their respective factors, except for two Extraversion items (“reserved; keeps thoughts and feelings to self” and “tends to be quiet”). Even so, the model fit was not adequate, according to fit statistics. The model fit further deteriorated when adjusting for aquiescence bias. See Supplemental Material Measurement invariance for more information, including Table S19.
Predisposition Model
Increased Neuroticism at ages 10 and 12 forecasted an increased number of symptoms of depression two years later, at 12 and 14, respectively (Table 3). From ages 14 to 16, no effect was observed. Changes in the other four traits, adjusted for Neuroticism, were unrelated to future changes in depression (Table 3). As regards possible developmental differences, a model where the cross-lagged paths from Neuroticism to depressive symptoms were set to be equal from ages 10 to 14—whereas the path from age 14 Neuroticism to age 16 depression could vary (i.e., set to be free)—fitted the data equally well as a freely estimated model (Table 4). Thus, the relations were similar across the first two lags and differed from ages 14 to 16. For the other four personality traits, models in which cross-lagged paths from personality to depression were fixed across ages fitted the data equally well as freely estimated models (Table 4). These latter results indicate that the impact of personality traits on depression might not vary across the investigated age period. Notably, when adjusting for Neuroticism in these models, we allowed the path from Neuroticism to depression to be freely estimated from ages 14 to 16, in accordance with the model fit results in the depression-Neuroticism model.
When rerunning the RI-CLPM without adjustment for Neuroticism, the results on Neuroticism were replicated (Table S20). Additionally, increased Agreeableness predicted reduced depression across ages 10 to 16 (Table S21). The results on developmental effects echoed the original RI-CLPM models (Table S21).
Finally, we reran the models with CLPM. Again, our original RI-CLPM findings on Neuroticism (Table S22) and the results on developmental effects (Table S23) were replicated. However, in the CLPM models, Openness predicted depression across all ages (Table S22).
Scar Model
When examining scar models, increased number of depressive symptoms predicted increased levels of both Neuroticism and Conscientiousness from ages 10 to 12 and 12 to 14, whereas no effects were observed from ages 14 to 16 (Table 3). Furthermore, increases in depressive symptoms predicted reduced levels of Extraversion across all lags (Table 3). Increases in depressive symptoms were unrelated to future changes in Agreeableness and Openness (Table 3). As for developmental differences, the path from depression at age 14 on Neuroticism differed from the previous age-lags (Table 4). The paths from Conscientiousness on depression varied across ages. For the models on Extraversion, Egreeableness, and Openness in which cross-lagged panel effects were set to be equal mostly fitted the data as well as the models in which these effects were allowed to vary (i.e., indicating no developmental differences) (Table 4). Yet again, when adjusting for Neuroticism, the path from depression to Neuroticism was freely estimated from ages 14 to 16.
When we reran the RI-CLPM models without controlling for Neuroticism, the results were similar, with two exceptions. Depressive symptoms predicted reduced Agreeableness from ages 10 to 12, and reduced Conscientiousness from ages 10 to 12 (and not from ages 12 to 14, as in the original results) (Table S20). Regarding developmental differences, in addition to the 14–16 age span from depression to Neuroticism differing from previous ages, and the paths from Conscientiousness differing across ages, the paths from depression on Agreeableness also varied across all ages (Table S21).
When we reran the models with CLPM, the results echoed our original RI-CLPM results except that depression additionally predicted reduced Conscientiousness and reduced Agreeableness from ages 10 to 12 (Table S22). The path for Agreeableness from ages 10 to 12 differed from the later ages (Table S23). Thus, two apparent scar mechanisms were demonstrated with CLPM that did not appear with the RI-CLPM.
Discussion
Although it has been long established that depressive symptoms and personality traits covary in adolescence (e.g., Klimstra et al., 2010), the understanding of this relation is limited. Two common explanations are that personality traits can pose a vulnerability for depression, and/or that depression may impact personality traits (i.e., ‘scars’). However, prior research examining these predisposition and scar explanations have all applied traditional regression-type or CLPM analyses. These approaches cannot answer whether changes in personality forecast changes in depression (or vice versa) at the level of the individual. Therefore, and for the first time, we tested the predisposition and scar explanations by applying within-person methodology in a representative community sample, using adolescents as their own controls. We identified a reciprocal relation between depressive symptoms and Neuroticism across ages 10 to 14, in line with both predisposition and scar models. Moreover, increases in depressive symptoms predicted decreased levels of Extraversion throughout ages 10 to 16, and decreased levels of Conscientiousness from ages 12 to 14, in accordance with a scar model. There were no significant within-person paths involving Agreeableness or Openness. Besides the 14–16 age span for Neuroticism, and the predictions from Conscientiousness to depression that varied across ages 10 to 16, we did not find developmental differences in the relations between depression and the personality traits.
Reciprocal Relations Between Depression and Neuroticism
First and foremost, our results demonstrate a reciprocal within-person relation between Neuroticism and depressive symptoms across ages 10–12 and 12–14, which indicates support for both the predisposition and the scar models. This extends earlier CLPM findings to the within-person level and already from the age of 10 (Calvete et al., 2016; Goldstein et al., 2020; Kercher et al., 2009; Klimstra et al., 2010; Yang et al., 2008; Zhang et al., 2020).
Establishing reciprocal within-person predictions between depression and Neuroticism is only a first step to understanding this relation. Although our study does not inform on the mechanisms involved, prior research does allude to some possibilities. Adolescents scoring high on Neuroticism might experience more stress, which is a risk factor for depression (Ge et al., 1994). For example, Tian et al. (2019) found that the impact of high levels of Neuroticism on depression was mediated by perceived school stress. Relatedly, when faced with stress, adolescents scoring high on Neuroticism may be more prone to use emotional regulation strategies such as rumination and self-blame (Liu et al., 2020) or emotional suppression (Yoon et al., 2013). Both studies found that these strategies increased the risk for depression.
Contrary to our hypotheses, there were no significant paths between depression and Neuroticism from ages 14 to 16. This is in contrast to a CLPM study on the predisposition model in an age group comparable to ours, that did find that Neuroticism predicted depression (Goldstein et al., 2020). Our null-finding might be explained by the change in the depression measure from ages 14 to 16 (detailed above and in the limitations section). However, metric invariance was established. In that sense, we cannot rule out that this (null) finding is substantial. Alternatively, Neuroticism may lead to transitional increases in depressive symptoms (see, e.g., Ormel et al., 2013), or, depression might lead to temporary changes in personality (Ormel et al., 2020). Thus, a possibility is that the relation between depression and Neuroticism exists in mid-adolescence as well, but perhaps over shorter time spans than captured by our two-year lags. Changes in both depression and Neuroticism after the age 14 assessment could have receded before the age 16 assessment. Future and more intensive longitudinal within-person research could help illuminate these possibilities.
Depressive Symptoms Predicted Reduced Extraversion and Conscientiousness
Beyond our study providing support for the scar model for Neuroticism, we also found increased number of depressive symptoms to predict reduced Extraversion. By using an within-person approach, our study extends similar findings using the CLPM (Klimstra et al., 2010). Moreover, by including participants younger than age 12, we were positioned to capture the period before the prevalence of depression increases (e.g., Morken et al., 2020). Also, we found that the predictions from depression to Extraversion were equal across ages 10 to 16, which indicates no developmental differences. It is possible that symptoms of depression (e.g., fatigue, feelings of worthlessness, loss of interest) directly curb the frequency and quality of social interactions (e.g., social withdrawal, insecurity in social settings), and for this reason forecast a decline in Extraversion. Another potential mechanism might involve erosion of social support (Coyne, 1976). Depressed individuals have been found to evoke social rejection (Segrin & Dillard, 1992)—possibly due to excessive reassurance-seeking (Starr & Davila, 2008). Thus, depressed adolescents may experience rejection when they do seek social support, thereby reinforcing their negative self-beliefs and further sustaining social withdrawal, as reflected in low Extraversion.
Further, we found increased depressive symptoms to forecast reduced Conscientiousness across ages 12 to 14—again in accordance with the scar model. Potential mechanisms could involve reduced executive functioning. Recent findings suggest that depression may diminish cognitive flexibility over time (Halse et al., 2022), and cognitive flexibility has been associated with lower Conscientiousness (e.g., Fleming et al., 2016). However, prospective studies are needed to determine whether an effect of depression on Conscientiousness is mediated through reduced cognitive flexibility, and why this should occur only in the 12–14 age span. Notably, however, we cannot rule out the possibility of scar-effects on Conscientiousness occurring before age 12 and after age 14, which could be more transient than this two-year measurement span could capture.
As hypothesized, neither reduced Extraversion nor Conscientiousness predicted depression. Thus, only the scar—but not the predisposition—explanation was supported for these traits. Our findings are in line with previous studies using the CLPM (Calvete et al., 2016; Goldstein et al., 2018; Yang et al., 2008), with one exception: Klimstra et al. (2010) reported that both low Extraversion and Conscientiousness predicted depression. In contrast to the current study and two of the former studies using the CLPM (Goldstein et al., 2018; Yang et al., 2008), Klimstra et al. (2010) did not control for Neuroticism. However, when we examined the models without accounting for Neuroticism, our null findings remained.
Agreeableness and Openness
Finally, depression was not predicted by—or did not predict—changes in Agreeableness or Openness. Thus, the predisposition and scar models were not supported. Previous studies using the CLPM also indicate nonexistent reciprocal relations between depression and these traits (Goldstein et al., 2018; Klimstra et al., 2010), with one exception: Klimstra et al. (2010) found that higher levels of depression predicted lower levels of Agreeableness, yet again without accounting for Neuroticism. Interestingly, when we reran the RI-CLPMs without controlling for Neuroticism, as well as with CLPMs, depressive symptoms did predict Agreeableness—but only from ages 10 to 12. In the age groups overlapping with Klimstra et al. (2010) (age 12 and onward), we still did not find a scar-effect. It is therefore unclear why our findings diverge from those of Klimstra et al. (2010).
Limitations
This study had a range of strengths, including a representative cohort sample, repeated assessments throughout ages 10 to 16, investigating the predisposition and scar models at the within-person level, and testing for developmental differences. Furthermore, to limit common method effects, symptoms of MDD and dysthymia were assessed by clinical interviews with both adolescents and parents, while personality traits were assessed by self-report questionnaires. Nevertheless, we acknowledge several important limitations.
First, adolescents with more depressive symptoms at age 12 more often dropped out of the study by age 14, which could potentially result in the underestimation of the increase in depressive symptoms during this period. However, considering that our prime interest was associations—and that we applied an FIML approach to missingness—we consider the possibility that factors associated with selective attrition interacted with study variables to produce the current results to be modest. Second, although we adjusted for time-invariant confounding effects, time-varying effects—such as stronger genetic effects in one age period than another (e.g., Kwong et al., 2021)—may still have influenced both changes in depressive symptoms and personality traits, and may therefore have produced spurious relations between them. Third, we captured depressive symptoms occurring in the prior three-month period. The three-month period in the CAPA was chosen because of concerns about the reliability of the children’s and parents’ memories over a longer time period (Angold & Costello, 2000), which was based on research showing that this reliability falls steeply after three to five months (Angold et al., 1996). Although not reported explicitly, there is probably a similar logic behind the choice of the three-month period in the K-SADS. However, this interval means that symptoms of MDD occurring between our 2-year intervals of observation may have been missed (i.e., lower validity). As such, the relation between depression and personality traits may have been underestimated, and/or null findings could represent Type II errors.
Fourth, from ages 14 to 16, we changed the clinical interview used to measure depressive symptoms from CAPA to K-SADS. The K-SADS has somewhat stricter criteria in that a depressive symptom must have been present for most of the day/at least 50% of the day—whereas in the CAPA, the symptom must have been present for at least one hour per day. This may have contributed to the apparent decrease in the mean number of depressive symptoms from ages 14 to 16 (Table 2)—thereby contradicting previous research that shows an increase in depressive symptoms during this age period (Merikangas et al., 2010). The lower mean level may have influenced the results by reducing statistical power, and thus increasing the risk of false negative cross-lagged relations from age 14 personality to depressive symptoms at age 16. Fifth, the current study focused on depressive symptoms only, although many children and adolescents have comorbid conditions such as anxiety disorders (Sharma et al., 2019) and attention-deficit/hyperactivity disorder (ADHD) (Sandstrom et al., 2021). Our study was not able to discern whether the results would, for example, differ according to different comorbidities. Relatedly, time-varying third-variable explanations for the longitudinal explanations (e.g., anxiety symptoms) cannot be ruled out.
Sixth, the moderate reliability of the BFI at age 10 is in line with research in adolescents from the USA and Canada (Soto et al., 2008). We also identified metric invariance. Complete configural invariance, however, could not be demonstrated, and adjusting for acquiescence bias (see Soto et al., 2008) did not improve the model fit. Possibly, such bias may operate differently across cultures, and/or the child’s overall intellectual capacity may be just as important. In a European sample, such as the present, Allik et al. (2004) reported that self-reports of Big Five traits (measured with a NEO inventory) were linked with intelligence among young adolescents (n = 2,650). This effect disappeared with increasing age. Notwithstanding, the uncertainty of our findings is somewhat higher from ages 10 to 12 than at later ages—that is, lack of associations might represent Type II errors, and the strength of the detected associations might have been underestimated.
Seventh, because the Big Five personality traits correlate (Van der Linden et al., 2010), our results might not reflect the unique contribution from each trait. Because RI-CLPM is power-demanding (Masselink et al., 2018), we were only able to adjust for the most likely candidate of confounding—Neuroticism (Goldstein et al., 2018). Eight, Norway is a country with low rates of psychiatric disorders (Bøe et al., 2021; Wichstrøm et al., 2012), and our sample may differ from contexts with overall lower and more variation in socioeconomic status and more ethnic diversity. Accordingly, the results might not be generalized to such populations, and replications in more diverse countries are needed.
Finally, we emphasize that, even though within-person approaches are endorsed in developmental psychopathology (e.g., Lervåg, 2020), there has been some criticism. Lüdtke and Robitzch (2021) proposed that a person’s temporary fluctuations around the mean (analyzed in the RI-CLPM) might offer limited insights, in contrast to the impact of factors that elucidate the variations among individuals (analyzed in the CLPM). However, this an ongoing debate, which in the years to come may further advance longitudinal analyses.
Conclusions
This is the first within-person study—of any developmental age group—to examine the predisposition and scar explanations for the relation between depression and personality. We found evidence for within-person associations between depressive symptoms and the Big Five personality traits from age 10 onwards. The results showed reciprocal relations between depressive symptoms and Neuroticism across ages 10 to 14, which is in line with both the predisposition and scar models. Moreover, increased depressive symptoms predicted lower Extraversion across ages 10 to 16 and lower Conscientiousness from ages 12 to 14, which is in line with the scar model. The strength of the relations between depression and personality traits mostly did not vary across age. Our findings indicate that preventive and treatment efforts should consider high levels of Neuroticism as a potential vulnerability factor for depressive symptoms. Moreover, the finding that depressive symptoms may alter early adolescents’ personality traits underlines the importance of preventing depression a at this age.
Materials and/or Code Availability
Due to conditions for consent from participants, data cannot be shared.
References
Allik, J., Laidra, K., Realo, A., & Pullmann, H. (2004). Personality development from 12 to 18 years of age: Changes in mean levels and structure of traits. European Journal of Personality, 18(6), 445–462.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (DSM-IV). American Psychiatric Pub.
Angold, A., & Costello, E. J. (2000). The child and adolescent psychiatric assessment (CAPA). Journal of the American Academy of Child & Adolescent Psychiatry, 39(1), 39–48. https://doi.org/10.1097/00004583-200001000-00015
Angold, A., Erkanli, A., Costello, E. J., & Rutter, M. (1996). Precision, reliability and accuracy in the dating of symptom onsets in child and adolescent psychopathology. Journal of Child Psychology and Psychiatry, 37, 657–664. https://doi.org/10.1111/j.1469-7610.1996.tb01457.x
Berry, D., & Willoughby, M. T. (2017). On the practical interpretability of cross-lagged panel models: Rethinking a developmental workhorse. Child Development, 88(4), 1186–1206. https://doi.org/10.1111/cdev.12660
Bertha, E. A., & Balázs, J. (2013). Subthreshold depression in adolescence: A systematic review. European Child & Adolescent Psychiatry, 22(10), 589–603. https://doi.org/10.1007/s00787-013-0411-0
Bøe, T., Heiervang, E. R., Stormark, K. M., Lundervold, A. J., & Hysing, M. (2021). Prevalence of psychiatric disorders in Norwegian 10–14-year-olds: Results from a cross-sectional study. PLoS ONE, 16(3), e0248864. https://doi.org/10.1371/journal.pone.0248864
Calvete, E., Orue, I., & Gamez-Guadix, M. (2016). Do extraversion and neuroticism moderate the association between bullying victimization and internalizing symptoms? A three-wave longitudinal study. Journal of School Psychology, 56, 1–11. https://doi.org/10.1016/j.jsp.2016.02.003
Chen, F. F. (2007). Sensitivity of goodness of fit indexes to lack of measurement invariance. Structural Equation Modeling: A Multidisciplinary Journal, 14(3), 464–504. https://doi.org/10.1080/10705510701301834
Curran, P. J., & Bauer, D. J. (2011). The disaggregation of within-person and between-person effects in longitudinal models of change. Annual Review of Psychology, 62, 583–619. https://doi.org/10.1146/annurev.psych.093008.100356
Coyne, J. C. (1976). Depression and the response of others. Journal of Abnormal Psychology, 85(2), 186–193. https://doi.org/10.1037/0021-843X.85.2.186
De Bolle, M., Beyers, W., De Clercq, B., & De Fruyt, F. (2012). General personality and psychopathology in referred and nonreferred children and adolescents: an investigation of continuity, pathoplasty, and complication models. Journal of Abnormal Psychology, 121(4), 958–970. https://doi.org/10.1037/a0027742
Fleming, K. A., Heintzelman, S. J., & Bartholow, B. D. (2016). Specifying associations between conscientiousness and executive functioning: Mental set shifting, not prepotent response inhibition or working memory updating. Journal of Personality, 84(3), 348–360. https://doi.org/10.1111/jopy.12163
Ge, X., Lorenz, F. O., Conger, R. D., Elder, G. H., & Simons, R. L. (1994). Trajectories of stressful life events and depressive symptoms during adolescence. Developmental Psychology, 30(4), 467–483. https://doi.org/10.1037/0012-1649.30.4.467
Gibb, B. E. (2014). Depression in children. In I. Gotlib, H. & C. Hammen, L. (Eds.), Handbook of depression (3rd ed., pp. 374–390). The Guilford Press.
Goldstein, B. L., Kotov, R., Perlman, G., Watson, D., & Klein, D. N. (2018). Trait and facet-level predictors of first-onset depressive and anxiety disorders in a community sample of adolescent girls. Psychological Medicine, 48(8), 1282–1290. https://doi.org/10.1017/S0033291717002719
Goldstein, B. L., Perlman, G., Eaton, N. R., Kotov, R., & Klein, D. N. (2020). Testing explanatory models of the interplay between depression, neuroticism, and stressful life events: A dynamic trait-stress generation approach. Psychological Medicine, 50(16), 2780–2789. https://doi.org/10.1017/S0033291719002927
Goodman, R., Ford, T., Simmons, H., Gatward, R., & Meltzer, H. (2000). Using the Strengths and Difficulties Questionnaire (SDQ) to screen for child psychiatric disorders in a community sample. The British Journa of Psychiatry, 177(6), 534–539. https://doi.org/10.1192/bjp.177.6.534
Hakulinen, C., Elovainio, M., Pulkki-Råback, L., Virtanen, M., Kivimäki, M., & Jokela, M. (2015). Personality and depressive symptoms: Individual participant meta-analysis of 10 cohort studies. Depression and Anxiety, 32(7), 461–470. https://doi.org/10.1002/da.22376
Halse, M., Steinsbekk, S., Hammar, Å., & Wichstrøm, L. (2022). Longitudinal relations between impaired executive function and symptoms of psychiatric disorders in childhood. Journal of Child Psychology and Psychiatry, 63(12), 1574–1582. https://doi.org/10.1111/jcpp.13622
Hamaker, E. L., Kuiper, R. M., & Grasman, R. P. (2015). A critique of the cross-lagged panel model. Psychological Methods, 20(1), 102–116. https://doi.org/10.1037/a0038889
Hamaker, E. L., Mulder, J. D., & van IJzendoorn, M. H. (2020). Description, prediction and causation: Methodological challenges of studying child and adolescent development. Developmental Cognitive Neuroscience, 46, 1–14. https://doi.org/10.1016/j.dcn.2020.100867
John, O. P., Naumann, L. P., & Soto, C. J. (2008). Paradigm shift to the integrative Big Five trait taxonomy: History, measurement, and conceptual issues. In O. P. John, R. W. Robins, & L. A. Pervin (Eds.), Handbook of personality: Theory and research (pp. 114–158). The Guilford Press.
Kaufman, J., Birmaher, B., Axelson, D., Perepletchikova, F., Brent, D., & Ryan, N. (2016). K-SADS-PL DSM-5. Western Psychiatric Institute and Clinic.
Kendler, K. S., Gardner, C. O., Neale, M. C., Aggen, S., Heath, A., Colodro-Conde, L., et al. (2019). Shared and specific genetic risk factors for lifetime major depression, depressive symptoms and neuroticism in three population-based twin samples. Psychological Medicine, 49(16), 2745–2753. https://doi.org/10.1017/S003329171800377X
Kercher, A. J., Rapee, R. M., & Schniering, C. A. (2009). Neuroticism, life events and negative thoughts in the development of depression in adolescent girls. Journal of Abnormal Child Psychology, 37, 903–915. https://doi.org/10.1007/s10802-009-9325-1
Klein, D. N., Kotov, R., & Bufferd, S. J. (2011). Personality and depression: Explanatory models and review of the evidence. Annual Review of Clinical Psychology, 7, 269–295. https://doi.org/10.1146/annurev-clinpsy-032210-104540
Klimstra, T. A., Akse, J., Hale, W. W., III., Raaijmakers, Q. A., & Meeus, W. H. (2010). Longitudinal associations between personality traits and problem behavior symptoms in adolescence. Journal of Research in Personality, 44(2), 273–284. https://doi.org/10.1016/j.jrp.2010.02.004
Krause, E. D., Vélez, C. E., Woo, R., Hoffmann, B., Freres, D. R., Abenavoli, R. M., et al. (2018). Rumination, depression, and gender in early adolescence: A longitudinal study of a bidirectional model. The Journal of Early Adolescence, 38(7), 923–946. https://doi.org/10.1177/027243161770495
Kwong, A. S. F., Morris, T. T., Pearson, R. M., Timpson, N. J., Rice, F., Stergiakouli, E., et al. (2021). Polygenic risk for depression, anxiety and neuroticism are associated with the severity and rate of change in depressive symptoms across adolescence. Journal of Child Psycholology and Psychiatry, 62(12), 1462–1474. https://doi.org/10.1111/jcpp.13422
Laceulle, O. M., Ormel, J., Vollebergh, W. A., Van Aken, M. A., & Nederhof, E. (2014). A test of the vulnerability model: Temperament and temperament change as predictors of future mental disorders–the TRAILS study. Journal of Child Psychology and Psychiatry, 55(3), 227–236. https://doi.org/10.1111/jcpp.12141
Lervåg, A. (2020). Some roads less travelled—different routes to understanding the causes of child psychopathology. Journal of Child Psychology and Psychiatry, 61(6), 625–627. https://doi.org/10.1111/jcpp.13362
Li, J., Yao, G., Liu, S., Li, X., Zhao, W., Du, X., et al. (2021). Mechanisms of the effects of parental emotional warmth on extraversion in children and adolescents. Neuroscience, 467, 134–141. https://doi.org/10.1016/j.neuroscience.2021.05.021
Little, R. J. (1988). A test of missing completely at random for multivariate data with missing values. Journal of the American Statistical Association, 83, (404), 1198–1202.
Liu, C., Chen, L., & Chen, S. (2020). Influence of neuroticism on depressive symptoms among Chinese adolescents: The mediation effects of cognitive emotion regulation strategies. Frontiers in Psychiatry, 11(420), 1–11. https://doi.org/10.3389/fpsyt.2020.00420
Lüdtke, O., & Robitzsch, A. (2021). A critique of the random intercept cross-lagged panel model. PsyArXiv Preprints. https://doi.org/10.31234/osf.io/6f85c
Masselink, M., Van Roekel, E., Hankin, B., Keijsers, L., Lodder, G., Vanhalst, J., et al. (2018). The longitudinal association between self–esteem and depressive symptoms in adolescents: Separating between–person effects from within–person effects. European Journal of Personality, 32(6), 653–671. https://doi.org/10.1002/per.2179
Merikangas, K. R., He, J.-P., Burstein, M., Swanson, S. A., Avenevoli, S., Cui, L., Benjet, C., Georgiades, K., & Swendsen, J. (2010). Lifetime prevalence of mental disorders in US adolescents: Results from the National Comorbidity Survey Replication-Adolescent Supplement (NCS-A). Journal of the American Academy of Child & Adolescent Psychiatry, 49(10), 980–989. https://doi.org/10.1016/j.jaac.2010.05.017
Morken, I. S., Viddal, K. R., Ranum, B., & Wichstrøm, L. (2020). Depression from preschool to adolescence—five faces of stability. Journal of Child Psychology and Psychiatry, 62(8), 1000–1009. https://doi.org/10.1111/jcpp.13362
Mund, M., & Nestler, S. (2019). Beyond the cross-lagged panel model: Next-generation statistical tools for analyzing interdependencies across the life course. Advances in Life Course Research, 41, 100249. https://doi.org/10.1016/j.alcr.2018.10.002
Ormel, J., Jeronimus, B. F., Kotov, R., Riese, H., Bos, E. H., Hankin, B., Rosmalen, J. G. M., & Oldehinkel, A. J. (2013). Neuroticism and common mental disorders: Meaning and utility of a complex relationship. Clinical Psychology Review, 33(5), 686–697. https://doi.org/10.1016/j.cpr.2013.04.003
Ormel, J., Oerlemans, A. M., Raven, D., Oldehinkel, A. J., & Laceulle, O. M. (2020). Mental disorder during adolescence: Evidence of arrested personality development. Clinical Psychological Science, 8(3), 395–411. https://doi.org/10.1177/2167702619896372
Richards, D. (2011). Prevalence and clinical course of depression: a review. Clinical Psychology Review, 31(7), 1117–1125. https://doi.org/10.1016/j.cpr.2011.07.004
Rudolph, K. D., & Flynn, M. (2014). Depression in adolescents. In I. H. Gotlb & C. Hammen, L (Eds.), Handbook of depression (3rd ed., pp. 391–409). The Guilford Press.
Rueger, S. Y., Malecki, C. K., Pyun, Y., Aycock, C., & Coyle, S. (2016). A meta-analytic review of the association between perceived social support and depression in childhood and adolescence. Psychological Bulletin, 142(10), 1017–1067. https://doi.org/10.1037/bul0000058
Salk, R. H., Hyde, J. S., & Abramson, L. Y. (2017). Gender differences in depression in representative national samples: meta-analyses of diagnoses and symptoms. Psychological Bulletin, 143(8), 783–822. https://doi.org/10.1037/bul0000102
Sandstrom, A., Perroud, N., Alda, M., Uher, R., & Pavlova, B. (2021). Prevalence of attention-deficit/hyperactivity disorder in people with mood disorders: a systematic review and meta-analysis. Acta Psychiatrica Scandinavica, 143(5), 380–391. https://doi.org/10.1111/acps.13283
Satorra, A., & Bentler, P. M. (2001). A scaled difference chi-square test statistic for moment structure analysis. Psychometrika, 66(4), 507–514. https://doi.org/10.1007/BF02296192
Segrin, C., & Dillard, J. P. (1992). The interactional theory of depression: A meta-analysis of the research literature. Journal of Social and Clinical Psychology, 11(1), 43–70. https://doi.org/10.1521/jscp.1992.11.1.43
Sharma, V., Coleman, S., Nixon, J., Sharples, L., Hamilton-Shield, J., Rutter, H., & Bryant, M. (2019). A systematic review and meta-analysis estimating the population prevalence of comorbidities in children and adolescents aged 5 to 18 years. Obesity Reviews, 20(10), 1341–1349. https://doi.org/10.1111/obr.12904
Slavish, D. C., Sliwinski, M. J., Smyth, J. M., Almeida, D. M., Lipton, R. B., Katz, M. J., et al. (2018). Neuroticism, rumination, negative affect, and sleep: Examining between-and within-person associations. Personality and Individual Differences, 123, 217–222. https://doi.org/10.1016/j.paid.2017.11.023
Soto, C. J., John, O. P., Gosling, S. D., & Potter, J. (2008). The developmental psychometrics of big five self-reports: Acquiescence, factor structure, coherence, and differentiation from ages 10 to 20. Journal of Personality and Social Psychology, 94(4), 718–737. https://doi.org/10.1037/0022-3514.94.4.718
Soto, C. J., John, O. P., Gosling, S. D., & Potter, J. (2011). Age differences in personality traits from 10 to 65: Big Five domains and facets in a large cross-sectional sample. Journal of Personality and Social Psychology, 100(2), 330–348. https://doi.org/10.1037/a0021717
Starr, L. R., & Davila, J. (2008). Excessive reassurance seeking, depression, and interpersonal rejection: A meta-analytic review. Journal of Abnormal Psychology, 117(4), 762–775. https://doi.org/10.1037/a0013866
Steinsbekk, S., & Wichstrøm, L. (2018). Cohort Profile: The Trondheim Early Secure Study (TESS)—a study of mental health, psychosocial development and health behaviour from preschool to adolescence. International Journal of Epidemiology, 47(5), 1401–1401i. https://doi.org/10.1093/ije/dyy190
Swickert, R. J., Rosentreter, C. J., Hittner, J. B., & Mushrush, J. E. (2002). Extraversion, social support processes, and stress. Personality and Individual Differences, 32(5), 877–891. https://doi.org/10.1016/S0191-8869(01)00093-9
Tackett, J. L. (2006). Evaluating models of the personality–psychopathology relationship in children and adolescents. Clinical Psychology Review, 26(5), 584–599. https://doi.org/10.1016/j.cpr.2006.04.003
Tian, L., Jiang, S., & Huebner, E. S. (2019). The big two personality traits and adolescents’ complete mental health: The mediation role of perceived school stress. School Psychology, 34(1), 32–42. https://doi.org/10.1037/spq0000257
Ullman, J. B., Tabachnick, B. G., & Fidell, L. S. (2001). Structural equation modeling. In B. G. Tabachnick & L. S. Fidell (Eds.), Using Multivariate Statistics (4th ed., pp. 653–771). Pearson Eduation.
Usami, S. (2023). Within-person variability score-based causal inference: A two-step estimation for joint effects of time-varying treatments. Psychometrika, 88(4), 1466–1494. https://doi.org/10.1007/s11336-022-09879-1
Van der Linden, D., te Nijenhuis, J., & Bakker, A. B. (2010). The general factor of personality: A meta-analysis of Big Five intercorrelations and a criterion-related validity study. Journal of Research in Personality, 44(3), 315–327. https://doi.org/10.1016/j.jrp.2010.03.003
Wichstrøm, L., Berg-Nielsen, T. S., Angold, A., Egger, H. L., Solheim, E., & Sveen, T. H. (2012). Prevalence of psychiatric disorders in preschoolers. Journal of Child Psychology and Psychiatry, 53(6), 695–705. https://doi.org/10.1111/j.1469-7610.2011.02514.x
Williams, A. L., Craske, M. G., Mineka, S., & Zinbarg, R. E. (2021). Neuroticism and the longitudinal trajectories of anxiety and depressive symptoms in older adolescents. Journal of Abnormal Psychology, 130(2), 126–140. https://doi.org/10.1037/abn0000638
World Health Organization, WHO. (2019). Adolescent mental health. Retrieved from https://www.who.int/news-room/fact-sheets/detail/adolescent-mental-health
Yang, H.-J., Chiu, Y.-J., Soong, W.-T., & Chen, W. J. (2008). The roles of personality traits and negative life events on the episodes of depressive symptoms in nonreferred adolescents: a 1-year follow-up study. Journal of Adolescent Health, 42(4), 378–385. https://doi.org/10.1016/j.jadohealth.2007.09.017
Yoon, K. L., Maltby, J., & Joormann, J. (2013). A pathway from neuroticism to depression: Examining the role of emotion regulation. Anxiety, Stress & Coping, 26(5), 558–572. https://doi.org/10.1080/10615806.2012.734810
Zhang, D., Huebner, E. S., & Tian, L. (2020). Longitudinal associations among neuroticism, depression, and cyberbullying in early adolescents. Computers in Human Behavior, 112(106475), 1–9. https://doi.org/10.1016/j.chb.2020.106475
Acknowledgements
We are grateful to the adolescents and families who diligently biennially participated in the Trondheim Early Secure Study (TESS).
Funding
Open access funding provided by NTNU Norwegian University of Science and Technology (incl St. Olavs Hospital - Trondheim University Hospital)
Author information
Authors and Affiliations
Contributions
All authors conceived the research questions and design. ISM performed the literature searches and drafted the first manuscript. LW, KRV and SS contributed to the development and writing of the manuscript. Statistical analyses were performed by LW, and statistical interpretation was performed by all authors. All authors approved the final draft. All authors had full access to all data in the study and final responsibility for the decision to submit for publication.
Corresponding author
Ethics declarations
Funding
The paper was funded by grant ES611813 from the Research Council of Norway, and a grant from the Liaison Committee for Education, Research and Innovation in Central Norway.
Competing Interests
We declare no competing interests. The funders of the study had no role in the study design, data collection, data analyses, data interpretation, or writing of the report.
Ethics Approval
Study procedures were approved by the Regional Committee for Medical and Health Research Ethics, Mid-Norway (approval number 2009/994).
Informed Consent
We have obtained written consent from the participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Morken, I.S., Wichstrøm, L., Steinsbekk, S. et al. Depression and Personality Traits Across Adolescence—Within-Person Analyses of a Birth Cohort. Res Child Adolesc Psychopathol (2024). https://doi.org/10.1007/s10802-024-01188-8
Accepted:
Published:
DOI: https://doi.org/10.1007/s10802-024-01188-8