Abstract
Purpose
Somatization is an important mental process that may causes medically unexplained and treatment-resistant somatic symptoms. The aim of the study is assess the presence of somatization in patients with dry eye disease (DED).
Methods
Eighty-eight patients with no objective DED finding and ongoing DED treatment were included in this prospective and observational study. Patients with subjective symptoms formed the symptom group and patients without subjective symptoms formed the control group. All patients were scored with the Turkish version of the Ocular Surface Disease Index (OSDI), Hamilton Depression Rating Scale (HAM-D), Hamilton Anxiety Rating Scale (HAM-A), Symptom Checklist-90-R (SCL-90R) somatization subscale, Toronto Alexithymia Scale (TAS), Pain Catastrophizing Scale (PCS), and Symptom Interpretation Questionnaire (SIQ).
Results
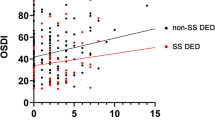
Mean OSDI score was significantly higher in the symptom group than in the control group. The mean HAM-D and HAM-A outcomes did not differ between the groups. The mean SCL-90R somatization subscale, TAS, and PCS scores were significantly higher in the symptom group than in the control group. In the SIQ, somatic attributional style score was significantly higher in the symptom group than in the control group. The SCL-90R somatization subscale, PCS, and somatic attributional style scores had positive and mild-moderate correlation with OSDI scores in the symptom group. The TAS score had positive and moderate correlation with OSDI scores in all sample analyses.
Conclusion
Somatization should be considered in patients with DED with chronic ocular surface symptoms. Presence of subjective symptoms resistant to treatment may be an indicator of somatization.
Similar content being viewed by others
References
Javadi MA, Feizi S (2011) Dry eye syndrome. J Ophthalmic Vis Res 6:192–198
Nelson JD, Helms H, Fiscella R et al (2000) A new look at dry eye disease and its treatment. Adv Ther 17:84–93
Miljanović B, Dana R, Sullivan DA et al (2007) Impact of dry eye syndrome on vision-related quality of life. Am J Ophthalmol 143(409–415):e402
Labbé A, Wang YX, Jie Y et al (2013) Dry eye disease, dry eye symptoms and depression: the Beijing eye study. Br J Ophthalmol 97:1399–1403
Li M, Gong L, Sun X et al (2011) Anxiety and depression in patients with dry eye syndrome. Curr Eye Res 36:1–7
Scamvougeras A, Howard A (2020) Somatic symptom disorder, medically unexplained symptoms, somatoform disorders, functional neurological disorder: how DSM-5 got it wrong. Can J Psychiatry 65(5):301–305. https://doi.org/10.1177/0706743720912858
Hiller W, Rief W, Brähler E (2006) Somatization in the population: from mild bodily misperceptions to disabling symptoms. Soc Psychiatry Psychiatr Epidemiol 41:704–712
Flasinski T, Dierolf AM, Rost S et al (2020) Altered interoceptive awareness in high habitual symptom reporters and patients with somatoform disorders. Front Psychol 11:1859
Zhao J, Su Q, Liu F et al (2020) Enhanced connectivity of thalamocortical networks in first-episode, treatment-naive somatization disorder. Front Psychiatry 11:555836
Barsky AJ, Orav EJ, Bates DW (2005) Somatization increases medical utilization and costs independent of psychiatric and medical comorbidity. Arch Gen Psychiatry 62:903–910
Irkec M, Group TOS (2007) Reliability and validity of Turkish translation of the ocular surface disease index (OSDI) in dry eye syndrome. Invest Ophthalmol Vis Sci 48:408–408
Craig JP, Nichols KK, Akpek EK et al (2017) TFOS DEWS II definition and classification report. Ocul Surf 15:276–283
Akdemir A, Türkçapar M, Örsel S et al (2001) Reliability and validity of the Turkish version of the Hamilton depression rating scale. Compr Psychiatry 42:161–165
Yazici MK, Demir B, Tanriverdi N et al (1998) Hamilton anxiety rating scale: interrater reliability and validity study. Turk Psikiyatri Derg 9:114–117
Kılıç M (1991) Belirti tarama listesi (SCL-90-R)’nin Geçerlilik ve Güvenirliği. Türk Psikolojik Danışma ve Rehberlik Dergisi 1:45–52
Gülec H, Kose S, Citak S et al (2009) The Turkish version of the 20-Item Toronto alexithymia scale (TAS-20): reliability, validity, and factorial structure. Klinik Psikofarmakol Bulteni 19:214–220
Ugurlu M, Karakas Ugurlu G, Erten S et al (2017) Validity of Turkish form of Pain Catastrophizing Scale and modeling of the relationship between pain-related disability with pain intensity, cognitive, and emotional factors. Psychiatr Clin Psychopharmacol 27:189–196
Duman O, Usubutun S, Goka E (2004) Belirti yorumlama ölçeğinin türkçe geçerlik ve güvenilirliği. Turk Psikiyatri Derg 15:26–40
Belmonte C, Nichols JJ, Cox SM et al (2017) TFOS DEWS II pain and sensation report. Ocul Surf 15:404–437
North C, Hong B, Lai H et al (2019) Assessing somatization in urologic chronic pelvic pain syndrome. BMC Urol 19:130
Zolnoun D, Park EM, Moore CG et al (2008) Somatization and psychological distress among women with vulvar vestibulitis syndrome. Int J Gynaecol Obstet 103:38–43
Fishbain DA, Lewis JE, Gao J et al (2009) Is chronic pain associated with somatization/hypochondriasis? An evidence- based structured review. Pain Pract 9:449–467
Rief W, Broadbent E (2007) Explaining medically unexplained symptoms-models and mechanisms. Clin Psychol Rev 27:821–841. https://doi.org/10.1016/j.cpr.2007.07.005
Fishbain DA, Cole B, Cutler RB et al (2006) Chronic pain and the measurement of personality: do states influence traits? Pain Med 7:509–529
Barsky AJ, Wyshak G (1990) Hypochondriasis and somatosensory amplification. Br J Psychiatry 157:404–409
DeGucht V, Heiser W (2003) Alexithymia and somatisation: quantitative review of the literature. J Psychosom Res 54(5):425–434. https://doi.org/10.1016/S0022-3999(02)00467-1
Di Tella M, Castelli L (2016) Alexithymia in chronic pain disorders. Curr Rheumatol Rep 18(7):41. https://doi.org/10.1007/s11926-016-0592-x
Tuzer V, Bulut SD, Bastug B et al (2011) Causal attributions and alexithymia in female patients with fibromyalgia or chronic low back pain. Nord J Psychiatry 65(2):138–144
Wan KH, Chen LJ, Young AL (2016) Depression and anxiety in dry eye disease: a systematic review and meta-analysis. Eye (Lond) 30(12):1558–1567
Funding
No funding was received to assist with the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Fuat Yavrum, Melike Ezerbolat Özateş and Serdar Özateş. The first draft of the manuscript was written by Fuat Yavrum and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
This prospective and observational study was conducted at the Okan University Faculty of Medicine, Istanbul, Turkey and Erenkoy Mental Health and Neurological Diseases Training and Research Hospital, Istanbul, Turkey in accordance with the ethical standards of the Declaration of Helsinki. The study protocol was approved by the institutional board of the Erenkoy Mental Health and Neurological Diseases Training and Research Hospital ethics committee.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent to publish
Additional informed consent was obtained from all individual participants for whom identifying information is included in this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yavrum, F., Ezerbolat Ozates, M. & Ozates, S. An important contributing factor in dry eye disease: somatization. Int Ophthalmol 44, 190 (2024). https://doi.org/10.1007/s10792-024-03133-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10792-024-03133-6