Abstract
Purpose
This study was conducted to compare the ocular surface temperature in keratoconus eyes with that in normal eyes.
Methods
A total of 27 participants were enrolled, with 10 and 17 participants in the keratoconus and control groups, respectively. Participants in the control group underwent an ophthalmic slit lamp examination and ocular thermography, while an additional corneal tomography was performed for those in the keratoconus group.
Results
For patients with keratoconus, the mean upper eyelid temperature (UET) was 32.36 ± 1.02 °C, inner canthus temperature (ICT) was 34.25 ± 0.83 °C, outer canthus temperature (OCT) was 33.62 ± 0.96 °C, initial central corneal temperature (initial CCT) was 33.04 ± 1.03 °C, sixth-second CCT (6 s-CCT) was 32.67 ± 1.19 °C, and the mean change in CCT measured within 6 s (change in CCT within 6 s) was 0.36 ± 0.26 °C. For controls, the values for UET, ICT, OCT, initial CCT, 6 s-CCT, and change in CCT within 6 s were 32.35 ± 1.13 °C, 34.14 ± 0.91 °C, 33.51 ± 1.02 °C, 33.22 ± 1.01 °C, 32.99 ± 1.01 °C, and 0.22 ± 0.17 °C, respectively. Except for the change in CCT within 6 s (p = 0.022), no significant differences were observed in UET (p = 0.973), ICT (p = 0.659), OCT (p = 0.697), initial CCT (p = 0.556) or 6 s-CCT (p = 0.310) between the two groups.
Conclusion
The keratoconus eyes showed faster changes in CCT and evaporation of tear film after opening the eyes. Therefore, the keratoconus eyes had a higher incidence of dry eye conditions.





Similar content being viewed by others
Abbreviations
- ROIs:
-
Regions of interest
- CCT:
-
Central corneal temperature
- FT:
-
Forehead temperature
- UET:
-
Upper eyelid temperature
- ICT:
-
Inner canthus temperature
- OCT:
-
Outer canthus temperature
- InitialCCT:
-
Initial central corneal temperature
- 6 s-CCT:
-
Sixth-second central corneal temperature
- Change in CCT within 6 s:
-
Change in central corneal temperature measured within 6 s
- BCVA:
-
Best corrected visual acuity
- Kf:
-
Corneal curvature flat
- Ks:
-
Corneal curvature steep
- Rf:
-
Corneal curvature radius flat
- Rs:
-
Corneal curvature radius steep
References
Morgan PB, Smyth JV, Tullo AB, Efron N (1999) Ocular temperature in carotid artery stenosis. Optom Vis Sci 76:850–854. https://doi.org/10.1097/00006324-199912000-00021
García-Porta N, Gantes-Nuñez FJ, Tabernero J, Pardhan S (2019) Characterization of the ocular surface temperature dynamics in glaucoma subjects using long-wave infrared thermal imaging: publisher’s note. J Opt Soc Am A 36:1584. https://doi.org/10.1364/JOSAA.36.001584
Hannerz J (1985) Pain characteristics of painful ophthalmoplegia (The Tolosa-Hunt syndrome). Cephalalgia 5:103–106. https://doi.org/10.1046/j.1468-2982.1985.0502103.x
Tan J-H, Ng EYK, Rajendra Acharya U, Chee C (2009) Infrared thermography on ocular surface temperature: a review. Infrared Phys Technol 52:97–108. https://doi.org/10.1016/j.infrared.2009.05.002
Su T-Y, Chang S-W (2021) Normalized ocular surface temperature models for tear film characteristics and dry eye disease evaluation. Ocul Surf 19:74–82. https://doi.org/10.1016/j.jtos.2020.04.002
Dursch TJ, Li W, Taraz B et al (2018) Tear-film evaporation rate from simultaneous ocular-surface temperature and tear-breakup area. Optom Vis Sci 95:5–12. https://doi.org/10.1097/OPX.0000000000001156
Su T-Y, Chang S-W, Yang C-J, Chiang HK (2014) Direct observation and validation of fluorescein tear film break-up patterns by using a dual thermal-fluorescent imaging system. Biomed Opt Express 5:2614. https://doi.org/10.1364/BOE.5.002614
Abreau K, Callan C, Kottaiyan R et al (2016) Temperatures of the ocular surface, lid, and periorbital regions of Sjögren’s, evaporative, and aqueous-deficient dry eyes relative to normals. Ocul Surf 14:64–73. https://doi.org/10.1016/j.jtos.2015.09.001
Matteoli S, Favuzza E, Mazzantini L et al (2017) Ocular surface temperature in patients with evaporative and aqueous-deficient dry eyes: a thermographic approach. Physiol Meas 38:1503–1512. https://doi.org/10.1088/1361-6579/aa78bd
Zhang Q, Wu Y, Song Y et al (2021) Screening evaporative dry eyes severity using an infrared image. J Ophthalmol 2021:1–8. https://doi.org/10.1155/2021/8396503
Romero-Jiménez M, Santodomingo-Rubido J, Wolffsohn JS (2010) Keratoconus: a review. Cont Lens Anter Eye 33:157–166. https://doi.org/10.1016/j.clae.2010.04.006
Zadnik K, Barr JT, Gordon MO, Edrington TB (1996) Biomicroscopic signs and disease severity in keratoconus. Cornea 15:139–146. https://doi.org/10.1097/00003226-199603000-00006
Kennedy RH, Bourne WM, Dyer JA (1986) A 48-year clinical and epidemiologic study of keratoconus. Am J Ophthalmol 101:267–273. https://doi.org/10.1016/0002-9394(86)90817-2
Zadnik K, Steger-May K, Fink BA et al (2002) Between-eye asymmetry in keratoconus. Cornea 21:671–679. https://doi.org/10.1097/00003226-200210000-00008
Chopra I, Jain AK (2005) Between eye asymmetry in keratoconus in an Indian population. Clin Exp Optom 88:146–152. https://doi.org/10.1111/j.1444-0938.2005.tb06687.x
Rabinowitz YS (1998) Keratoconus. Surv Ophthalmol 42:297–319. https://doi.org/10.1016/S0039-6257(97)00119-7
Chang H-YP, Chodosh J (2013) The genetics of keratoconus. Semin Ophthalmol 28:275–280. https://doi.org/10.3109/08820538.2013.825295
Lema I, Sobrino T, Duran JA et al (2009) Subclinical keratoconus and inflammatory molecules from tears. Br J Ophthalmol 93:820–824. https://doi.org/10.1136/bjo.2008.144253
Stachon T, Latta L, Kolev K et al (2021) Erhöhte NF-κB-und iNOS-expression in Keratozyten von Keratokonuspatienten–Hinweise auf eine entzündliche Komponente? Klin Monbl Augenheilkd 238:1010–1017. https://doi.org/10.1055/a-1002-0100
Klamann MKJ, Maier A-KB, Gonnermann J et al (2013) Ocular surface temperature gradient is increased in eyes with bacterial corneal ulcers. Ophthalmic Res 49:52–56. https://doi.org/10.1159/000343774
Kawali AA (2013) Thermography in ocular inflammation. Indian J Radiol Imaging 23:281–283. https://doi.org/10.1055/s-0041-1734381
Hara Y, Shiraishi A, Yamaguchi M et al (2014) Evaluation of allergic conjunctivitis by thermography. Ophthalmic Res 51:161–166. https://doi.org/10.1159/000357105
Giannaccare G, Fresina M, Agnifili L, Versura P (2016) Ocular-surface temperature modification by cataract surgery. J Cataract Refract Surg 42:983–989. https://doi.org/10.1016/j.jcrs.2016.04.023
Kolozsvári BL, Petrovski G, Gogolák P et al (2014) Association between mediators in the tear fluid and the severity of keratoconus. Ophthalmic Res 51:46–51. https://doi.org/10.1159/000351626
Dogru M, Karakaya H, Özçetin H et al (2003) Tear function and ocular surface changes in keratoconus. Ophthalmology 110:1110–1118. https://doi.org/10.1016/S0161-6420(03)00261-6
Li X (2004) Longitudinal study of the normal eyes in unilateral keratoconus patients. Ophthalmology 111:440–446. https://doi.org/10.1016/j.ophtha.2003.06.020
Owens H, Gamble G (2003) A profile of keratoconus in New Zealand. Cornea 22:122–125. https://doi.org/10.1097/00003226-200303000-00008
Weed KH, McGhee CNJ (1998) Referral patterns, treatment management and visual outcome in keratoconus. Eye 12:663–668. https://doi.org/10.1038/eye.1998.165
Wagner H, Barr JT, Zadnik K (2007) Collaborative longitudinal evaluation of keratoconus (CLEK) study: methods and findings to date. Cont Lens Anter Eye 30:223–232. https://doi.org/10.1016/j.clae.2007.03.001
Németh O, Langenbucher A, Eppig T et al (2021) Correlation between corneal endothelial cell density and central ocular surface temperature in normal and keratoconus eyes. Curr Eye Res 46:445–451. https://doi.org/10.1080/02713683.2020.1812087
Dienes L, Kiss HJ, Perényi K et al (2015) Corneal sensitivity and dry eye symptoms in patients with keratoconus. PLoS One 10:e0141621. https://doi.org/10.1371/journal.pone.0141621
Németh O, Langenbucher A, Eppig T et al (2020) Ocular surface disease index and ocular thermography in keratoconus patients. J Ophthalmol 2020:1–8. https://doi.org/10.1155/2020/1571283
Zemova E, Eppig T, Seitz B et al (2014) Interaction between topographic/tomographic parameters and dry eye disease in keratoconus patients. Curr Eye Res 39:1–8. https://doi.org/10.3109/02713683.2013.798667
Jie Y, Xu L, Wu YY, Jonas JB (2009) Prevalence of dry eye among adult Chinese in the Beijing eye study. Eye 23:688–693. https://doi.org/10.1038/sj.eye.6703101
Stapleton F, Alves M, Bunya VY et al (2017) TFOS DEWS II epidemiology report. Ocul Surf 15:334–365. https://doi.org/10.1016/j.jtos.2017.05.003
Moshirfar M, West WB, Marx DP (2020) Face mask-associated ocular irritation and dryness. Ophthalmol Ther 9:397–400. https://doi.org/10.1007/s40123-020-00282-6
Boccardo L (2022) Self-reported symptoms of mask-associated dry eye: a survey study of 3605 people. Contact Lens Anter Eye 45:101408. https://doi.org/10.1016/j.clae.2021.01.003
Hadayer A, Zahavi A, Livny E et al (2020) Patients wearing face masks during intravitreal injections may be at a higher risk of endophthalmitis. Retina 40:1651–1656. https://doi.org/10.1097/IAE.0000000000002919
Acknowledgements
Thanks to the technical support of teachers from the School of Optical Electrical and Computer Engineering, University of Shanghai for Science and Technology. Also thanks to the patients/volunteers for their kind consent and cooperation during the study.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
Dr. Gu Zhensheng wrote the main manuscript text and prepared figures and tables. Dr. Wu Chunbo collected the data and prepared the data base. All authors contributed to the study conception and design. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Xin Hua Hospital affiliated with Shanghai Jiao Tong University School of Medicine (March 17, 2023/ No. XHEC-D-2023–047).
Consent to participate
Informed consent was obtained from all individual participants (> 16 years) included in the study; Written informed consent was obtained from the parents of participants (< = 16 years).
Consent to publish
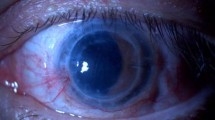
The authors affirm that human research participants provided informed consent for the publication of the images in Figure(s) 1a, 1b, and 1c.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gu, Z., Cao, G., Wu, C. et al. Comparing the ocular surface temperature and dry eye condition of keratoconus with normal eyes using infrared thermal imaging. Int Ophthalmol 43, 4781–4789 (2023). https://doi.org/10.1007/s10792-023-02878-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-023-02878-w