Abstract
Purpose
To determine the trends in the microbial spectrum and antibacterial susceptibility patterns of non-viral conjunctivitis over 16 years.
Methods
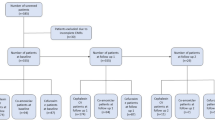
Microbiology data were reviewed from 2006–2021 for all the patients with clinically and culture-proven infectious conjunctivitis. Conjunctival swabs and/or conjunctival scrapings were collected for microbiological workup, and the demographic and antibiotic susceptibility data were extracted from the EMR (Electronic Medical Record). For statistical analysis, χ2-test was performed.
Results
Of the 1711 patients, 814 (47.57%) were culture positive and 897 (52.43%) were culture negative. Of the total culture-proven conjunctivitis cases, 775/814 (95.20%) were bacteria, and 39/814 (4.80%) were fungi. Among these bacterial isolates, 75.74% were gram-positive bacteria, while 24.26% were gram negative. The predominant gram-positive pathogens isolated were S. epidermidis (16.7%), S. aureus (17.9%) (p < 0.05), and S. pneumoniae (18.2%), while Haemophilus spp. (36.2%) (p < 0.05) was the most often isolated gram-negative bacteria (36.2%), and Aspergillus spp. was the most commonly isolated fungus (50%). The susceptibility of gram-positive bacteria to cefazoline increased from 90.46 to 98% (p = 0.01), whereas the susceptibility for gatifloxacin decreased in both gram-positive (81–41%; p < 0.0001) and gram-negative bacteria (73–58%; p = 0.02).
Conclusions
Increasing resistance of ocular isolates to mainstay antibiotics is a concern, and this data can assist healthcare practitioners in making informed choices regarding the treatment of ocular infections with ophthalmic antibiotics.





Similar content being viewed by others
References
Hosny AES, El-Bazza ZE, Ramadan MA et al (2021) Expression levels of pro-inflammatory interleukin-8 and certain antimicrobial peptides in concurrent with bacterial conjunctivitis. Int J Ophthalmol 14:666–675. https://doi.org/10.18240/ijo.2021.05.05
Høvding G (2008) Acute bacterial conjunctivitis. Acta Ophthalmol 86:5–17. https://doi.org/10.1111/j.1600-0420.2007.01006.x
Mohamed YH, Uematsu M, Morinaga Y et al (2021) Conjunctival sac microbiome in infectious conjunctivitis. Microorganisms 9:2095. https://doi.org/10.3390/microorganisms9102095
Adebayo A, Parikh JG, McCormick SA et al (2011) Shifting trends in in vitro antibiotic susceptibilities for common bacterial conjunctival isolates in the last decade at the New York Eye and Ear Infirmary. Graefes Arch Clin Exp Ophthalmol 249:111–119. https://doi.org/10.1007/s00417-010-1426-6
Azari AA, Barney NP (2013) Conjunctivitis: a systematic review of diagnosis and treatment. JAMA 310:1721–1730. https://doi.org/10.1001/jama.2013.280318
Sthapit PR, Tuladhar NR, Marasini S et al (2011) Bacterial conjunctivitis and use of antibiotics in Dhulikhel Hospital-Kathmandu University Hospital. Kathmandu Univ Med J 9:69–72. https://doi.org/10.3126/kumj.v9i2.6292
Shrestha SP, Khadka J, Pokhrel AK et al (2016) Acute bacterial conjunctivitis–antibiotic susceptibility and resistance to commercially available topical antibiotics in Nepal. Nepal J Ophthalmol 8:23–35. https://doi.org/10.3126/nepjoph.v8i1.16153
Alfonso SA, Fawley JD, Lu XA (2015) Conjunctivitis. Prim Care: Clin Office Pract 42(3):325–345. https://doi.org/10.1016/j.pop.2015.05.001
Haq A, Wardak H, Kraskian N (2013) Infective conjunctivitis–its pathogenesis, management and complications. Common Eye Infect. https://doi.org/10.5772/52462
Biswas P, Batra S, Gurha N et al (2022) Emerging antimicrobial resistance and need for antimicrobial stewardship for ocular infections in India: a narrative review. Indian J Ophthalmol 70(5):1513. https://doi.org/10.4103/ijo.IJO_2537_21
Kunimoto DY, Das T, Sharma S et al (1999) Microbiologic spectrum and susceptibility of isolates. Part I postoperative endophthalmitis. Am J Ophthalmol 128:240–242. https://doi.org/10.1016/s0002-9394(99)00112-9
Kunimoto DY, Das T, Sharma S et al (1999) Microbiologic spectrum and susceptibility of isolates. Part II posttraumatic endophthalmitis. Am J Ophthalmol 128:242–244. https://doi.org/10.1016/s0002-9394(99)00113-0
Sharma S, Kunimoto DY, Garg P et al (1999) Trends in antibiotic resistance of corneal pathogens: Part I. An analysis of commonly used ocular antibiotics. Indian J Ophthalmol 47:95–100
Sharma S, Jalali S, Adiraju MV et al (1996) Sensitivity and predictability of vitreous cytology, biopsy, and membrane filter culture in endophthalmitis. Retina (Philadelphia, Pa.) 16(6):525–529. https://doi.org/10.1097/00006982-199616060-00010
Kaliamurthy J, Kalavathy CM, Parmar P, Thomas PA et al (2013) Spectrum of bacterial keratitis at a tertiary eye care centre in India. BioMed Res Int. https://doi.org/10.1155/2013/181564
Wolfensberger A, Sax H, Weber R, Zbinden R, Kuster SP, Hombach M. Change of antibiotic susceptibility testing guidelines from CLSI to EUCAST: influence on cumulative hospital antibiograms. PloS one. 2013 Nov 1;8(11):e79130.
Tarabishy AB, Jeng BH (2008) Bacterial conjunctivitis—a review for internists. Clevel Clin J Med 75:507. https://doi.org/10.3949/ccjm.75.7.507
Gigliotti F, Williams WT, Hayden FG et al (1981) Etiology of acute conjunctivitis in children. J Pediatr 98:531–536. https://doi.org/10.1016/s0022-3476(81)80754-8
Schmitz H, Wigand R, Heinrich W (1983) Worldwide epidemiology of human adenovirus infections. Am J Epidemiol 117(4):455–466. https://doi.org/10.1093/oxfordjournals.aje.a113563
Fitch CP, Rapoza PA, Owens S et al (1989) Epidemiology and diagnosis of acute conjunctivitis at an inner-city hospital. Ophthalmology 96:1215–1220. https://doi.org/10.1016/s0161-6420(89)32749-7
Block SL, Hedrick J, Tyler R et al (2000) Increasing bacterial resistance in pediatric acute conjunctivitis (1997–1998). Antimicrob Agents Chemother 44:1650–1654. https://doi.org/10.1128/AAC.44.6.1650-1654.2000
Aoki K, Tagawa Y (2002) A twenty–one year surveillance of adenoviral conjunctivitis in Sapporo, Japan. Int Ophthalmol Clin 42:49–54. https://doi.org/10.1097/00004397-200201000-00008
Valentino MD, McGuire AM, Rosch JW et al (2014) Unencapsulated Streptococcus pneumoniae from conjunctivitis encode variant traits and belong to a distinct phylogenetic cluster. Nat Commun 12(5):5411. https://doi.org/10.1038/ncomms6411
Mokbul MI, Islam AK, Tabassum MN et al (2022) Recent incidence of infectious conjunctivitis in Bangladesh: are we aware? Ann Med Surg 84:104819. https://doi.org/10.1016/j.amsu.2022.104819
Hosny AE, El-Bazza ZE, Ramadan MA et al (2021) Expression levels of pro-inflammatory interleukin-8 and certain antimicrobial peptides in concurrent with bacterial conjunctivitis. Int J Ophthalmol 14(5):666. https://doi.org/10.18240/ijo.2021.05.05
National Health Portal India, Ministry of Health and Family Welfare (MoHFW), Government of India, Blepharitis2016. Available from: https://ncdc.mohfw.gov.in
Nuhu A, Usman A (2021) Bacterial conjunctivitis among patients of different age groups attending some eye clinics in Sokoto, Nigeria. Hmlyn Jr Appl Med Scie Res 2(5):161–165. https://doi.org/10.47310/hjamsr.2021.v02i05.030
Joseph J, Karoliya R, Sheba E et al (2022) Trends in the microbiological spectrum of nonviral keratitis at a single tertiary care ophthalmic hospital in India—a review of 30 years. Cornea 13:10–97. https://doi.org/10.1097/ICO.0000000000003105
Chatterjee S, Agrawal D, Gomase SN et al (2022) Fluoroquinolone resistance in bacterial isolates from ocular infections: trend in antibiotic susceptibility patterns between 2005–2020. Indian J Ophthalmol 70(12):4391–4398. https://doi.org/10.4103/ijo.IJO_1033_22
Lalitha P, Manoharan G, Karpagam R et al (2017) Trends in antibiotic resistance in bacterial keratitis isolates from South India. Br J Ophthalmol 101(2):108–113. https://doi.org/10.1136/bjophthalmol-2016-308487
Funding
Hyderabad Eye Research Foundation, Hyderabad, India.
Author information
Authors and Affiliations
Contributions
JJ shared in the conception and the design of the study. SM and JG were conducted in the data collection and statistical analysis. All authors shared in the interpretation of the data and in drafting the manuscript. All authors reviewed the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article. All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Ethical approval
The institutional ethics committee approved this study, and the procedures followed the Declaration of Helsinki’s precepts. All study participants signed a consent form.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Maiti, S., Gandhi, J. & Joseph, J. Microbiological spectrum and antibiotic susceptibility patterns of non-viral conjunctivitis over 16 years at a tertiary eye care center in Southern India. Int Ophthalmol 43, 3717–3724 (2023). https://doi.org/10.1007/s10792-023-02781-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-023-02781-4