Abstract
Purpose
The pathology of branch retinal vein occlusion (BRVO), a retinal circulatory disease, is related to monocular metamorphopsia-related vision impairment of the affected eyes, but the association of binocular metamorphopsia in such patients is unclear. This study aimed to examine the frequency of binocular metamorphopsia and its association with the clinical characteristics of patients with BRVO.
Methods
A total of 87 patients who were treated for BRVO-associated macular edema (ME) were included in this study. At baseline and 1 and 3 months after the initiation of anti-vascular endothelial growth factor (VEGF) treatment, we quantified metamorphopsia in the affected eyes and binocular metamorphopsia using the M-CHARTS® diagnostic tool.
Results
At baseline, 53 and 7 patients had metamorphopsia in the affected eyes and binocular metamorphopsia, respectively. Although the visual acuity improved significantly after the initiation of anti-VEGF treatment, the mean M-CHARTS score in the affected eyes did not change from the baseline score. At 3 months, 9 patients showed binocular metamorphopsia; it was significantly associated with metamorphopsia in the affected eyes with a 95% confidence interval of 0.021–0.122 (β = 0.306, p = 0.006).
Conclusion
Metamorphopsia in the affected eyes can cause binocular metamorphopsia in patients with BRVO-ME.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Branch retinal vein occlusion (BRVO) is the second most common retinal circulatory disease, and causes the retinal edema, hemorrhage, and/or ischemia in the affected area [1, 2]; involvement of the macular area in these pathological indications results in significant vision impairments [3,4,5]. Anti-vascular endothelial growth factor (VEGF) therapy can be used to treat most macular edemas (MEs) [6,7,8,9,10], and this has led to substantial improvements in the clinical management of decreased visual acuity (VA) [11,12,13].
Previous studies have shown that approximately 90% of patients with BRVO-ME suffer from monocular metamorphopsia-related vision impairment of the affected eyes [14]. Furthermore, it has also been elucidated that monocular metamorphopsia after BRVO-ME could negatively affect vision-related quality of life [15,16,17]. In clinical practice, occasional cases of patients with BRVO who complained of visual disability were observed, and this possibly could be related to metamorphopsia of the affected eyes [18, 19].
To better evaluate the association between the vision impairments and visual disability in patients with BRVO, a routine examination only for the affected eye may not be sufficient [20,21,22] and requires additional assessment (in addition to monocular metamorphopsia) of binocular metamorphopsia. However, the occurrence of binocular metamorphopsia in patients with BRVO is not fully investigated yet. This study aimed to examine the mono- and binocular metamorphopsia and associated clinical factors in patients with unilateral BRVO-ME.
Methods
This study adhered to the tenets of the Declaration of Helsinki and was approved by the Ethics Committees of the Kagawa University Faculty of Medicine (Kagawa, Japan), Kyoto University Graduate School of Medicine (Kyoto, Japan), Tokushima University Faculty of Medicine (Tokushima, Japan), and Saneikai Tsukazaki Hospital (Hyogo, Japan). Written informed consent was obtained from each patient before any study procedure or examination.
Patients
A total of 87 patients with unilateral and treatment-naïve BRVO who were examined and treated at Kagawa, Kyoto, Tokushima University, and Tsukazaki Hospital from April 2018 to March 2019 were included in this study. The inclusion criteria were as follows: (1) symptomatic BRVO with retinal hemorrhage and edema involving the macula, (2) foveal thickness (FT) greater than 250 µm at baseline (as measured by optical coherence tomography [OCT]), and (3) symptom duration of less than 3 months prior to the initial examination. BRVO was diagnosed based on fundus examinations, OCT angiography (PLEX Elite 9000; ZEISS, Germany), and/or fluorescein angiography (FA) findings. We excluded eyes with central retinal vein occlusion (CRVO) or hemi-CRVO and co-morbid ocular diseases that could affect the macula (e.g., epiretinal membrane, macular hole, diabetic retinopathy, retinal arterial macroaneurysm, glaucoma, central serous chorioretinopathy, age-related macular degeneration, and retinitis pigmentosa). We also excluded eyes with dense cataracts that could compromise OCT or OCT angiography image qualities and previously received any ocular interventions other than the cataract surgery. We did not exclude patients with BRVO because of poor VA of the affected eye. However, cases with Snellen VA of less than 20/40 in the fellow eye were excluded.
Study examinations and treatments
At baseline, medical history was obtained from each patient. All patients underwent a comprehensive ophthalmologic examination, including measurement of best-corrected VA (BCVA) using the Landolt chart, indirect ophthalmoscopy, slit-lamp biomicroscopy with a non-contact lens, and OCT imaging (Spectralis HRA + OCT; Heidelberg Engineering, Heidelberg, Germany; RS-3000, Nidek, Gamagori, Japan; 3D OCT-1, Topcon, Tokyo, Japan). We created a thickness map of the entire retina using the volumetric OCT scanning of the macula. Within the central subfield of the Early Treatment Diabetic Retinopathy Study grid, FT was defined as the mean distance between the vitreoretinal interface and retinal pigment epithelium.
In addition to OCT angiography, we performed FA (Optos 200Tx Imaging System, Optos PLC, Dunfermline, UK) to assess the retinal circulatory status. However, FA was not performed in patients who showed allergic reactions to the dye and those who did not provide consent for the FA examination.
All patients were treated for ME with intravitreal anti-VEGF injections of ranibizumab (0.5 mg Lucentis; Novartis Pharma, Tokyo, Japan) or aflibercept (0.5 mg Eylea; Bayer Pharma, Tokyo, Japan). After the initial treatment, each eye was examined every month, and further injections were administered on an as-needed basis when ME or serous retinal detachment was evident at the fovea on the OCT images.
Follow-up examinations were performed at one (month 1) and three months (month 3) after the initiation of anti-VEGF treatment. At each follow-up, the BCVA was measured, and retinal morphology was examined using the OCT.
Evaluation of metamorphopsia
At baseline, month 1, and month 3, we quantified metamorphopsia in the affected eyes and binocular metamorphopsia using the M-CHARTS® (Inami, Tokyo, Japan). An M-CHARTS® score of 0 indicates the absence of metamorphopsia. An M-CHARTS score of 0.3–0.5 or higher has been reported as the threshold for detecting metamorphopsia in daily life [23].
The M-CHARTS included 19 dotted lines. Each dot size was 0.1°, and the dot intervals ranged from 0.2 to 2.0° of the visual angle. A fixation point of 0.3° was placed at the center of each line. The examination was performed at a distance of 30 cm (with refraction correction) using charts with dotted lines (fine to coarse incremental spacing) that were shown to the patients one after another. When the patient recognized the presented line as straight, the visual angle to that line was considered as the degree of metamorphopsia. M-CHARTS were presented to the patient in vertical direction, followed by horizontal, vertical and horizontal scores were measured, and the average score of both directions was considered as the M-CHARTS score for the eye. In each patient, we evaluated metamorphopsia in the affected eye relative to the contralateral eye, and the binocular metamorphopsia was quantified using the M-CHARTS. Since the examinations were performed for the affected eye and the fellow eye, the sides of the affected eyes were disclosed by the examiners; however, the presence or absence of ME after the treatment and the treatment history were masked. The examiner was masked regarding the treatment history and recurrence of macular edema.
Statistical analysis
The data are presented as the mean ± standard deviation, where applicable. The BCVA was converted to the mean logarithm of the minimum angle of resolution (logMAR) for statistical analyses. Time-point and group comparisons were performed using the paired and unpaired t-tests, respectively. Multivariate linear regression analysis was performed to evaluate the contribution of each initially identifiable factor to binocular metamorphopsia at baseline. Statistical analyses were performed using the SPSS statistical software (version 26.0.0, IBM Japan, Tokyo, Japan), and statistical significance was defined as p < 0.05.
Results
Baseline
At baseline, all eyes with unilateral BRVO showed the ME-associated visual disturbances. The logMAR VA and FT were 0.48 ± 0.38 (range in Snellen VA was 20/1000–20/13) and 550.4 ± 218.0 µm, respectively (Table 1). Of the 87 patients, 53 (60.9%; mean M-CHARTS score 0.29 ± 0.37) and 7 (8.0%; M-CHARTS score 0.02 ± 0.09) patients showed metamorphopsia in the affected eyes and binocular metamorphopsia, respectively.
Changes in VA, FT, and metamorphopsia from baseline to month 3
After the initiation of anti-VEGF treatment, the logMAR VA improved significantly relative to the baseline value (p < 0.001 at both months 1 and 3, relative to baseline) (Table 1, Fig. 1); however, the mean M-CHARTS scores in the affected eyes showed no improvements (0.33 ± 0.37 (p = 0.322) and 0.36 ± 0.44 (p = 0.140) at months 1 and 3, respectively) (Fig. 1). During the observation period, binocular metamorphopsia was resolved in 4 patients but developed in 6 other patients. At the end of the follow-ups (month 3), 9 (10.3%) patients had binocular metamorphopsia. The mean binocular metamorphopsia M-CHARTS scores were 0.04 ± 0.13 and 0.03 ± 0.10 at months 1 and 3, respectively, with no improvements relative to the baseline score (p = 0.164 and p = 0.622 for months 1 and 3, respectively) (Fig. 1).
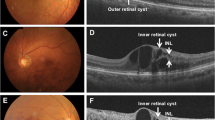
Changes in visual acuity, foveal thickness, and M-CHARTS® scores for the affected and both eyes from baseline to month 3 after initiating anti-vascular endothelial growth factor treatments for branch retinal vein occlusion-associated macular edemaChanges in a visual acuity, b foveal thickness, c M-CHARTS score for the affected eyes, and d M-CHARTS score for both eyes
Factors associated with metamorphopsia for binocular vision
Table 2 shows the results of the multivariate linear regression analysis on the association of the binocular metamorphopsia and other factors at baseline. The M-CHARTS score representing binocular metamorphopsia was significantly associated with the metamorphopsia in the affected eye (95% confidence interval of 0.021–0.122 [β = 0.306, p = 0.006]).
Discussion
This study showed that in patients with BRVO-ME, a high degree of the (monocular) metamorphopsia in the affected eye may lead to binocular metamorphopsia. The retinal area affected by BRVO is commonly asymmetrical in the vertical direction. Retinal edema also includes or excludes the fovea depending on the vertically asymmetric affected-retinal area. In this study, we therefore performed the M-CHARTS test in the vertical and horizontal directions and used the average value as the patient’s score. The M-CHARTS gradually changes from narrowly spaced dotted lines to widely spaced dotted lines and looks for the point at which the patient no longer perceives metamorphopsia. The process is very simple, and there appears to be no learning curve in the implementation of M-CHARTS.
M-CHARTS scores have been used to quantitatively examine the metamorphopsia in various retinal diseases. Previous examinations using M-CHARTS showed that a significant percentage of patients with BRVO-ME complain of metamorphopsia in the affected eyes [14], which was reportedly associated with presence of cystoid spaces in the inner retina and/or whole retinal thickness at the fovea [14, 15]. However, a direct mechanism responsible for the emergence of metamorphopsia remains obscure mainly due to presence of various pathologies (other than the retinal exudative changes) at the macula of eyes. In eyes with BRVO, retinal ischemic changes and/or foveal photoreceptor damage might lead to (monocular) metamorphopsia [18, 24,25,26]. VA significantly improved after 3 months (p < 0.001, Table 1); however, the rate of the metamorphopsia of the affected eye significantly increased from baseline to month 3. In six patients who had no binocular metamorphopsia at baseline, binocular metamorphopsia developed at 3 months. The rate of binocular metamorphopsia significantly increased from baseline to 3 months (p = 0.022, data not shown). Metamorphopsia might occur when cellular alignments in the neuronal and glial cells become irregular, and the pathologic changes are persistent to some degree [14]. Recovery of the resolution of ME might be sufficient for the improvement of VA; however, it might be insufficient for the improvement of metamorphopsia. Insufficient recovery of metamorphopsia might involve persistent and irregular alignments of the neuroglial cells. In this study, the degree of metamorphopsia for the affected eye at month 3 was significantly and positively associated with the defect length of the foveal ellipsoid zone band at baseline (p = 0.022, data not shown); however, it was not associated with FT.
Previous investigations showed that, in human vision, binocular summation and inhibition occur when the monocular acuities of the two eyes are nearly equivalent and discrepant, respectively [27,28,29]. Hence, binocular summation and/or inhibition might have contributed differently to the binocular vision of patients included in this study because the VA improved significantly during the observation period. Although details of the visual compensation in this study were unknown, the rate of occurrence of the binocular metamorphopsia was approximately one-sixth to that of the metamorphopsia in the affected eyes, and the M-CHARTS score representing the binocular metamorphopsia was significantly lower than that of the monocular metamorphopsia in the affected eyes (p < 0.001, Online Resource 1.), suggesting that the deteriorated signal from the affected eye may be effectively processed for the binocular vision. Metamorphopsia for binocular vision could be detected using M-CHARTS; however, the degree of metamorphopsia might be so subtle that it was imperceptible in daily life.
This study had some limitations. First, the observation period was short, and hence, it was difficult to assess the long-term prognoses of the mono- and binocular metamorphopsia. Second, we did not evaluate the impact of the mono- and binocular metamorphopsia on the visual disabilities at the individual level that contribute to tasks such as reading and face discrimination.
In conclusion, using M-CHARTS, this study showed that a high degree of metamorphopsia in the affected eyes could cause binocular metamorphopsia. Further prospective studies are needed to understand the effects of binocular metamorphopsia on the long-term course, effects of treatments, and impact on visual disability.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Shahid H, Hossain P, Amoaku WM (2006) The management of retinal vein occlusion: is interventional ophthalmology the way forward? Br J Ophthalmol 90:627–639. https://doi.org/10.1136/bjo.2005.068668
Klein R, Moss SE, Meuer SM, Klein BE (2008) The 15-year cumulative incidence of retinal vein occlusion: the beaver dam eye study. Arch Ophthalmol 126:513–518. https://doi.org/10.1001/archopht.126.4.513
Mitchell P, Smith W, Chang A (1996) Prevalence and associations of retinal vein occlusion in Australia. the blue mountains eye study. Arch Ophthalmol 114:1243–1247. https://doi.org/10.1001/archopht.1996.01100140443012
Noma H, Funatsu H, Mimura T, Harino S, Shimada K (2011) Functional-morphologic correlates in patients with branch retinal vein occlusion and macular edema. Retina 31:2102–2108. https://doi.org/10.1097/IAE.0b013e318212e24d
Morikawa S, Okamoto F, Murakami T, Sugiura Y, Hiraoka T, Oshika T (2022) Visual functions affecting stereopsis in patients with branch retinal vein occlusion. Eye 36:457–462. https://doi.org/10.1038/s41433-021-01452-x
Campochiaro PA, Heier JS, Feiner L, Gray S, Saroj N, Rundle AC, Murahashi WY, Rubio RG, Investigators BRAVO (2010) Ranibizumab for macular edema following branch retinal vein occlusion: six-month primary end point results of a phase III study. Ophthalmology 117:1102-1112.e1. https://doi.org/10.1016/j.ophtha.2010.02.021
Clark WL, Boyer DS, Heier JS, Brown DM, Haller JA, Vitti R, Kazmi H, Berliner AJ, Erickson K, Chu KW, Soo Y, Cheng Y, Campochiaro PA (2016) Intravitreal aflibercept for macular edema following branch retinal vein occlusion: 52-week results of the VIBRANT study. Ophthalmology 123:330–336. https://doi.org/10.1016/j.ophtha.2015.09.035
Thach AB, Yau L, Hoang C, Tuomi L (2014) Time to clinically significant visual acuity gains after ranibizumab treatment for retinal vein occlusion: BRAVO and CRUISE trials. Ophthalmology 121:1059–1066. https://doi.org/10.1016/j.ophtha.2013.11.022
Mitry D, Bunce C, Charteris D (2013) Anti-vascular endothelial growth factor for macular oedema secondary to branch retinal vein occlusion. Cochrane Database Syst Rev 7:Cd009510. https://doi.org/10.1002/14651858.CD009510.pub3
Pham B, Thomas SM, Lillie E, Lee T, Hamid J, Richter T, Janoudi G, Agarwal A, Sharpe JP, Scott A, Warren R, Brahmbhatt R, Macdonald E, Straus SE, Tricco AC (2019) Anti-vascular endothelial growth factor treatment for retinal conditions: a systematic review and meta-analysis. BMJ Open 9:e022031. https://doi.org/10.1136/bmjopen-2018-022031
Varma R, Bressler NM, Suñer I, Lee P, Dolan CM, Ward J, Colman S, Rubio RG (2012) Improved vision-related function after ranibizumab for macular edema after retinal vein occlusion: results from the BRAVO and CRUISE trials. Ophthalmology 119:2108–2118. https://doi.org/10.1016/j.ophtha.2012.05.017
Heier JS, Campochiaro PA, Yau L, Li Z, Saroj N, Rubio RG, Lai P (2012) Ranibizumab for macular edema due to retinal vein occlusions: long-term follow-up in the HORIZON trial. Ophthalmology 119:802–809. https://doi.org/10.1016/j.ophtha.2011.12.005
Scott IU, VanVeldhuisen PC, Ip MS, Blodi BA, Oden NL, Awh CC, Kunimoto DY, Marucs DM, Wroblewski JJ, King J, SCORE2 Investigator Group (2017) Effect of bevacizumab vs aflibercept on visual acuity among patients with macular edema due to central retinal vein occlusion: the SCORE2 randomized clinical trial. JAMA 317:2072–2087. https://doi.org/10.1001/jama.2017.4568
Murakami T, Okamoto F, Iida M, Sugiura Y, Okamoto Y, Hiraoka T, Oshika T (2016) Relationship between metamorphopsia and foveal microstructure in patients with branch retinal vein occlusion and cystoid macular edema. Graefes Arch Clin Exp Ophthalmol 254:2191–2196. https://doi.org/10.1007/s00417-016-3382-2
Nakagawa T, Harino S (2007) Iwahashi Y (2007) [Quantification of metamorphopsia in the course of branch retinal vein occlusion with M-CHARTS]. Nippon Ganka Gakkai Zasshi 111:331–335
Sugiura Y, Okamoto F, Morikawa S, Okamoto Y, Hiraoka T, Oshika T (2018) Time course of changes in metamorphopsia following intravitreal ranibizumab injection for branch retinal vein occlusion. Retina 38:1581–1587. https://doi.org/10.1097/iae.0000000000001740
Sugiura Y, Okamoto F, Murakami T, Morikawa S, Hiraoka T, Hussnain SA, Oshika T (2021) Relationship between metamorphopsia and inner retinal microstructure following intravitreal ranibizumab injection for branch retinal vein occlusion. Sci Rep 11:4454. https://doi.org/10.1038/s41598-021-84038-7
Manabe K, Tsujikawa A, Osaka R, Nakano Y, Fujita T, Shiragami C, Hirooka K, Uji A, Muraoka Y (2016) Metamorphopsia associated with branch retinal vein occlusion. PLoS ONE 11:e0153817. https://doi.org/10.1371/journal.pone.0153817
Osaka R, Manabe K, Manabe S, Nakano Y, Takasago Y, Shiragami C, Hirooka K, Muraoka Y, Tsujikawa A (2018) Persistent metamorphopsia associated with branch retinal vein occlusion. PLoS ONE 13:e0204015. https://doi.org/10.1371/journal.pone.0204015
Arimura E, Matsumoto C, Okuyama S, Takada S, Hashimoto S, Shimomura Y (2005) Retinal contraction and metamorphopsia scores in eyes with idiopathic epiretinal membrane. Invest Ophthalmol Vis Sci 46:2961–2966. https://doi.org/10.1167/iovs.04-1104
Watanabe A, Arimoto S, Nishi O (2009) Correlation between metamorphopsia and epiretinal membrane optical coherence tomography findings. Ophthalmology 116:1788–1793. https://doi.org/10.1016/j.ophtha.2009.04.046
Kinoshita T, Imaizumi H, Okushiba U, Miyamoto H, Ogino T, Mitamura Y (2012) Time course of changes in metamorphopsia, visual acuity, and OCT parameters after successful epiretinal membrane surgery. Invest Ophthalmol Vis Sci 53:3592–3597. https://doi.org/10.1167/iovs.12-9493
KinositaT IH, Miyamoto H, Okushiba U, Hayashi Y, Katome T, Mitamura Y (2015) Changes in metamorphopsia in daily life after successful epiretinal membrane surgery and correlation with M-CHARTS score. Clin Ophthalmol 9:225–233. https://doi.org/10.2147/OPTH.S76847
Achiron A, Lagstein O, Glick M, Gur Z, Bartov E, Burgansky-Eliash Z (2015) Quantifying metamorphopsia in patients with diabetic macular oedema and other macular abnormalities. Acta Ophthalmol 93:e649-653. https://doi.org/10.1111/aos.12735
Etheridge T, Dobson E, Wiedenmann M, Oden N, VanVeldhuisen P, Scott IU, Ip MS, Eliceiri KW, Blodi BA, Domalpally A (2021) Ellipsoid zone defects in retinal vein occlusion correlates with visual acuity prognosis: SCORE2 report 14. Transl Vis Sci Technol 10:31. https://doi.org/10.1167/tvst.10.3.31
Wang J, Cui Y, Vingopoulos F, Kasetty M, Silverman RF, Katz R, Kim L, Miller JB (2022) Disorganisation of retinal inner layers is associated with reduced contrast sensitivity in retinal vein occlusion. Br J Ophthalmol 106:241–245. https://doi.org/10.1136/bjophthalmol-2020-317615
Tzaridis S, Herrmann P, Charbel Issa P, Degli Esposti S, Wagner SK, Fruttiger M, Egan C, Rubin G, Holz FG, Heeren T (2019) Binocular inhibition of reading in macular telangiectasia type 2. Invest Ophthal Vis Sci 60:3835–3841. https://doi.org/10.1167/iovs.18-26414
Rubin GS, Muñoz B, Bandeen-Roche K, West SK (2000) Monocular versus binocular visual acuity as measures of vision impairment and predictors of visual disability. Invest Ophthal Vis Sci 41:3327–3334
Silvestri V, Sasso P, Piscopo P, Amore F, Rizzo S, Devenyi RG, Tarita-Nistor L (2020) Reading with central vision loss: binocular summation and inhibition. Ophthalmic Physiol Opt 40:778–789. https://doi.org/10.1111/opo.12726
Funding
This work was supported in part by a grant-in-aid for scientific research (no. 20K09771) from the Japan Society for the Promotion of Science (Tokyo, Japan) and Canon, Inc. (Tokyo, Japan). These organizations had no role in the design or conduct of this research. The funders had no role in the study design, data collection and analysis, decision to publish, or manuscript preparation.
Author information
Authors and Affiliations
Contributions
Conception and design: RO, YMu; data analysis and interpretation: RO, YMu, DN, YMi, NN; writing of the article: RO, YM; critical revision of the article: YMi, SK, TM, SO, KS, HT, AT. All authors have approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Yuki Muraoka received a grant and financial support from Bayer Yakuhin, Novartis Pharma, Canon, Alcon Japan, Santen Pharmaceutical, Senju Pharmaceutical, and AMO Japan. Yoshinori Mitamura received financial support from Santen Pharmaceutical, AMO Japan, Senju Pharmaceutical, Alcon Japan, Otsuka Pharmaceutical and HOYA. Tomoaki Murakami received grants and financial support from Bayer Yakuhin, Kowa Pharmaceutical, Alcon Pharma, Novartis Pharma, AMO Japan, Santen Pharmaceutical, Alcon Japan, and Senju Pharmaceutical. Kiyoshi Suzuma has received grants and financial support from Pfizer, Novartis Pharma, Bayer Yakuhin, Alcon Japan, Santen Pharmaceutical, Senju Pharmaceutical, Kowa, HOYA, and AMO Japan. Akitaka Tsujikawa received grants and financial support from Canon, Findex, Santen Pharmaceutical, Kowa Pharmaceutical, Pfizer, AMO Japan, Senju Pharmaceutical, Wakamoto Pharmaceutical, Alcon Japan, Alcon Pharma, Otsuka Pharmaceutical, Tomey Corporation, Taiho Pharma, HOYA, Bayer Yakuhin, Novartis Pharma, Chugai Pharmaceutical, Astellas, Eisai, Daiichi-Sankyo, Janssen Pharmaceutical, Kyoto Drug Discovery & Development, Allergan Japan, MSD, Ellex, Sanwa Kagaku Kenkyusho, Nitten Pharmaceutical, and AbbVie GK. Rie Osaka, Daisuke Nagasato, Naomi Nishigori, and Hitoshi Tabuchi declare no potential conflicts of interest. None of the aforementioned funding sources were involved in the design, conduct, preparation, or writing of this study or the manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the Ethics Committees of the Kagawa University Faculty of Medicine (Kagawa, Japan), Kyoto University Graduate School of Medicine (Kyoto, Japan), Tokushima University Faculty of Medicine (Tokushima, Japan), and Saneikai Tsukazaki Hospital (Hyogo, Japan).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent to publish
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Osaka, R., Muraoka, Y., Nagasato, D. et al. Binocular metamorphopsia in patients with branch retinal vein occlusion: a multi-center study. Int Ophthalmol 43, 3279–3286 (2023). https://doi.org/10.1007/s10792-023-02731-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-023-02731-0