Abstract
Purpose
Retinopathy of prematurity (ROP) progression is an inter-play of various perinatal and neonatal angiogenic and inflammatory cytokines. A small subset of ROP progresses to ROP requiring treatment. The present study was conducted with the aim to determine whether levels of IL-6, IL-8 and VEGF in serum and urine at the time of first ROP screening visit could be a biomarker for the prediction of development of treatable ROP.
Method
Prospective single-center observational study of preterm babies screened for ROP. Blood and urine samples were collected as a part of routine sampling at initial ROP screening visit and stored at −80 °C for further processing. The babies were followed up and grouped into ‘Group A’ comprising of 35 babies who developed treatable ROP and ‘Group B’ comprising of 36 babies with regressed ROP or no ROP. The evaluation of blood and urine samples was done for IL6, IL8 and VEGF by solid-phase sandwich RayBio® Human ELISA kit.
Results
The median serum values for IL-6, IL-8 and VEGF in Group A and Group B were 5.8 pg/ml (IQR 1.5,128.5) and 8.7 pg/ml (IQR 1.5,30.5), 55.9 pg/ml (IQR 28.0, 392.9) and 27.0 pg/ml (IQR 20.5,444.9) and 26.6 pg/ml (IQR 6.3, 39.4) and 30.0 pg/ml (IQR9.2,70.3), respectively. Group A had significantly increased levels of IL-8 (p < 0.05). However, AUROC curve for serum IL-8 demonstrated suboptimal discriminating ability.
Conclusion
Babies developing ROP requiring treatment had significantly increased levels of IL-8 in the serum at the time of initial screening. However, it could not serve as predictor for treatable ROP.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Retinopathy of prematurity (ROP) is a vaso-proliferative disorder of the developing retina and is a major cause of acquired childhood blindness [1].The worldwide incidence of ROP varies from 20 to 51.9% [2, 3]. Up to 15% of screened babies progress to develop treatable ROP [4]. It is estimated that around 14.5 million children are born prematurely every year worldwide, out of which 1,84,700 children develop any stage of ROP. Of these, 20,000 suffer blindness or severe visual impairment.1In high-income countries where most of the babies have access to high-quality neonatal care, ROP-associated blindness is uncommon. On the other hand, developing countries have not only the highest number of preterm births but also suboptimal infrastructure and capacity to screen these babies.
ROP is a biphasic disease consisting of an initial phase of blunted vascular growth characterized by low vascular endothelial growth factor (VEGF) and insulin-like growth factor (IGF-1) levels followed by a second phase of vaso-proliferation with an increase in VEGF and other pro-angiogenic markers [5]. Angiogenesis, the fundamental process involved in the development of retinal vasculature, is tightly regulated by a complex network of various factors in a time-dependent fashion. Although inflammatory cytokines can modulate angiogenesis [6, 7], their role in triggering the dysregulated angiogenesis in ROP has not been fully understood. Recent evidence suggests that prenatal, perinatal, and post-natal inflammation might contribute to a gradual increase in the risk for ROP [7]. Upregulation of pro-inflammatory cytokines is seen in hypoxic neonatal retina in rats [8].Cytokines such as IL-1β, TNF-α, and IL-6 act as primary initiators of inflammation following infection or tissue damage with cytokine receptor activation leading to downstream upregulation of effector molecules such as chemokines. Some of the chemokines studied for ROP pathophysiology include IL-8, IL6, monocyte chemotactic protein-1, and interferon-inducible T-cell alpha chemoattractant (I-TAC).
IL-8 has been implicated in both inflammation and pathological neovascularization in the eye [7, 9]. In adults, IL-8 is seen to play a major role in inflammation and angiogenesis in cornea, conjunctiva, iris and retina [9].
There is the scant literature on the inflammatory cytokines in ROP. The present study was conducted to determine whether the levels of IL-6, IL-8 and VEGF levels, in the serum and/or urine, at initial ROP screening of babies [10], could predict the development of ROP requiring treatment as per ETROP criteria (Type1 ROP) [11]. We hypothesized that serum inflammatory interleukins and VEGF at initial screening could have a role in progression to treatable ROP. We also hypothesized that urine analysis could act as a surrogate marker for the serum levels of these markers.
Material and methods
This was a hospital-based, institution review board (IRB) approved, prospective observational study involving preterm babies done between January 2020 and October 2020. Eligible neonates were enrolled after obtaining a written informed consent from the parents. The preterm babies with birth weight ≤ 2000 g and gestational age ≤ 34 weeks who were screened for ROP [10] were eligible for enrollment. We excluded neonates with major congenital abnormalities, hydrocephalus, necrotizing enterocolitis, periventricular leukomalacia, any evidence of TORCH infection or babies born to a mother with gestational metabolic diseases or TORCH infection.
A detailed history was taken and gender, gestational age, post-conception age, birth weight, duration of ventilation, multiplicity, any existing co-morbidities or congenital abnormality were recorded. Enrolled babies were screened for ROP by an ophthalmologist (SN) with more than 20 years of experience in managing ROP. At the time of first screening for ROP, i.e., 3–4 weeks of post-natal age, three ml of blood samples was collected as part of routine sampling. After centrifugation, the serum was separated and stored at −80 °C. Five ml of urine sample was also collected into a sterile or disposable container and stored at −80 °C. The screening examination was conducted under topical anesthesia (2% proparacaine) using a + 20 D lens, an indirect ophthalmoscope, a pediatric eye speculum and a wire Vectis for globe rotation. The exact stage and zone of ROP along with the presence of plus disease were recorded as per ICROP classification [12]. Preterm neonates were screened and followed up till the development of treatable ROP as per the ETROP study [11] (Type1 ROP requiring treatment) or till complete vascularization till ora-serrata or till 45 weeks of post-menstrual age. The mean time gap between the sampling and treatment was 4 weeks.
Group A (n = 35) comprised of the neonates who developed ROP needing treatment in either eye (type 1 ROP) at any time during study. Group B or the control group (n = 36) comprised of gestational age-matched neonates from the remaining cohort, who did not develop ROP needing treatment in both the eyes (type 2 ROP or no ROP). For the purpose of classification as case or control, the worst stage of ROP in either eye was considered.
Outcome measurement
Quantitative analysis of systemic IL-6, IL-8 and VEGF was done in batches by solid-phase sandwich ELISA technique. The IL-6 and IL8 levels were measured using DIACLONE IL-6/IL8 ELISA kit. VEGF level was assessed using RayBio® Human VEGF-A ELISA kit. Readings were taken using Tecan’s Magellan™ universal ELISA reader. The minimum detectable concentration was 2 pg/ml, 29 pg/ml and 10 pg/ml for IL-6, IL-8 and VEGF, respectively. Intra-assay and inter-assay coefficient of variation (CV %) for all parameters was < 10% in all the kits. The data collected were analyzed, and expression of biomarkers in blood and urine samples was determined.
Statistical analysis
The sample size in the study was calculated to detect differences in the main outcome measure, that is, IL-6 in the study. In the study by Silveira et al., IL-6 levels were reported to be 72 ± 172 pg/ml in neonates without ROP and 302 ± 1583 in neonates with severe ROP[13]. To detect at least twofold increase in levels of IL-6 with 80% power and two-sided alpha error of 5%, 35 neonates were required to be enrolled in each group.
Data were collected in an Excel database (Microsoft office 2019; Microsoft Inc). Data analysis was performed using Stata 16.1 (College Station, TX). Depending on distribution, numerical data were analyzed using t test or Mann–Whitney U Test. Categorical data were analyzed using chi-square test or Fisher exact test. Correlation was analyzed using Spearman’s correlation coefficient. P value < 0.05 was considered as significant. Receiver operating characteristic (ROC) curves were analyzed for all cytokines studied. Once the final diagnosis of ROP was made by indirect ophthalmoscopy, the cutoff point for each cytokine was detected and the best cutoff point of each cytokine was then used to compare Group A and Group B.
Results
A total of 249 neonates were screened for ROP during the study period. Of these, 78 neonates fulfilled the inclusion criteria. Seven babies were excluded based on predefined criteria. (Fig. 1). Of the 35 babies with ROP, Zone 1 (A-ROP in 7) and Zone II (AROP in 6) ROP was seen in 7 and 28 eyes, respectively. Stage 2, Stage 3, Stage 4 A, and Stage 5 ROP was seen in 7, 11, 2, 2 babies, respectively. The babies with stage 4 and 5 were those who had missed their screening visits due to lock down during COVID-19 pandemic. All babies had symmetrical ROP. As neonates eligible to be enrolled as controls were not available as gestation matching pairs, we enrolled neonates from the available cohort of neonates without ROP. Thirty-six neonates who did not develop treatable ROP were included as controls. Of these, 24 developed type 2 ROP which regressed spontaneously and 12 did not develop any ROP. All the neonates with ROP had symmetrical disease in both eyes.
In comparison to controls, the cases had lower birth weight (1309 ± 244 g vs. 1524 ± 297 g) and smaller gestational age (30.2 ± 1.8 weeks vs. 32.0 ± 1.5 weeks). Cases were more likely to have respiratory distress syndrome (86% vs. 33%) and needed longer duration of respiratory support including oxygen, CPAP, and invasive ventilation (Table 1). The blood and urine samples were collected at the time of first screening examination. The post-conceptual age (PCA) at the time of sample collection in cases and controls was 34.8 ± 3.1 weeks and 36.0 ± 1.7 weeks, respectively.
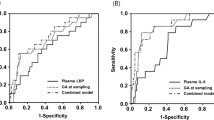
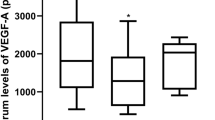
The details of the level of biomarkers are given in Table 2. Serum IL-6 and VEGF levels were similar in cases and controls. However, serum IL-8 levels were significantly higher in cases (median [IQR]: 55.9 [28.0 to 392.9] vs. 27.0 [20.5 to 441.9], P = 0.048). Levels of all the three markers were comparable in urine. The area under the ROC curve (AUROC) for serum IL-8 predicting case vs control was 0.636 (95% CI: 0.501–0.771), thus demonstrating poor diagnostic performance (Figs. 2, 3, 4).
Fundus picture of baby of birthweight 900 g, gestational age of 31 weeks with transient tachypnoea of newborn, showing Zone I A-ROP with initial screening serum IL-6 of 200 pg/ml, IL-8 2000 pg/ml and VEGF 31.5 pg/ml. Figure 4 inset fluorescein angiogram of the same eye showing large avascular area extending to zone I
IL-6 levels in serum showed positive correlation with IL-8 levels in serum, (p = 0.002). For every 1 unit increase in IL-6 (serum), the IL-8 (serum) increased by 2.32 units. Also, moderate positive correlation was seen in IL-8 in serum with IL-6 level in urine (p = 0.06). IL-8 in urine showed positive correlation with VEGF level in urine (p = 0.049). Both IL-8 and IL-6 levels had a positive effect on each other. If the level of one increased, levels of other parameters increased in concentration in both serum and urine.
In controls, positive correlation of IL-6 level in serum was seen in association with IL-8 level in serum (p = 0.075) and VEGF level in serum (p = 0.041). Urinary levels of IL-6 increased as IL-8 and VEGF in urine increased (p = 0.04 and p = 0.4). With rise in IL-8 in urine, rise in VEGF level in urine was seen in the control group (p = 0.046).
Association of stages and zones with biomarkers was also studied, and it was seen that higher levels of IL-6 and IL-8 in serum were present with increasing stages of the disease. VEGF level in serum and urinary levels of each biomarker showed no significant difference between various stages and zones, but values of IL-8 level in urine were higher as compared to other parameters.
Correlation between serum and urine levels of IL-6 (r = 0.07), IL-8 (r = −0.10) and VEGF in cases (r = 0.07) was poor.
Discussion
The pathogenesis of ROP remains a dilemma for the treating ophthalmologists. The role of vasculogenesis and angiogenesis has been vastly studied in ROP, but the inter-play of inflammatory biomarkers causing the disease is not well understood [7, 13]. Some studies have described the effect of multiple “hits” of exposure from various risk factors, like perinatal inflammation, oxygen supplementation, lower gestational birth or neonatal sepsis, on the development of severe form of ROP [7, 8]. Despite the documented affirmed role of various risk factors in ROP, etiology behind the inflammation is still not very clear. In a study by Rathi et al., the authors have done quantitative analysis of the cytokines in the tear film and the vitreous sample of eyes with severe ROP [14], while Vinekar A et al. studied the status of pro-angiogenic factors in the tear fluid of preterm infants with and without ROP [15]. However, in the present study, we studied the role of inflammatory cytokines in the blood and urine samples of babies undergoing ROP screening as a predictive tool for the development of severe ROP. The determination of systemic inflammatory biomarkers in babies with ROP could help in the better understanding of the disease.
In the present study, the mean birth weight of babies developing treatable ROP was 1309 ± 244 g and the mean gestational age was 30.2 ± 1.8 weeks which was significantly lower than the control group (p < 0.001). Birth weight and gestational age are major risk factors for ROP. However, the birth weight and gestational age in our cohort are higher than that reported by the Cryo-ROP study or the ETROP study [2, 11]. Lately, ROP has been reported in babies with higher birth weight and larger gestational age [16, 17]. Among the neonatal morbidity factors, respiratory distress syndrome (RDS), longer duration of respiratory support including oxygen, CPAP, and invasive ventilation were the only risk factors significantly associated (p = < 0.001) with the development of ROP which is in concurrence with previous studies [17, 18].
In the present study, IL-8 levels in blood were significantly raised in cases (55.9 pg/ml) in comparison to controls (27 pg/ml). The levels were much higher than the normal values as seen in healthy neonates where IL-8 in serum has been found to be in the 8- 21.1 pg/ml range [19]. There were other factors like respiratory distress syndrome, CPAP which could also be the contributing factors for IL8, but these are established risk factors for ROP.
IL-8 has broad spectrum effects on neutrophil recruitment in inflammation, cell adhesion, honing of neutrophils and lymphocytes, tumor growth, angiogenesis, neuronal protection and brain development. The raised levels of IL-8 have been seen in various vitreoretinal diseases like retinal vein occlusion, diabetic macular edema, age-related macular degeneration, suggesting a common pathway for angiogenesis in these diseases [9]. IL-8 has been correlated with raised IL-6 levels in numerous eye diseases which highlights the role of inflammation in these diseases. In the present study also, for every unit increase in IL-6 levels, there was 2.32 unit increase in IL-8 levels. This is consistent with earlier studies where the levels of IL-6 and IL-8 positively correlate with each other in anterior segment diseases with manifest inflammation or occult inflammation associated with hypoxia [20].
It was also seen that IL-8 levels in serum were more as compared to IL-6 levels which might be due to short half-life of IL-6 which remains active only for the first few days of inflammation. However, the levels could not be used as the predictor for disease progression and the area under the ROC curve demonstrated poor diagnostic performance.
Sood et al. have studied the role of cytokines with perinatal inflammatory response and have observed that although IL-6 was significantly associated with ROP, the association could only be seen at day 14 of birth and not thereafter making it a less reliable or less specific marker[21]. In the present study, the sample was withdrawn once at the time of initial screening, which is 3–4 weeks after birth. Sequential samples could have given us more information.
The mean value of VEGF in serum of cases (30 ± 33 pg/ml) and controls (43 ± 36 pg/ml) was comparable (p = 0.08). Lower levels of VEGF in infants with ROP compared with infants without ROP have been previously documented[15]. Hellgren et al. studied the median VEGF concentrations in cord blood and concluded that no correlation was present between VEGF levels at birth with later development of ROP [22]. It was found that serum VEGF levels peaked at the first detection of ROP and not at the time of laser treatment or proliferative stage of ROP. The authors concluded that no significant change occurs in the levels of serum VEGF when the samples were taken before the treatment or within 2 weeks after giving treatment. Pieh et al. investigated longitudinal VEGF concentrations where they have reported no differences in VEGF levels in serum in ROP and the control group in a subgroup of patients between 32 and 36 weeks of post-menstrual age [23]. It has been seen in different studies that various risk factors may play a role in keeping sustained high levels of plasma VEGF like bronchopulmonary dysplasia or supplemental oxygen therapy, in the absence of which VEGF levels in the blood usually come to low levels in a few weeks[24]. In the present study, we did not observe any difference between cases and controls in samples collected at 34.8 weeks of PCA which is consistent with the two above-mentioned studies. There are possibly other serum biomarkers or genetic factors which play a role in the development of ROP.
An alternative treatment to laser is desired as even in the present era with vast research work being done, adequate available treatment of ROP is still associated with unsuccessful visual outcome and recurrence of the disease. As an alternative treatment immune targeting of IL-8 by anti-IL-8 cytokines like IL-10 or medications like cholecalciferol or steroids early in life may be studied to prevent the occurrence of ROP[9]. Systemic biomarkers analysis can help us in targeting concerned biomarker in the early neonatal phase so as to avoid the future occurrence of Type 1 ROP even before screening and can help us in predicting the babies who are likely to develop a severe form of ROP in future.
The main limitation of our study was that we could not achieve the exact gestation age matching in the two groups as neonates with ROP were of significantly lower gestation and this could be the confounding factor. Moreover, in the present study, the PCA at the time of sample collection in cases and controls was 34.8 ± 3.1 weeks and 36.0 ± 1.7 weeks, respectively. Neonates of lower gestation who are more prone to develop ROP are screened for the first time by 3 weeks of post-natal age, while relatively mature neonates who would not have developed ROP were screened after completing 4 weeks of age. This accounts for a difference of about 1 week in the post-conceptional age. Circulating chemokine can bind to neutrophils, and therefore, plasma IL8 may not be a true indicator of total IL8 and plasma IL-8 reflects only a portion of the total IL-8 blood pool. Moreover, there was only one-time assessment of biomarkers. The serial longitudinal analysis could have given us a better understanding while studying the pattern of association.
To conclude, babies requiring treatment requiring ROP had significantly increased levels of IL-8 which are seen at the time of initial screening. In future, IL-8 may be used as a new biomarker or therapeutic tool for treatable ROP. More prospective studies are required in this direction. If validated by further studies, the incorporation of the quantitative assessment of IL-8 in blood and urine samples as a routine test in premature infants may help predict the course of ROP in these infants.
References
Gilbert C, Foster A (2001) Childhood blindness in the context of VISION 2020: the right to sight. Bull World Health Organ 79:227–232
Quinn GE (2016) Retinopathy of prematurity blindness worldwide: phenotypes in the third epidemic. Eye brain 8:31–36
Honavar SG (2019) Do we need India-specific retinopathy of prematurity screening guidelines? Indian J Ophthalmol 67:711–716
Jayadev C, Vinekar A, Bharamshetter R, Mangalesh S, Rao HL, Dogra M et al (2019) Retinal immaturity at first screening and retinopathy of prematurity. Image-based validation of 1202 eyes of premature infants to predict disease progression. Indian J Ophthalmol 67:846–53
Flynn JT, Chan-Ling T (2006) Retinopathy of prematurity: two distinct mechanisms that underlie zone 1 and zone 2 disease. Am J Ophthalmol 142:46–59
Chen J, Smith LEH (2007) Retinopathy of prematurity. Angiogenesis 10:133–140
Lee J, Dammann O (2012) Perinatal infection, inflammation, and retinopathy of prematurity. Semin Fetal Neonatal Med 17:26–29
Sivakumar V, Foulds WS, Luu CD, Ling EA, Kaur C (2011) Retinal ganglion cell death is induced by microglia derived pro-inflammatory cytokines in the hypoxic neonatal retina. J Pathol 224:245–260
Ghasemi H, Ghazanfari T, Yaraee R, Faghihzadeh S, Hassan ZM (2011) Roles of IL-8 in ocular inflammations: a review. Ocul Immunol Inflamm 19:401–412
Pejawar R, Vinekar A, Bilagi A. National Neonatology Foundation’s Evidence-based Clinical Practise Guidelines, Retinopathy of Prematurity, NNF India, New Delhi 2010:253–62
Early Treatment for Retinopathy of Prematurity Cooperative Group (2003) Revised indications for the treatment of retinopathy of prematurity: results of the early treatment for retinopathy of prematurity randomized trial. Arch Ophthalmol 121:1684–1694
The International Committee for Classification of Retinopathy of Prematurity (2005) International classification of retinopathy of prematurity revisited. Arch Ophthalmol 123:991–9
Silveira RC, Fortes Filho JB, Procianoy RS (2011) Assessment of the contribution of cytokine plasma levels to detect retinopathy of prematurity in very low birth weight infants. Invest Ophthalmol Vis Sci 52:1297–1301
Rathi S, Jalali S, Patnaik S, Shahulhameed S, Musada GR, Balakrishnan D, Rani PK, Kekunnaya R, Chhablani PP, Swain S, Giri L, Chakrabarti S, Kaur I (2017) Abnormal complement activation and inflammation in the pathogenesis of retinopathy of prematurity. Front Immunol 8:1868
Vinekar A, Nair AP, Sinha S et al (2021) Tear fluid angiogenic factors: Potential noninvasive biomarkers for retinopathy of prematurity in preterm infants. Invest Ophthalmol Vis Sci 62:2
Dwivedi A, Dwivedi D, Lakhtakia S, Chalisgaonkar C, Jain S (2019) Prevalence, risk factors and pattern of severe retinopathy of prematurity in eastern Madhya Pradesh. Indian J Ophthalmol 67:819–823
Kumar P, Sankar MJ, Deorari A, Azad R, Chandra P, Agarwal R, Paul V (2011) Risk factors for severe retinopathy of prematurity in preterm low birth weight neonates. Indian J Pediatr 78:812–816
Dutta S, Narang S, Narang A, Dogra M, Gupta A (2004) Risk factors of threshold retinopathy of prematurity. Indian Pediatr 41:665–671
Boskabadi H, Maamouri G, TavakolAfshari J et al (2013) Evaluation of serum interleukins-6, 8 and 10 levels as diagnostic markers of neonatal infection and possibility of mortality. Iran J Basic Med Sci 16:1232–1237
Zenkel M, Lewczuk P, Junemann A, Kruse FE, Naumann GOH, Schlotzer-Schrehardt U (2010) Pro-inflammatory cytokines are involved in the initiation of the abnormal matrix process in Pseudoexfoliation syndrome/glaucoma. Am J Pathol 176:2868–2879
Sood BG, Madan A, Saha S, Schendel D, Thorsen P, Skogstrand K et al (2010) Perinatal systemic inflammatory response syndrome and retinopathy of prematurity. Pediatr Res 67:394–400
Hellgren G, Löfqvist C, Hård AL, Hansen-Pupp I, Gram M, Ley D, Smith LE, Hellström A (2016) Serum concentrations of vascular endothelial growth factor in relation to retinopathy of prematurity. Pediatr Res 79:70–75
Pieh C, Agostini H, Buschbeck C, Kruger M, Schulte-Monting J, Zirrgiebel U et al (2008) VEGF-A, VEGFR-1, VEGFR-2 and Tie2 levels in plasma of premature infants: relationship to retinopathy of prematurity. Br J Ophthalmol 92:689–93
Chen X, Zhou L, Zhang Q, Xu Y, Zhao P, Xia H (2019) Serum vascular endothelial growth factor levels before and after intravenous ranibizumab injection for retinopathy of prematurity. J Ophthalmol 2019(20):2985161
Funding
This study was not funded by any other agency.
Author information
Authors and Affiliations
Contributions
PS and SN wrote the main manuscript and evaluated babies for ROP stage and extent. DC and DK did the statistical analysis. SG and JK did the biomarker assay. SN, DC and SJ did the editing for the manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflict of interest
None of the authors has any conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from parents of all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sehgal, P., Narang, S., Chawla, D. et al. Systemic biomarkers of retinopathy of prematurity in preterm babies. Int Ophthalmol 43, 1751–1759 (2023). https://doi.org/10.1007/s10792-022-02576-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-022-02576-z