Abstract
Purpose
The study aims to describe modifications and refinements in the technique and technology of Transcanalicular Endoscopic Lacrimal Duct Recanalization (TELDR) based on anatomical foundations to optimize its clinical outcomes in patients with complete Primary Acquired Nasolacrimal Duct Obstruction (PANDO).
Methods
The medical records of 115 patients who underwent TELDR procedures from January 2018 to July 2020 were reviewed retrospectively. Of the 115 patients, only those 35 patients with complete PANDO characterized by longstanding epiphora of 3–5 years duration, dense, diffuse fibrous tissue obstruction involving the sac, sac duct junction and the entire length of the nasolacrimal duct were included in the study. Parameters for success were analyzed based on patency on irrigation, functional endoscopic dye test, and improvement of epiphora.
Results
Forty-five cases from 35 patients with complete PANDO were included in the study. The mean length of time from the date of operation to silicone stent removal was 8.1 weeks, while the mean length of follow-up starting from the removal of silicone stent to last follow-up was 61.0 weeks. There were 95.6% anatomic patency on canalicular irrigation with saline and 95.6% functional patency based on functional endoscopic dye test. There was significant improvement of epiphora (p value of < 0.0001) post-operatively.
Conclusion
The results of modified TELDR improved clinical outcomes and could be a definitive treatment in patients with complete PANDO with longstanding, dense, diffuse, fibrous tissue obstruction. Patients who experience reobstruction, may undergo a repeat of the recanalization approach.






Similar content being viewed by others
Data availability
If editors or referees request, the author can share the patients’ data.
References
Pifaretti JM (1998) Endoscopie des voies lacrymales [endoscopy of the lacrimal ducts]. Klin Monatsbl Augenheilkd 212(5):259–260. https://doi.org/10.1055/s-2008-1034874
Haefliger IO, Piffaretti JM (2001) Lacrimal drainage system endoscopic examination and surgery through the lacrimal punctum. Klin Monbl Augenheilkd 218(5):384–387. https://doi.org/10.1055/s-2001-15907
Hong J, Qian T, Wei A et al (2016) Nasolacrimal recanalization as an alternative to external dacryocystorhinostomy for treating failed nasolacrimal duct intubation. Medicine 95(30):e4350. https://doi.org/10.1097/MD.0000000000004350
Athanasiov PA, Prabhakaran VC, Mannor G et al (2009) Transcanalicular approach to adult lacrimal duct obstruction: a review of instruments and methods. Ophthalmic Surg Lasers Imaging 40(2):149–159. https://doi.org/10.3928/15428877-20090301-04
Becker BB (2001) Recanalization of the obstructed nasolacrimal duct system. J Vasc Interv Radiol JVIR 12(6):697–699. https://doi.org/10.1016/s1051-0443(07)61439-0
Ali M, Paulsen F (2020) Human lacrimal drainage system reconstruction, recanalization, and regeneration. Curr Eye Res 45(3):241–252. https://doi.org/10.1080/02713683.2019.1580376
Guinot-Saera A, Koay P (1998) Efficacy of probing as treatment of epiphora in adults with blocked nasolacrimal ducts. Br J Ophthalmol 82(4):389–391. https://doi.org/10.1136/bjo.82.4.389
Bell TA (1986) An investigation into the efficacy of probing the nasolacrimal duct as a treatment for epiphora in adults. Trans Ophthalmol Soc U K 105(Pt 4):494–497
Yazici Z, Yazici B, Parlak M et al (1999) Treatment of obstructive epiphora in adults by balloon dacryocystoplasty. Br J Ophthalmol 83(6):692–696. https://doi.org/10.1136/bjo.83.6.692
Janssen AG, Mansour K, Bos JJ (1997) Obstructed nasolacrimal duct system in epiphora: long-term results of dacryocystoplasty by means of balloon dilation. Radiology 205(3):791–796. https://doi.org/10.1148/radiology.205.3.9393537
Satici A, Basar E, Guzey M (2004) Probing in adults with nasolacrimal duct obstruction. Hong Kong J Ophthalmol 8(1):8–11. https://hkjo.hk/index.php/hkjo/article/view/91. Accessed Jan 14, 2022
Berkefeld J, Kirchner J, Müller HM et al (1997) Balloon dacryocystoplasty: indications and contraindications. Radiology 205(3):785–790. https://doi.org/10.1148/radiology.205.3.9393536
Angrist RC, Dortzbach RK (1985) Silicone intubation for partial and total nasolacrimal duct obstruction in adults. Ophthalmic Plast Reconst Surg 1(1):51–54. https://doi.org/10.1097/00002341-198501000-00008
Wang Z, Huang Y, Chen W et al (2007) Diagnosis and treatment of lacrimal passage obstruction by lacrimal endoscope. J Huazhong Univ Sci Technol Med Sci 27(5):593–597. https://doi.org/10.1007/s11596-007-0530-2
Chen D, Ge J, Wang L et al (2009) A simple and evolutional approach proven to recanalise the nasolacrimal duct obstruction. Br J Ophthalmol 93(11):1438–1443. https://doi.org/10.1136/bjo.2008.149393
Ali MJ, Naik MN (2014) Efficacy of endoscopic guided anterograde 3 mm balloon dacryoplasty with silicone intubation in treatment of acquired partial nasolacrimal duct obstruction in adults. Saudi J Ophthalmol Off J Saudi Ophthalmol Soc 28(1):40–43. https://doi.org/10.1016/j.sjopt.2013.12.004
Perry JD, Maus M, Nowinski TS et al (1998) Balloon catheter dilation for treatment of adults with partial nasolacrimal duct obstruction: a preliminary report. Am J Ophthalmol 126(6):811–816. https://doi.org/10.1016/s0002-9394(98)00278-5
Javate R, Pamintuan F, Cruz R Jr (2010) Efficacy of endoscopic lacrimal duct recanalization using microendoscope. Ophthalmic Plast Reconstr Surg 26(5):330–333. https://doi.org/10.1097/IOP.0b013e3181c7577a
Lee SM, Lew H (2021) Transcanalicular endoscopic dacryoplasty in patients with primary acquired nasolacrimal duct obstruction. Graefe’s Arch Clin Exp Ophthalmol 259(1):173–180. https://doi.org/10.1007/s00417-020-04833-2
Paulsen FP, Thale AB, Maune S et al (2001) New insights into the pathophysiology of primary acquired dacryostenosis. Ophthalmology 108(12):2329–2336. https://doi.org/10.1016/s0161-6420(01)00946-0
Sasaki T, Nagata Y, Sugiyama K (2005) Nasolacrimal duct obstruction classified by dacryoendoscopy and treated with inferior meatal dacryorhinotomy. Part I: positional diagnosis of primary nasolacrimal duct obstruction with dacryoendoscope. Am J Ophthalmol 140(6):1065–1069. https://doi.org/10.1016/j.ajo.2005.07.038
Linberg JV, McCormick SA (1986) Primary acquired nasolacrimal duct obstruction. A clinicopathologic report and biopsy technique. Ophthalmology 93(8):1055–1063. https://doi.org/10.1016/s0161-6420(86)33620-0
Munk PL, Lin DT, Morris DC (1990) Epiphora: treatment by means of dacryocystoplasty with balloon dilation of the nasolacrimal drainage apparatus. Radiology 177(3):687–690. https://doi.org/10.1148/radiology.177.3.2243969
Lemke B, Della RR (1990) Surgery of the eyelids and orbit: an anatomical approach. In: Lemke BN, Della Rocca RC (eds) Lacrimal excretory osteology. Appleton and Lange, Connecticut, pp 96–101
Meyer-Rüsenberg HW, Emmerich KH (2010) Modern lacrimal duct surgery from the ophthalmological perspective. Deutsches Arzteblatt Int 107(14):254–258. https://doi.org/10.3238/arztebl.2010.0254
Agrawal S, Gupta SK, Singh V, Agrawal S (2013) A novel technique to recanalize the nasolacrimal duct with endodiathermy bipolar probe. Indian J Ophthalmol 61(12):718–721. https://doi.org/10.4103/0301-4738.121180
Javate R, Dy IE, Buyucan KF, Ma Guerrero EE (2016) Retention rates and benefits of painless punctal plug F(TM) in dry eye patients. Orbit 35(3):126–131. https://doi.org/10.1080/01676830.2016.1176204
Carter KD, Nelson CC, Martonyi CL (1988) Size variation of the lacrimal punctum in adults. Ophthalmic Plast Reconstr Surg 4(4):231–233. https://doi.org/10.1097/00002341-198804040-00006
Tucker NA, Tucker SM, Linberg JV (1996) The anatomy of the common canaliculus. Arch Ophthalmol 114(10):1231–1234. https://doi.org/10.1001/archopht.1996.01100140431010
Lee JM, Song HY, Han YM et al (1994) Balloon dacryocystoplasty: results in the treatment of complete and partial obstructions of the nasolacrimal system. Radiology 192(2):503–508. https://doi.org/10.1148/radiology.192.2.8029423
Takahashi Y, Suzuki T, Kakizaki H (2014) Lacrimal sac movement under intrasac pressure changes observed with dacryoendoscopy. Ophthalmic Plast Reconstr Surg 30(4):313–314. https://doi.org/10.1097/IOP.0000000000000099
Javate R (2012) Endoscopy and microendoscopy of the lacrimal drainage system. Endo-Press GmbH, Tuttlingen
Javate R, Pamintuan F, Lapid-Lim S (2011) Innovations in lacrimal surgery. UST Publishing House, Manila
Abele JE (1980) Balloon catheters and transluminal dilatation: technical considerations. AJR Am J Roentgenol 135(5):901–906. https://doi.org/10.2214/ajr.135.5.901
Kuchar A, Steinkogler FJ (2001) Antegrade balloon dilatation of nasolacrimal duct obstruction in adults. Br J Ophthalmol 85(2):200–204. https://doi.org/10.1136/bjo.85.2.200
Couch SM, White WL (2004) Endoscopically assisted balloon dacryoplasty treatment of incomplete nasolacrimal duct obstruction. Ophthalmology 111(3):585–589. https://doi.org/10.1016/j.ophtha.2003.06.013
Goldstein SM, Katowitz JA, Syed NA (2006) The histopathologic effects of balloon dacryoplasty on the rabbit nasolacrimal duct. J AAPOS Off Publ Am Assoc Pediatric Ophthalmol Strabismus 10(4):333–335. https://doi.org/10.1016/j.jaapos.2006.03.004
Aritürk N, Oge I, Oge F et al (1999) Silicone intubation for obstruction of the nasolacrimal duct in adults. Acta Ophthalmol Scand 77(4):481–482. https://doi.org/10.1034/j.1600-0420.1999.770429.x
Moscato EE, Dolmetsch AM, Silkiss RZ et al (2012) Silicone intubation for the treatment of epiphora in adults with presumed functional nasolacrimal duct obstruction. Ophthalmic Plast Reconstr Surg 28(1):35–39. https://doi.org/10.1097/IOP.0b013e318230b110
Acknowledgements
I am grateful to Mr. Raymark Salonga for his statistical analysis of our data, to Ann Carmeline Beronilla, M.D., Joy Katrina Bolusan R.N., and Nenita Sanchez, BSPsych for their technical assistance in the preparation of the article.
Funding
The author received no financial support for the research, authorship and/or publication of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Ethical approval
This study is in accordance with the guidelines of the Declaration of Helsinki of 1975, as revised in 2000 and submitted to the Research Ethics Committee of the University of Santo Tomas Hospital, Manila, Philippines (REC-2020-09-103-MD-FR).
Consent to participate
This is a retrospective study and only medical charts were reviewed.
Consent to publish
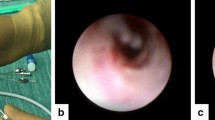
Informed consent was obtained by the author for publication of image in Figs. 3 and 4.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (MPG 336192 kb)
Rights and permissions
About this article
Cite this article
Javate, R.M. Optimizing clinical outcomes for endoscopic lacrimal duct recanalization in patients with complete PANDO. Int Ophthalmol 43, 175–184 (2023). https://doi.org/10.1007/s10792-022-02414-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-022-02414-2