Abstract
Purpose
Conjunctivitis is one of the most common ocular pathologies. Its treatment depends on its etiology, but an excessive use of antibiotics and corticosteroids, which in many cases are contraindicated, has been described. The objective was to describe the prescription patterns of medications used to treat conjunctivitis in a Colombian population.
Methods
This was a cross-sectional study on the pharmacological treatment of patients diagnosed with conjunctivitis between April 1, 2020, and March 31, 2021; based on a drug-dispensing database of approximately 8.5 million people affiliated with the Colombian Health System. Some sociodemographic and pharmacological variables and comorbidities were considered. A descriptive analysis was performed.
Results
A total of 8708 patients were identified; they had a median age of 44.7 years, and 59.3% were women. The most common causes of conjunctivitis were unspecified (53.1%) and allergic (37.4%). The most commonly used drug was olopatadine (26.1%), followed by dexamethasone with neomycin and polymyxin B (25.0%). A total of 97.0% of the patients received ophthalmic prescriptions, while 12.8% received systemic medications. Glucocorticoids (40.3%), antibiotics (37.7%) and antihistamines (31.7%) were the most commonly used groups of ophthalmic drugs. Glucocorticoids and ophthalmic antibiotics were the medications most frequently prescribed by general practitioners for the treatment of viral or bacterial conjunctivitis.
Conclusions
Many patients with conjunctivitis are not being managed according to the recommendations of clinical practice guidelines, which highlights that the widespread use of antibiotics with ophthalmic glucocorticoids could be considered potentially inappropriate prescriptions in many cases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Conjunctivitis is the inflammation or infection of the conjunctiva and is characterized by dilation of the conjunctival vessels that leads to hyperemia, edema, pain and ocular discharge [1, 2]. It is the most common ocular pathology, representing approximately 2.0% of all primary care consultations and 1.0% of emergency consultations [1, 3], and the majority of patients are initially managed by primary care physicians instead of ophthalmology professionals [1]. Its prevalence varies according to the underlying cause, the age of the patient and the season of the year [1]. However, in general, viral and allergic causes are the most frequent etiologies [1, 4, 5].
Conjunctivitis can be classified according to its etiology, chronicity and severity. In this way, conjunctivitis can be infectious (viral, bacterial or parasitic) or noninfectious (allergic, mechanical, irritative, toxic, immune-mediated or neoplastic); acute (lasting less than 4 weeks) or chronic (lasting more than 4 weeks); and mild or moderate/severe according to the intensity of its clinical manifestations [2, 4, 5]. Its treatment depends mainly on the underlying etiology; however, definitive diagnosis is a great challenge in making the definitive diagnosis due to the overlap of symptoms and the heterogeneous clinical presentation, and studies have shown a clinical inaccuracy rate that oscillates between 40.0 and 75.0% [3] and contributes to the inadequate management of patients [6].
Excessive use of ophthalmic antibiotics and glucocorticoids has been shown in patients with conjunctivitis [6, 7]. The former class of medications is indicated in for bacterial etiologies, while the latter can be used in some patients with allergic or atopic conjunctivitis that is refractory to treatment [8, 9]. The indiscriminate use of these drugs can lead to complications and adverse ophthalmological reactions, such as antimicrobial resistance, worsening infections or increasing intraocular pressure, among others [1, 10].
The Colombian Health System offers universal coverage to the entire population through two regimes: a contributory one that is paid by workers and employers, and another that is subsidized by the state. The health system includes a benefit plan that covers a significant number of heterogeneous medications used in the management of patients with conjunctivitis. The objective of this study was to determine the prescription patterns of medications used in the treatment conjunctivitis in a population of Colombians covered by the health system.
Materials and methods
A cross-sectional study was developed to establish the prescriptions used in the treatment of patients diagnosed with conjunctivitis based on a drug dispensing database that collects information from approximately 8.5 million people affiliated with the Colombian Health System through six health insurance companies, corresponding to approximately 30.0% of the active affiliated population of the contributory or payment regime and 6.0% of the state-subsidized regime and approximately 17.0% of the Colombian population during the study period.
Patients with a first diagnosis of conjunctivitis between April 1, 2020, and March 31, 2021, were identified based on the following International Classification of Diseases, version 10 (ICD-10) codes: allergic conjunctivitis (H01), bacterial conjunctivitis (A543, A740, H100), viral conjunctivitis (B301, B303, B308, B309), parasitic conjunctivitis (H130, H131) and unspecified conjunctivitis (H102, H103, H104, H108, H109, H132, H138, P391). Patients of any sex and age who were treated through outpatient medical consultations were selected. Patients with a concomitant diagnosis of keratitis/corneal ulcer, blepharitis, stye, periorbital/orbital cellulitis, Sjögren’s syndrome, stenosis and other lacrimal pathway disorders were excluded. Based on the drug consumption information for the affiliated population that was systematically obtained by the dispensing company (Audifarma SA), a database was designed that allowed the following groups of patient variables to be collected:
-
1.
Sociodemographic: Age, sex, city of dispensation, type of affiliation with the Colombian Health System.
-
2.
Clinical: The type of conjunctivitis (unspecified, bacterial, viral or allergic) and comorbidities were identified from the ICD-10 codes.
-
3.
Pharmacological:
-
•
Ophthalmological medications: N-acetyl aspartyl glutamic acid, antibiotics (azithromycin, bacitracin, ciprofloxacin, gatifloxacin, moxifloxacin, neomycin, polymyxin b, sulfacetamide, tobramycin), antihistamines (alcaftadine, bepotastine, epinastine, ketotifen, olopatadine), nonsteroidal anti0inflammatory drugs (diclofenac, bromfenac, nepafenac), antivirals (acyclovir, ganciclovir), glucocorticoids (dexamethasone, fluorometholone, loteprednol, prednisolone), mast cell membrane stabilizers (sodium cromoglycate), immunosuppressants (cyclosporine, tacrolimus), ocular lubricants/artificial tears (polyacrylic acid, polyvinyl alcohol, polyvinyl carboxylic acid, sodium cromoglycate), polyvinyl alcohol, carboxymethylcellulose, sodium hyaluronate, chondroitin sulfate, hydroxypropyl methylcellulose, polyethylene glycol, propylene glycol, sympathomimetics (phenylephrine, naphazoline, tetryzoline).
-
•
Systemic drugs: Antibiotics (amoxicillin, ampicillin, azithromycin, cefadroxil, cephalexin, cephradine, ceftriaxone, ciprofloxacin, clarithromycin, clindamycin, dicloxacillin, doxycycline, erythromycin, norfloxacin) antihistamines (cetirizine, chlorpheniramine, desloratadine, diphenhydramine, fexofenadine, hydroxyzine, ketotifen, levocetirizine, loratadine), antiviral (acyclovir).
-
•
Type of prescriber: General practitioner, optometrist, ophthalmologist, other specialty (internal medicine, pediatrics, geriatrics, etc.).
-
•
The different pharmacological treatments were classified as appropriate or inappropriate according to the clinical practice guideline [8]. For example, it was considered inappropriate to use antibiotics in allergic conjunctivitis, or prescribing corticosteroids for bacterial conjunctivitis [8].
Additionally, the prevalence of conjunctivitis was calculated during the study period, as well as during the previous 12 months (including the time before the COVID-19 pandemic, which began in Colombia in March 2020).
The protocol was approved by the Bioethics Committee of the Universidad Tecnologica de Pereira in the category of research without risk (Endorsement code: 02-210,920). The ethical principles established by the Declaration of Helsinki were respected.
The data were analyzed with the statistical package SPSS Statistics, version 26.0 for Windows (IBM, USA). A descriptive analysis was performed using frequencies and proportions for qualitative-categorical variables. The normality of the continuous variables was evaluated using the Kolmogorov–Smirnov test, and continuous variables are reported as means and standard deviations and nonparametric variables are reported as medians and interquartile. The data are presented in the text and in tables.
Results
A total of 8708 patients with a diagnosis of conjunctivitis distributed in 140 different cities of Colombia were identified during the study period (April-2020 to March-2021), indicating an overall mean prevalence of conjunctivitis of 0.8 cases per 10,000 people. In the previous year (April-2019 to March-2020), a total of 63,040 cases of conjunctivitis were identified in the database, with a mean of 6.5 cases per 10,000 people. This represents a variation of − 86.2% with respect to the total number of cases (See Supplementary Figure).
From the 8708 patients included for analysis, the 59.3% (n = 5160) were women, and the median age was 44.7 years (interquartile range 22.4–65.3 years; range 0.1–102.8 years). A total of 21.6% (n = 1877) were younger than 18 years old, 23.4% (n = 2041) were between 18 and 39 years old, 32.4% (n = 2821) were between 40 and 64 years old, and 22.6% (n = 1969) were 65 years old or older. A total of 70.4% (n = 6130) of the patients lived in Bogotá (n = 1542; 17.7%), Cartagena (n = 857; 9.8%), Barranquilla (n = 724; 8, 3%), Popayán (n = 719; 8.3%), Montería (n = 650; 7.5%), Cali (n = 548; 6.3%), Sincelejo (n = 456; 5.2%), Armenia (n = 226; 2.6%), Manizales (n = 211; 2.4%) or Pereira (n = 197; 2.3%); 73.0% (n = 6356) were affiliated with the contributory regime, and 27.0% (n = 2352) were affiliated with the subsidized regime of the country’s health system.
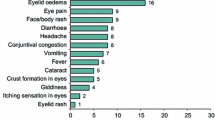
The most common etiology of conjunctivitis was unspecified (n = 4624; 53.1%), followed by allergic (n = 3259; 37.4%), bacterial (n = 636; 7.3%) and viral (n = 189; 2.2%). Most of the patients were attended by general practitioners (n = 7274; 83.5%). A total of 97.0% (n = 8444) of the patients received ophthalmic prescriptions, most commonly glucocorticoids (n = 3507; 40.3%), followed by antibiotics (n = 3284; 37.7%), antihistamines (n = 2764); 31.7%) and artificial tears (n = 1627; 18.7%). Systemic treatments for the management of conjunctivitis were prescribed in 14.3% (n = 1243) of cases and mainly comprised antihistamines (n = 997; 11.4%) and antibiotics (n = 293; 3.4. %). Table 1 shows the most commonly used ophthalmic and systemic medications for the management of patients with conjunctivitis.
A total of 489 different treatment regimens were found, and 51.6% (n = 4489) of the patients received one of the following treatments: olopatadine (n = 1737; 19.9%), dexamethasone + neomycin + polymyxin (n = 1453; 16.7%), carboxymethylcellulose (n = 481; 5.5%), fluorometholone (n = 477; 5.5%) and gentamicin (n = 341; 3.9%) (Table 2). Glucocorticoids associated with antibiotics were dispensed for 28.9% (n = 2519) of patients with conjunctivitis, while glucocorticoids without antibiotics were dispensed for 11.3% (n = 988), and antibiotics without glucocorticoids were used for 8.8% (n = 765) of patients.
As Table 2 shows, the proportion of women was higher for all types of conjunctivitis, and the median age among the groups was similar. Regarding the frequencies of prescriptions for various drug types, glucocorticoids and ophthalmic antibiotics predominated for both viral and bacterial conjunctivitis, while ophthalmic antihistamines were prescribed more frequently for allergic conjunctivitis, and artificial tears were prescribed most frequently for unspecified conjunctivitis. Systemic medications were used more often for viral and bacterial conjunctivitis (Table 2). Patients with viral conjunctivitis were the ones who had the highest proportion of inadequate pharmacological treatment (n = 166/189; 87.8%), followed by those who had bacterial conjunctivitis (n = 445/636; 70.0%) and allergic conjunctivitis (n = 922/3259; 28.3%). In patients with unspecified conjunctivitis, it was not possible to determine the adequacy.
Table 3 shows the prescription patterns for the drug groups according to the prescriber and type of conjunctivitis. Notably, the majority of the ophthalmic glucocorticoids prescriptions were issued by general practitioners and optometrists. Similarly, ophthalmic antibiotics and systemic medications were prescribed mainly by general practitioners; in contrast, most of the prescriptions issued by ophthalmologists were for antihistamines and artificial tears.
Discussion
This study allowed us to determine the prescription patterns of ophthalmic and systemic medications for the treatment of conjunctivitis in a group of patients affiliated with the Colombian Health System as evidence of drug use in the real world. These findings can be useful to help health care personnel; academics and scientists make decisions regarding the risks that their patients face and can contribute to strengthening the practices related to the rational use of antibiotics and glucocorticoids among physicians in an effort to reduce adverse drug reactions and ophthalmic complications in the country.
The prevalence of conjunctivitis varies according to the etiology and can be influenced by the patient’s age, sex, as well as by the seasons of the year [1, 11]. In this report, it was found that the general prevalence of conjunctivitis was affected by the COVID-19 pandemic, where a significant reduction in cases of conjunctivitis can be seen when comparing the pre-pandemic year with the first year of the pandemic, which is consistent with other studies [12, 13]. Thus, for example, Conde et al. [12] documented a 48.5% reduction in cases of viral conjunctivitis in a hospital institution in Spain, while in the USA, Lavista et al. [13] identified a 37.3% reduction in patients with non-allergic conjunctivitis. These changes may be due to social distancing, isolation, travel restrictions, closure of colleges and universities, less use of health services for conditions other than COVID-19, as well as a greater emphasis on hygiene and the use of personal protection elements [12, 13].
We observed that ophthalmic antibiotics were prescribed for more than one third of patients, including a large proportion of those with viral and unspecified conjunctivitis and a smaller proportion of patients with allergic conjunctivitis, for which clinical practice guidelines do not recommend the use of antibiotics [8, 9, 14]. However, the rate of antibiotics prescriptions for acute conjunctivitis is higher in countries such as the USA (58.0–72.7%) [6, 15], Australia (74.0%) [16], Holland (80.0%) [17] and Belgium (89.4%) [7] and lower in different Scandinavian countries (4.2–21.1%) [18]. The present analysis found that the majority of prescriptions were issued by general practitioners, which is consistent with the reports of other publications [6, 15,16,17]. For example, in England, Everitt et al.surveyed general practitioners and found that 95.0% prescribed antibiotics for the management of acute infectious conjunctivitis, but 58.0% of professionals believed that half of their patients had a viral infection [19]. The indiscriminate use of antibiotics can cause severe alterations in the ocular bacterial flora, which is essential for the prevention of ocular infections, and can be associated with an increase in antimicrobial resistance [10, 20].
Differences were found in the most frequently used type of antibiotic. In the present report, a quarter of the patients were prescribed neomycin with polymyxin B and glucocorticoid; this is in contrast with other reports, in which other antibiotics predominated [7, 15,16,17, 21,22,23,24]. For example, the use of polymyxin B with trimethoprim predominated in the USA (53.4%) [15], whereas it was prescribed with fusidic acid in the Netherlands (69.0%) [17], levofloxacin in China (71.8%) [21], chloramphenicol in Australia (50.8%) [16], moxifloxacin in India (52.0–53.5%) [23, 24] and tobramycin in Spain (66.1%) [22] and Belgium (23.4%) [7]. The differences in drug prescription patterns have been shown in other pharmacoepidemiological studies in the country, but in different clinical contexts [25,26,27]. These variations can be explained by the epidemiological heterogeneity among countries in terms of the etiology and resistance patterns of microorganisms, the characteristics of health systems, the accessibility and availability of drugs and the marketing strategies of the pharmaceutical industry [25, 26].
The inappropriate use of antibiotics for conjunctivitis with an etiology other than bacteria can have various causes. Professionals, especially general practitioners, may have difficulty distinguishing cases of viral and allergic conjunctivitis from bacterial cases because the three etiologies can present similar clinical characteristics, such as eye irritation, conjunctival injection and foreign body sensation [1, 4]. In addition, some prescribers may not have appropriate academic training for the correct diagnosis and treatment of acute conjunctivitis [28]. Similarly, the prescription of ophthalmic medications may be associated with sociodemographic characteristics of the patient, such as age, race, income, education level and comorbidities [6]. Additionally, patients may believe that antibiotics promotes faster recovery from the pathology and may therefore specifically seek such prescriptions from their doctor [18], and the unsubstantiated demand for these medications could lead to bias in the treating physician’s diagnostic and therapeutic process. Furthermore, the large number of prescriptions for systemic medications to treat conjunctivitis is noteworthy given that these drugs be reserved for adjuvant therapy for conjunctivitis derived from sexually transmitted infections [1]. Finally, the absence of updated guidelines for the management of patients with conjunctivitis could contribute to the incorrect diagnosis and inadequate treatment of this pathology [29].
Another relevant aspect of this report was the large proportion of patients who received ophthalmic glucocorticoids, which are not recommended for the management of most cases of infectious conjunctivitis [8, 14]. However, they can be used in short cycles for refractory cases of allergic and atopic conjunctivitis [8, 9]. It is striking that almost 30.0% of the patients received antibiotics, which is consistent with other studies, such as those reported by De Loof et al. [7] in Belgium (30.5%), and is higher than that reported by Shekhawat et al. [6] in a study of more than 340,000 American patients, 20.0% of whom concomitantly used glucocorticoids and antibiotics, and by Yu et al. [21] in China, where this association was present in 17.5% of cases. The use of ophthalmic glucocorticoids should be limited due to the risk of complications and adverse drug reactions, since they increase the latency period of adenoviruses, prolong the course of viral conjunctivitis, aggravate herpes simplex virus infections, increase intraocular pressure and increase the risk of glaucoma and cataracts [1, 8, 9, 30, 31] Therefore, due to the need for strict monitoring, these drug combinations should exclusively use by ophthalmologists and health personnel who have the necessary equipment to detect and prevent adverse eye reactions.
Some limitations in the interpretation of the results are recognized, since medical records were not accessed to verify the diagnosis of conjunctivitis or its etiology (allergic, infectious, other), severity and complications. Similarly, medications that the patients may have received that were prescribed outside the health system or were not delivered by the dispensing company were unknown. In addition, it is possible that some of the systemic prescriptions were used for pathologies other than conjunctivitis; however, these pathologies were not identified among the primary and secondary diagnoses listed in the database. However, the study included a significant number of patients who were distributed throughout most of the national territory and were covered by both the contributory and subsidized regimes of the country’s health system.
With these findings, we can conclude that different types of conjunctivitis are being managed without following the recommendations of clinical practice guidelines. The results highlight the extensive use of antibiotics with ophthalmic glucocorticoids, which in many cases can be considered potentially inappropriate prescriptions. It is suggested that those responsible for health care and training provide continuing education measures and develop clinical practice guidelines specifically aimed at first-line health personnel, such as general practitioners, to promote better diagnostic processes and the more careful selection of available medications to reduce the risk of adverse drug reactions and the rates of antimicrobial resistance.
Data availability
protocolos.io.
Code availability
dx.doi.org/10.17504/protocols.io.b4bxqspn
References
Azari AA, Barney NP (2014) Conjunctivitis: a systematic review of diagnosis and treatment. JAMA 311(1):95. https://doi.org/10.1001/jama.2013.280318
Azari AA, Arabi A (2020) Conjunctivitis: a Systematic Review. J Ophthalmic Vis Res 15(3):372–395. https://doi.org/10.18502/jovr.v15i3.7456
Segal KL, Lai EC, Starr CE (2014) Management of acute conjunctivitis. Curr Ophthalmol Rep 2(3):116–123
Yeu E, Hauswirth S (2020) A Review of the differential diagnosis of acute infectious conjunctivitis: implications for treatment and management. Clin Ophthalmol 14:805–813. https://doi.org/10.2147/OPTH.S236571
Chan VF, Yong AC, Azuara-Blanco A, Gordon I, Safi S, Lingham G, Evans J, Keel S (2021) A systematic review of clinical practice guidelines for infectious and non-infectious conjunctivitis. Ophthalmic Epidemiol. https://doi.org/10.1080/09286586.2021.1971262
Shekhawat NS, Shtein RM, Blachley TS, Stein JD (2017) Antibiotic prescription fills for acute conjunctivitis among enrollees in a large United States managed care network. Ophthalmology 124(8):1099–1107. https://doi.org/10.1016/j.ophtha.2017.04.034
De Loof H, De Win E, Moens N, Verhoeven V, Van Royen P, Kreps EO, Philips H (2021) Overprescribing of topical ocular corticosteroids and antibiotics in out-of-hours primary care in Belgium. Drug Healthc Patient saf 13:229–32. https://doi.org/10.2147/DHPS.S339141
Varu DM, Rhee MK, Akpek EK, Amescua G, Farid M, Garcia-Ferrer FJ, Lin A, Musch DC, Mah FS, Dunn SP (2019) American academy of ophthalmology preferred practice pattern cornea and external disease panel. Conjunctivitis preferred practice pattern®. Ophthalmology 126(1):P94–P169. https://doi.org/10.1016/j.ophtha.2018.10.020
Optometric clinical practice guideline: care of the patient with conjunctivitis, American optometric association. (2010) Accessed 24 Nov 2021. Available from: https://www.sdeyes.org/docs/CPG-11.pdf
Dave SB, Toma HS, Kim SJ (2013) Changes in ocular flora in eyes exposed to ophthalmic antibiotics. Ophthalmology 120(5):937–41. https://doi.org/10.1016/j.ophtha.2012.11.005
Ramirez DA, Porco TC, Lietman TM, Keenan JD (2017) Epidemiology of conjunctivitis in US emergency departments. JAMA ophthalmol 135(10):1119–21. https://doi.org/10.1001/jamaophthalmol.2017.3319
Conde Bachiller Y, Puente Gete B, Gil Ibáñez L, Esquivel Benito G, Asencio Duran M, Dabad Moreno JV (2022) COVID-19 pandemic: impact on the rate of viral conjunctivitis. Archivos de la Sociedad Espanola de Oftalmología 97(2):63–9. https://doi.org/10.1016/j.oftal.2021.03.002
Lavista Ferres JM, Meirick T, Lomazow W, Lee CS, Lee AY, Lee MD (2022) Association of public health measures during the COVID-19 pandemic with the incidence of infectious conjunctivitis. JAMA ophthalmol 140(1):43–9. https://doi.org/10.1001/jamaophthalmol.2021.4852
National institute for health and care excellence. Conjunctivitis-infective. 2021. Accessed 24 Nov 2021. Available from https://cks.nice.org.uk/topics/conjunctivitis-infective/
Frost HM, Sebastian T, Durfee J, Jenkins TC (2021) Ophthalmic antibiotic use for acute infectious conjunctivitis in children. J AAPOS 25(6):350.e1-350.e7. https://doi.org/10.1016/j.jaapos.2021.06.006
Cherry MD, Tapley A, Quain D, Holliday EG, Ball J, Davey A, van Driel ML, Fielding A, Spike N, FitzGerald K, Magin P (2021) Antibiotic prescribing patterns of general practice registrars for infective conjunctivitis: a cross-sectional analysis. J Prim Health Care 13(1):5–14. https://doi.org/10.1071/HC20040
Rietveld RP, ter Riet G, Bindels PJ, Schellevis FG, van Weert HC (2007) Do general practitioners adhere to the guideline on infectious conjunctivitis? Results of the second Dutch national survey of general practice. BMC Fam Pract 8:54. https://doi.org/10.1186/1471-2296-8-54
Andersson J, Hofsli M, Gade UL, Heegaard S, Pottegård A (2018) Use of topical ocular antibiotics in young children: a Scandinavian drug utilization study. Acta Ophthalmol 96(8):789–794. https://doi.org/10.1111/aos.13813
Everitt H, Little P (2002) How do GPs diagnose and manage acute infective conjunctivitis? A GP survey. Fam Pract 19(6):658–60. https://doi.org/10.1093/fampra/19.6.658
Al-Khalaileh W, Abu-Farha R, Wazaify M, Van Hout MC (2019) Ophthalmic drug abuse: an observational study from community pharmacies. Res Social Adm Pharm 15(8):943–948. https://doi.org/10.1016/j.sapharm.2019.01.016
Yu Z, Zhu J, Jin J, Yu L, Han G (2021) Trends in outpatient prescribing patterns for ocular topical anti-infectives in six major areas of China, 2013–2019. Antibiotics (Basel) 10(8):916. https://doi.org/10.3390/antibiotics10080916
Gutiérrez-Abejón E, Herrera-Gómez F, Ayestarán-Martínez IJ, Álvarez FJ (2020) Trend in the use of topical ocular anti-infectives in a region of Spain between 2015 and 2019: a population-based registry study. Rev Esp Quimioter 33(6):453–458. https://doi.org/10.37201/req/096.2020
Kauser H, Chopra D, Mukherjee S, Mohan P (2018) Pharmacoepidemiological observational study of antimicrobial use in outpatients of ophthalmology department in north Indian population. J Pharm Bioallied Sci 10(2):72–76. https://doi.org/10.4103/JPBS.JPBS_255_17
Supritha N, Mohapatra S, Rani RJ (2016) Prescription pattern of antibiotics and susceptibility of the pathogens in infectious conjunctivitis. Biomed Pharmacol J 9(2):599–604
Machado-Alba JE, Valladales-Restrepo LF, Gaviria-Mendoza A, Machado-Duque ME, Figueras A (2020) Patterns of antibiotic prescription in Colombia: are there differences between capital cities and municipalities? Antibiotics (Basel) 9(7):389. https://doi.org/10.3390/antibiotics9070389
Valladales-Restrepo LF, Constain-Mosquera CA, Álvarez-Amaya V, Machado-Alba JE (2021) Study of prescription-indication of tetracyclines in a population in Colombia. Fundam Clin Pharmacol Epub ahead of print. https://doi.org/10.1111/fcp.12724.
Valladales-Restrepo LF, Peña-Verjan NM, Vargas-Díaz K, Machado-Alba JE (2021) Potentially inappropriate prescriptions of antipsychotic and anticholinergic drugs in patients with Parkinson’s disease. Neurodegener Dis Manag 11(5):361–371. https://doi.org/10.2217/nmt-2021-0021
Suman RK, Gore VS, Mohanty IR, Israni NA, Deshmukh YA (2015) Prescribing patterns of drugs used for treatment of conjunctivitis in ophthalmology outpatient department of tertiary care hospital. Int J Health Sci Res 5:194–199
Giovanni Castaño M. Guía para manejo de urgencias tomo II Bogotá: Imprenta Nacional de Colombia. 2009: 370–7. Accessed 24 Nov 2021. Available from http://www.med-informatica.net/TERAPEUTICA-STAR/UrgenciasGuiaMPS2009_2_DocNewsNo19038DocumentNo10950.pdf
Holland EJ, Fingeret M, Mah FS (2019) Use of topical steroids in conjunctivitis: a review of the evidence. Cornea 38(8):1062–1067. https://doi.org/10.1097/ICO.0000000000001982
Sen P, Jain S, Mohan A, Shah C, Sen A, Jain E (2019) Pattern of steroid misuse in vernal keratoconjunctivitis resulting in steroid induced glaucoma and visual disability in Indian rural population: an important public health problem in pediatric age group. Indian J Ophthalmol 67(10):1650–1655. https://doi.org/10.4103/ijo.IJO_2143_18
Acknowledgements
To Soffy Claritza López for her work in obtaining the database. To Brahyan Osorio Velásquez and Jairo Daniel Corzo Romero for their collaboration in preparing the draft.
Funding
This work received no funding.
Author information
Authors and Affiliations
Contributions
LFVR participated in the drafting, data collection, data analysis, description of results and discussion. MEMD participated in the drafting, data collection, data analysis, description of results and discussion. AGM participated in the drafting, description of results, and discussion of the article. DFLC participated in the drafting, description of results. JAOC participated in the drafting, description of results. MCOG participated in the drafting, description of results. DFMP participated in the drafting, description of results, and discussion of the article. JEMA participated in the drafting, data analysis, description of results, discussion, critical revision of the article, and evaluation of the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
The protocol was approved by the Bioethics Committee of the Universidad Tecnológica de Pereira (Technological University of Pereira) in the category of “risk-free research” (approval number 02-210920). The principles established by the Declaration of Helsinki were respected.
Consent to participate
Not applicable as it is a retrospective observational study.
Consent to publication
All authors consent to participate.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
About this article
Cite this article
Valladales-Restrepo, L.F., Machado-Duque, M.E., Gaviria-Mendoza, A. et al. Indication-prescription study for the management of conjunctivitis in a Colombian population. Int Ophthalmol 43, 83–93 (2023). https://doi.org/10.1007/s10792-022-02390-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-022-02390-7