Abstract
Purpose
To introduce a modified procedure of ICL implantation, to summarize the perioperative problems and their corresponding treatment after myopia correction with Implantable Collamer Lens (ICL), and to compare the difference of complications between the no-hole ICL and hole ICL.
Methods
We searched all articles on ICL-related perioperative problems and their corresponding treatment in Scopus, Embase, PubMed and Web of Science databases for the last 22 years.
Results
ICL implantation is safe, effective, stable and predictable in the correction of myopia, hyperopia and astigmatism, but can also cause a series of perioperative problems, including intraoperative and postoperative complications.
Conclusion
There are many kinds of complications related to ICL, but the common intraoperative and postoperative complications mainly include abnormality of arch height, abnormal position of ICL, loss of corneal endothelial cells and corneal decompensation, high intraocular pressure and secondary glaucoma, cataract and night vision symptoms. Compared with ICL without central pore, the incidence of complications such as loss of corneal endothelial cells and corneal decompensation, high intraocular pressure and secondary glaucoma and cataract was relatively lower in central hole ICL, while postoperative complications such as night vision symptoms were obvious.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction of ICL process
The brief procedures of surgery we recommend are as follows: After topical anesthesia, a 2.7 mm or 3 mm superior clear corneal main incision is created. The anterior chamber was filled with viscoelastic agent. The ICL was inserted through the main incision with the use of an injector cartridge (STAAR Surgical, Switzerland) and was placed in the posterior chamber by gently tucking the footplates beneath the iris. The viscoelastic agent was suctioned out of the anterior chamber with irrigation/aspiration (IA) surgery handpiece. No preoperative or intraoperative peripheral iridectomy was performed in any case. After surgery, the patient's intraocular pressure was monitored for 2–4 h, and topical anti-inflammatory and infection prevention regimens were prescribed. Different surgeons and different hospitals have different topical anti-inflammatory and infection prevention regimens. In our hospital, it included 0.3% Tobramycin and 0.1% Dexamethasone ophthalmic suspension (Tobramycin and Dexamethasone Eye Drops, s.a. ALCON-COUVREUR n.v.; four times per day and cut back once a week for 4 weeks), Bromfenac Sodium Hydrate Ophthalmic Solution (Senju Pharmaceutical Co., Ltd., Japan; two times per day for 4 weeks).
The traditional incision is in the temporal side of the cornea, but we recommend a superior incision, because the vertically fixated ICL through a superior incision achieved good results without significant complications. Considering that younger patients requiring ICL surgery tend to have with-the-rule astigmatism, this surgical technique may be a viable option for reducing astigmatism without using toric ICL (TICL) [1]. The normal process is that viscoelastic agent will be first injected into the anterior chamber followed by ICL implantation. However, it was reported that reversing the order of the two had no effects on the corneal endothelial cell count. Additionally, the implantation of an intraocular lens prior to injecting OVDs reduces the operation time and lowers the rate of IOP rise in the early postoperative period, making it safe and effective for ICL implantation [2]. Therefore, we recommend the modified surgical procedure.
Summary and treatment of intraoperative complications of ICL
Operation injury
Surgical injury can lead to conjunctival or intraocular hemorrhage, corneal epithelial defects, corneal edema, descemet membrane detachment of the cornea, anterior chamber angle injury, and traumatic cataract, so the surgeon's learning curve is considered to be a risk factor for postoperative cataract formation. Traumatic cataract is the most serious consequence of surgical injury. For non-central hole ICL implantation, when performing intraoperative peripheral iridectomy (PI), iris and anterior lens capsule may be drawn to anterior vitrectomy cutter which result in large PI and injury to anterior lens capsule [3]. Both Steinwender G [4] and Chung JK [5] agreed that anterior subcapsular cataract was induced during implantation of a ICL with a central hole by cannula irrigation with enforced stream onto the capsule through that hole. This problem can be solved by modified surgical methods, such as the use of IA surgery handpiece.
Meibomian gland dysfunction and dry eye
ICL surgery may lead to changes in the microenvironment of the eye surface, resulting in meibomian gland dysfunction, or even dry eyes. It was reported by Moshirfar M et al. [6] that dry eye symptoms occurred in 13% of patients on the first day after surgery and peaked at about 29% at 3 months. According to the study of Paul J Dougherty et al., 5.8% of patients undergoing V4 ICL implantation had dry eye after surgery, mainly mild to moderate dry eye, without severe symptom [7]. It was reported that OSDI scores increased, while NIBUT decreased significantly at 1 month after ICL implantation, which restored slowly and did not return to the original level at 3 months after surgeries. Moreover, lid marginal abnormality and Meibomian gland secretion were significantly higher at 1 month postoperatively and returned near the baselines gradually at 3 months postoperatively. In addition, patients who had dry eye symptoms before surgery had significantly worse symptoms after surgery [8, 9]. In another report, the stability of tear film decreased and caused dry eye symptoms of varying degrees in patients in the early stage after ICL surgery, but there was no significant impact on the amount of basic tear secretion. Three months after surgery, the subjective dry eye discomfort symptoms and eye surface tear film stability of patients basically recovered to the preoperative level. However, for patients with high postoperative corneal staining score or OSDI questionnaire score, drugs or artificial tears should be given in time to help repair of corneal epithelium [10].
Astigmatism
There were few reports about surgical astigmatism of ICL surgery. Kamiya, K. et al. reported that astigmatism caused by ICL surgery with horizontal 3.0 mm transparent corneal incision is 0.45D measured by keratometer and 0.49D by corneal topography. Moreover, its regular astigmatism and will not recover over time [11, 12]. However, it was reported that the magnitude of corneal astigmatism significantly increased in the temporal incision group, but it significantly decreased postoperatively in the superior incision group [13].
Urrets-zavalia syndrome
ICL-related UZS may be caused by the increase in intraocular pressure postoperative due to viscoelastic agent retention. This condition leads to anterior chamber angle obstruction, potentially promoting ischemia of the root of the iris, resulting in permanent and relative paralysis of the ciliary muscle.
To our knowledge, Kummelil et al. were the first to report an association between UZS and ICL implantation (Poster P85, American Society of Cataract and Refractive Surgery, May 25–29, 2011, San Diego).
In 2015, Al Habash A et al. [14] described the case of a healthy 28-year-old woman who underwent ICL implantation in both eyes for correction of bilateral high myopia with astigmatism, but UZS occurred only in the patient's left eye. On the first postoperative day, the patient developed increased intraocular pressure (IOP) and a fixed, mid-dilated pupil in her left eye. The elevated IOP was corrected within 3 days by medical treatment. However, the pupil remained mid-dilated and nonreactive to both light and accommodative effort during 2 months of follow-up; there was no reaction to pilocarpine (0.125% or 4%) eyedrops.
A similar case was reported by Srirampur et al. [15], who underwent bilateral ICL implantation but developed UZS in only one eye. Because the patient was implanted with a non-toric ICL, rotation of ICL was performed to reduce the high vaulting and optic capture along with single-pass four throw pupilloplasty, and received a successful outcome.
Iris and ciliary cysts
Gharaibeh et al. reported a 27-year-old patient who developed iris and ciliary cysts after ICL implantation. They suggested that the iris and ciliary cysts originated from corneal or conjunctival epithelial cells that either happened to implant onto the iris during surgery or migrated to the iris via the surgical wound postoperatively [16].
If the cyst is small and asymptomatic, only close follow-up is required, but continued cyst growth may lead to potentially vision-threatening complications such as displacement of ICL.
Lacquer crack and choroidal neovascularization
Lacquer cracking and choroidal neovascularization are rare complications after ICL implantation, and only a few literatures have been reported [17, 18]. The main pathogenesis is that the posterior sclera of patients with high myopia is thin. ICL implantation leads to intraocular biomechanical abnormalities, which is more likely to cause the rupture of posterior Bruchs membrane and atrophy of the retinal pigment epithelium, resulting in lacquer cracks.
Retinal hiatus and rhegmatogenous retinal detachment
Retinal hole is one of the complications of ICL implantation. In the process of ICL implantation, acute posterior vitreous detachment can be caused by sudden decompression of the anterior chamber due to the initial establishment of surgical channel or the operator's operation. For young patients with high myopia, the vitreous body and the retina are attached relatively closely, and the acute posterior vitreous detachment can easily pull the retina, resulting in retinal hiatus [19, 20]. Moreover, the crack region generated by ICL implantation would appear in new sites, independent of the patient's existing fissure lesions [21]. If the hiatus appeared within a short period of time after operation and accompanied by internal limiting membrane defect around the hiatus, the prognosis was very poor. If occult progression occurs, surgical treatment results in better best corrected visual acuity [22,23,24].
Vitreous liquefaction was obvious in patients with high myopia, and the formation of retinal hiatus was more likely to develop into rhegmatogenous retinal detachment. A retrospective study by Martinez-Castillo et al. showed that the incidence of rhegmatogenous retinal detachment after ICL implantation was 2.07%, which occurred on average 29.12 months after surgery, and 68.75% of retinal detachment cases had only one ruptured hole [25]. Rhegmatogenous retinal detachment may occur several hours after ICL or may progress slowly for several months. Most patients can recover good visual quality after treatment, but some patients still cannot recover their visual quality even after therapy [26,27,28,29,30,31]. However, it was also reported that V4c ICL implantation for high myopia correction does not add RRD risk in the long term [32].
Endophthalmitis
Endophthalmitis after ICL implantation includes infectious endophthalmitis and aseptic endophthalmitis, with an incidence of about 0.0167% [33].
Infectious endophthalmitis is one of the most serious complications after ICL surgery. Reported pathogenic bacteria include staphylococcus epidermidis, radioactive rhizobia, aspergillus, pseudomonas aeruginosa, cutibacterium acnes, etc. [34,35,36,37,38,39]. Report of aseptic endophthalmitis after ICL implantation includes Toxic anterior segment syndrome (TASS) and acute aseptic anterior uveitis [40]. TASS is the main cause of aseptic endophthalmitis after ICL implantation, which is induced by the material of pollution of intraocular lavage fluid, talc powder of gloves and so on [41,42,43,44,45].
Summary and treatment of postoperative complications of ICL
Night vision symptoms
58% of the patients reported a worsening in night vision symptoms (mostly nonspecific glare and halo or starburst) after surgery, but overall levels of satisfaction were high [46, 47]. The incidence of halo after ICL implantation was 68.8%, and that of starburst was 43.8% [48]. Glare/halo was present in 39% of eyes at 1 month, 32% at 3 months, 24% at 6 months, and improved to 15% of eyes at 12 months. The size of the halo will not change with the luminance levels after ICL implantation, but the incidence will decrease with postoperative time. Halo in about 15.2% of patients and glare in 23.2% postoperatively in the study of Mahfouth A et al. [49], while Dong Hui Lim et al. reported that the incidence of halo and glare was 34% and 26%, respectively. The mismatches of pupil diameter, white to white (WTW) and ICL optical region diameter were positively correlated with halo occurrence, and the high curvature of ICL is one of the significant risk factors for postoperative glare [50]. In addition, postoperative glare occurred in a small number of patients because of laser iridotomy [51].
Abnormality of arch height
Arch height was positively correlated with anterior chamber depth, pupil diameter, axial length and lens position and negatively correlated with lens thickness [52,53,54]. At 1 month after surgery, ICL size had the greatest impact on the arch height, followed by horizontal sulcus-to-sulcus diameter (STS), crystalline lens thickness (LT), and vertical STS. The influence of other factors such as white-to-white diameter (WTW) and preoperative spherical equivalent refractive error had no effect [55,56,57,58]. Although WTW can indirectly predict STS, the WTW diameter was further away from 11.08 to 12.51 mm, or the ACD was further away from 2.81 to 3.74 mm, the correlation between the STS and WTW diameters was weaker [59].
The causes of postoperative high arch height include the too large ICL relative to the ciliary sulcus, the younger age of the patients, and the higher myopia [60, 61]. Too large intraocular lens relative to the ciliary sulcus is the main influencing factor of high arch height. High crystalline lens rise, and low ICL spherical equivalent were the major risk factors in eyes presenting low arch height [62]. Moreover, arch height also decreased with time and decreased the most from one month to three months after operation [63,64,65,66,67,68,69,70,71,72,73,74,75,76]. But it is also been reported in the literature that the average postoperative arch height will decrease significantly at 6 months after surgery and will remain basically stable thereafter [6]. Schmidinger reported that the arch height was reduced by an average of 28 μm per year [77], while Choi, JH's study showed that the value was 21 μm [78]. Different surgeons have different perceptions of the range of safe arch height, but existing reports suggested that the minimum safe arch height is from 52 to 260 μm [79,80,81,82].
In view of the decrease in arch height over time [83], in order to maintain sufficient arch height for a long time (> 10 years), the immediate arch height after operation should be greater than 550 µm [84], and for arch height below 150 µm, immediate removal and/or replacement with a more appropriate ICL should be considered [85]. Additionally, vertical rotation of an ICL may be a less invasive method to treat high arch height in certain cases [86].
With the advent of the microscope-integrated optical coherence tomography (OCT), intraoperative determination of ICL vault using OCT is an effective method for predicting postoperative ICL vault and minimizing postoperative abnormality of arch height that could require surgical retouching [87].
Abnormal position of ICL
Postoperative position abnormalities include ICL dislocation, ICL rotation and ICL inversion.
ICL dislocation includes subluxation and total dislocation, and the causes involve Improper arch height, residual of viscoelastic agent, and relatively inappropriate size of ICL [88, 89]. There are also some rare predisposing factors, such as the use of specific drugs and trauma. Rui Wang et al. reported a case of postoperative ICL dislocation associated with olanzapine and buspirone. These two drugs both have anticholinergic effects and can cause pupil dilation and ciliary paralysis, which is speculated to make ICL dislocate into the anterior chamber in conjunction with other factors such as face-down ducking and dim-light induced pupil dilation. This case suggests that systemic anticholinergic agents may be a relative contraindication to ICL implantation [90]. Up to now, fourteen cases of trauma-related ICL dislocation had been reported, of which thirteen cases occurred after ocular contusion. Another case was caused by sudden occipital trauma. All of them received ICL repositioning surgery, but postoperative visual acuity recovery varied. Therefore, it is important to educate patients to use protective eyewear during activities with a risk of ocular contusion [91, 92].
Spontaneous rotation is a common postoperative complication. For patients with ICL implantation, spontaneous rotation only affected the arch height of patients to a certain extent, and for patients with TICL, it resulted in a significant loss of visual acuity [93, 94]. The incidence of spontaneous rotation of TICL was about 0.12% [86]. Majid Moshirfar et al. 's study showed that 87% of patients rotated < 5° after TICL implantation and did not require additional intervention [6]. However, it was also reported that approximately 9.375% of patients had a cylinder axis rotation of 10° or greater occurred and required repositioning [95].
Most of the turn-over of ICL occurred during surgery, with an incidence of about 1.8%, and were mostly related to factors such as lens preinstallation, surgical incision, injection process, and anterior chamber depth. Spontaneous turnover after ICL implantation is extremely rare, and only two cases have been reported, and the longest one occurred five years after surgery [96, 97].
Loss of corneal endothelial cells and corneal decompensation
Direct contact between ICL and corneal endothelial cells and postoperative corneal remodeling are the main causes of corneal endothelial cell loss [98]. Further loss may result in corneal decompensation [99].
It is reported that the lowest rate of endothelial cell loss after non-central hole ICL was 1.1% and the highest was 13.4% within 5 years [100, 101]. Beyond five years after operation, the lowest rate was 4.7% and the highest was 19.75% [102,103,104,105,106]. The lowest rate of endothelial cell loss within five years after ICL with a central hole (V4c ICL) is 0.41%, and the highest is 22.0%, and arch height was the most significant factor for changes in corneal endothelium cell density in V4c ICL [57, 66, 69,70,71, 73, 75, 76, 107,108,109,110,111,112,113,114,115,116].
V4c ICL implantation may have advantages over conventional ICL implantation only in terms of the density in the superior regions, possibly because preoperative laser iridotomies are unnecessary [108]. In addition, the use of viscoelastic agent for V4cICL implantation can effectively protect corneal endothelial cells [117]. However, newer studies had shown that the OVD-free method is safe and efficient for ICL implantation. It can be a safer method of ICL implantation without additional damage to the corneal endothelial cells compared to the standard method and it completely eliminates ophthalmic viscoelastic devices-related complications without causing additional complications [118,119,120,121,122,123,124].
Decreased anterior chamber angle (ACA)/trabecular iris angle (TIA) and anterior chamber depth (ACD)
It was reported that peripheral ACD and ACA after ICL/TICL(V4c) implantation were significantly lower than pre-operative values. The ACD and ACA was significantly narrowed immediately after V4c ICL implantation and the decrease tended to be stable after one month [21, 76, 83]. Variations of peripheral ACD and ACA were greater in eyes after TICL (V4c) implantation compared with identically sized ICL (V4c) implantation and with larger size than smaller size lens implantation [125].
Within one month after ICL implantation, both trabecular iris angle (TIA) and anterior chamber depth (ACD) decreased compared with that before surgery. TIA was reduced by about 7.4–45% postoperatively [105, 126,127,128,129,130,131,132,133], ACD decreased by about 2.4–35% compared with the preoperative level [42, 127, 128, 134, 135].
High intraocular pressure and secondary glaucoma
High intraocular pressure and secondary glaucoma account for 4.4% of postoperative complications after ICL implantation [136], and the causes include steroid response, viscoelastic agent residue, aqueous misdirection, pupillary block, Iris pigmentation, narrow ACA, etc. [137,138,139]. The increase in IOP mostly reached its peak at the end of the first postoperative month, and the vast majority of patients can resume normal IOP [137]. Currently, the reported secondary glaucoma after ICL implantation can occur at most 8 years after surgery [68].
Steroid response is one of the most common causes of postoperative high intraocular pressure, accounting for about 64% [136, 138], mainly occurring 1 to 4 weeks after surgery and generally requiring no treatment [140].
High intraocular pressure caused by viscoelastic agent residue can be observed for 24 h. If the patient's intraocular pressure continues to rise and exceeds 35 mmHg, or the symptoms such as nausea and vomiting, swelling pain of the affected eye and headache remain unrelieved, another operation can be considered to remove viscoelastic agent [141].
The incidence of secondary glaucoma caused by postoperative dispersion of pigment, pupillary block and other reasons is between 0 and 5%, and the onset time is variable [100, 142, 143].
The most common complication of late postoperative secondary glaucoma is Pigmentary Glaucoma Syndrome [144, 145]. The ICL implantation can cause pigment deposition in trabecular meshwork and high IOP in the short term [126, 136, 140].
Pupillary block occurs mostly after implantation of ICL without central hole. At present, the central hole ICL can reduce the incidence of pupillary block, eliminates the need for laser peripheral iridectomy preoperatively and obtains satisfactory IOP after surgery [146,147,148,149,150,151]. In particular, Gonzalez-Lopez [152], Mansoori T [153], Isha G [154] and Frost A et al. [155] had all reported pupillary block glaucoma secondary to central hole obstruction after ICL implantation, which may be related to viscoelastic residue, iris pigmentation, increase in inflammatory factors in aqueous humor and so on. The longest occurrence was 5 years after ICL implantation.
The cause of malignant glaucoma after ICL implantation may be that ICL is too small, which leads to hyperemia of the ciliary body and damage of the suspensory ligament, resulting in relatively poor forward flow of aqueous humor, forcing aqueous humor to flow backward into the vitreous cavity, forming a vicious circle. Moreover, it may also be that viscoelastic agent entered the posterior chamber, resulting in obstruction. Kodjikian et al. [156]. reported that a 23-year-old woman received an ICM 130 V2 myopic phakic intraocular lens (IOL) (Staar Surgical AG) implantation. Three days later, the patient developed malignant glaucoma without pupillary block or choroidal hemorrhage/effusion. As maximum medical treatment failed, rapid secondary surgery was performed with sclerotomy, aspiration in the midvitreous cavity, and removal of the IOL. Almalki S et al. had also reported malignant glaucoma due to aqueous misdirection [137]. Senthil S et al. [138] also reported the occurrence of malignant glaucoma in one eye after ICL implantation, which received the treatment of pars plana vitrectomy and hyaloidotomy. Chanbour WA et al. [157] reported that a V4cICL was placed in the eye of a 31-year-old male patient with high myopia followed by the development of malignant glaucoma. After failing medical treatment for 5 days, a noncomplicated pars plana vitrectomy and anterior hyaloidectomy succeeded in breaking the aqueous misdirection. Furthermore, they suggest that intraoperative miotics may increase the risk of malignant glaucoma after surgery.
Decreased ACA after surgery may cause high intraocular pressure and secondary glaucoma. Ex-PRESS glaucoma filtration surgery might be a safe and effective alternative treatment for intractable glaucoma caused by narrow ACA after ICL implantation [158].
Occlusion of laser iridotomy
YAG laser iridotomy is required to balance IOP 1 to 2 weeks before implantation of ICL without central hole, which is prone to cause recurrent occlusion of laser iridotomy after surgery, possibly due to surgical trauma or reactivation of static anterior uveitis [159].
Traumatic prolapse of iris
Jordan W et al. reported the first case of traumatic prolapse of iris after ICL implantation, which may be caused by ocular contusion and high intraocular pressure caused by strong external forces. The sudden increase in intraocular pressure will split the transparent corneal incision that has healed after ICL implantation, and then, the iris will be expelled from the eye [160]. Packer KT et al. had a similar report [114].
Cataract
Cataract is one of the common complications after ICL implantation [161], and early cataract after ICL implantation is mostly related to surgical trauma, while late cataract is mostly related to contact between ICL and the lens itself [162]. The incidence increases with the passage of postoperative time [68, 74, 77, 84, 142, 163,164,165,166,167,168,169]. It has been reported that the incidence of cataract within 10 years after ICL implantation is 12.1% [78] and the risk of cataract formation will increase seven years after ICL implantation [114]. Ohoud Owaidhah et al. also reported a case of bilateral cataract 4 months after ICL implantation for both eyes [170], while the longest reported cataract caused by ICL implantation is 10 years after surgery.
Low arch height is considered to be one of the most important factors in increasing the risk of ICL-associated cataract development [171]. Other factors that increase the risk of ICL-associated cataract include contact between ICL and the lens itself, abnormal aqueous humor circulation on the lens surface after surgery, age greater than 40–45 years old, preoperative diopter greater than -12D to -14D and preexisting lens opacity [53, 80, 82, 84, 172,173,174]. Miguel J Maldonado et al. reported that the use of miotics after ICL implantation can also cause cataracts, possibly because the lens moves forward while the ICL moves backward during eye adjustment, resulting in rapid contact between them [175, 176]. This does not occur in all patients, but caution is advised against cholinergic agonists in patients with ICL implantation.
The most common type of ICL-associated cataract is anterior subcapsular cataract (ACS). The incidence ranged from 0.3% to 28%, with an average onset time of 3.4 ± 1.9 years after ICL implantation. ACS has a significant positive correlation with age and a significant negative correlation with anterior chamber depth (ACD) [95, 100, 116, 136, 145, 165, 177,178,179].
Femtosecond laser-assisted cataract surgery (FLACS) combined with ICL extraction has been shown to be a feasible method for patients developing cataracts after the ICL implantation [180,181,182,183]. We can also proceed for ICL explanation with cataract surgery and IOL insertion of the affected eye [184].
Ciliary body detachment and secondary choroidal detachment
Franciscol et al. reported a case of ciliary body detachment and secondary 360-degree choroidal detachment after ICL implantation. After exclusion of other possibilities, it was considered to be caused by preoperative YAG laser iridotomy. The patient received surgical treatment and recovered well [185].
Suprachoroidal effusion
According to Victoria de Rojas et al., a young man developed suprachoroidal effusion after ICL implantation, possibly related to the postoperative use of acetazolamide, an IOP lowering medication [186].
Macular edema and macular hole
Julide Canan et al. reported a 33-year-old male patient who developed cystoid macular edema after ICL implantation [187]. Possible mechanisms include continuous friction between ICL and posterior iris surface or ciliary sulcus, posterior vitreous detachment caused by ICL implantation, retinal traction, and surgical reduction after primary surgery. CME after ICL is usually self-limited. For patients with severe conditions, intravitreal injection of NSAID drugs can subside CME, but it is not recommended to use it to prevent CME after ICL implantation.
In the report of Kumar et al. [188], a 28-year-old male was found to have a full-thickness macular hole in his right eye 4 months after bilateral ICL implantation without obvious retinal or vitreous changes, preoperatively. The patient received a treatment of pars plana vitrectomy with inverted internal limiting membrane flap and gained well visual acuity (20/40) with the closure of the hole.
Microvascular anomalies in myopic retinoschisis
Zhang X et al. [189] reported a case that retinoschisis with supranasal microvascular anomalies of the left eye was found during routine reexamination one year after ICL implantation. The patient had no complaints. The naked eye visual acuity of the left eye was 1.0. This case suggests that the fundus of patients with high myopia without complaint should also be examined in detail and comprehensively. In addition to paying attention to peripheral retinopathy, the posterior pole and middle peripheral retina should be carefully examined, especially the areas that cannot be covered by conventional OCT.
Thickening of the retinal nerve fiber layer
According to the research of Zhu QJ et al., central retinal thickness (CRT) was significantly higher at one and three months postoperative (all P < 0.01). Ganglion cell-inner plexiform layer thickness (GCT) was significantly higher at 1wk, 1, and 3 month postoperative (all P < 0.01) [190]. The thickness of the retinal nerve fiber layer (RNFL) increased significantly after surgery, especially in the upper and lower quadrants of the retina, and the thickness of RNFL was not related to the change of the equivalent spherical equivalent refraction before and after surgery or the diopter of the intraocular lens[191].
Transient reduction in the retinal microvascular network
A statistically significant reduction in microvascular density in the retina and the superficial plexus was found 1 week and 1 month after ICL implantation. However, the microvascular density recovered toward the baseline level 3 months postoperatively [192]. Therefore, patients with pre-existing retinal vascular-related problems should carefully consider whether to perform this operation.
Conclusion
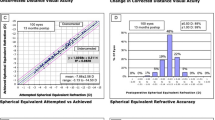
There are many kinds of complications related to ICL, but the common intraoperative and postoperative complications mainly include abnormality of arch height, abnormal position of ICL, loss of corneal endothelial cells and corneal decompensation, high intraocular pressure and secondary glaucoma, cataract and night vision symptoms. Compared with ICL without central pore, the incidence of complications such as loss of corneal endothelial cells and corneal decompensation, high intraocular pressure and secondary glaucoma and cataract was relatively lower in central hole ICL, while postoperative complications such as night vision symptoms were obvious. The corresponding proportions are shown in Fig. 1.
Out look
At present, Evo + ICL implantation is being initially carried out in China. Compared with V4c ICL, Evo + ICL expands the optical area and further provides better guarantee for the improvement of night vision and vision quality of patients [193]. However, Evo + ICL does not solve the problems of spontaneous rotation of ICL, inappropriate arch height and so on. It is hoped that better type of ICL will be designed in the future to solve these problems.
References
Kamiya K, Ando W, Hayakawa H, Gotoda S, Shoji N (2022) Vertically fixated posterior chamber phakic intraocular lens implantation through a superior corneal incision. Ophthalmol Ther 11(2):701–10. https://doi.org/10.1007/s40123-022-00470-6
Liu H, Dong D, Chen C, Ye J (2021) A comparative study of two types of implantation surgery methods for implantable collamer lenses. J Ophthalmol 2021:4074773. https://doi.org/10.1155/2021/4074773
Alshabeeb RS, Alharbi SS (2019) Vitrector induced lens injury during peripheral iridectomy in implantable collamer lens surgery. Saudi J Ophthalmol 33(4):389–91. https://doi.org/10.1016/j.sjopt.2018.10.006
Steinwender G, Varna-Tigka K, Shajari M, Kohnen T (2017) Anterior subcapsular cataract caused by forceful irrigation during implantation of a posterior chamber phakic intraocular lens with a central hole. J Cataract Refract Surg 43(7):969–74. https://doi.org/10.1016/j.jcrs.2017.03.045
Chung JK, Shin JH, Lee SJ (2013) Transient anterior subcapsular vacuolar change of the crystalline lens in patients after posterior chamber phakic intraocular lens implantation. BMC Ophthalmol. https://doi.org/10.1186/1471-2415-13-61
Moshirfar M, Bundogji N, Tukan AN et al (2021) Toric implantable collamer lens for the treatment of myopic astigmatism. Clin Ophthalmol 15:2893–906. https://doi.org/10.2147/opth.S321095
Dougherty PJ, Priver T (2017) Refractive outcomes and safety of the implantable collamer lens in young low-to-moderate myopes. Clin Ophthalmol 11:273–7. https://doi.org/10.2147/opth.S120427
Chen H, Feng X, Niu G, Fan Y (2020) Evaluation of dry eye after Implantable Collamer Lens surgery. Ophthalmic Res. https://doi.org/10.1159/000511197
Chen H, Feng X, Niu G, Fan Y (2021) Evaluation of dry eye after implantable collamer lens surgery. Ophthalmic Res 64(3):356–62. https://doi.org/10.1159/000511197
Miu N, Deng Y, Zhang X, Ma K (2021) Study of dry eye after phakic posterior chamber intraocular lens implantation. Int Eye Sci 21(08):1457–1460
Kayhan B, Coskunseven E, Sahin O, Pallikaris I (2019) The effects of implantable collamer lens implantation on higher order aberrations. Int J Ophthalmol 12(12):1848–52. https://doi.org/10.18240/ijo.2019.12.05
Kamiya K, Shimizu K, Aizawa D, Igarashi A, Komatsu M (2009) Surgically induced astigmatism after posterior chamber phakic intraocular lens implantation. Br J Ophthalmol 93(12):1648–51. https://doi.org/10.1136/bjo.2009.160044
Kamiya K, Ando W, Takahashi M, Shoji N (2021) Comparison of magnitude and summated vector mean of surgically induced astigmatism vector according to incision site after phakic intraocular lens implantation. Eye Vision (London, England) 8(1):32. https://doi.org/10.1186/s40662-021-00257-z
Al Habash A, Al Arfaj K, Al AO (2015) Urrets-Zavalia syndrome after implantable Collamer lens placement. Digit J Ophthalmol 21(3):1–11. https://doi.org/10.5693/djo.02.2014.09.002
Srirampur A, Mansoori T, Balijepalli P, Gadde AK (2020) Management of anisocoria and high vault in an eye with implantable collamer lens. Indian J Ophthalmol 68(12):3070–2. https://doi.org/10.4103/ijo.IJO_3030_20
Gharaibeh AM, Liehneova I, Mojzis P, Ziak P, Alio JL (2020) Iris and ciliary body cysts and phakic intraocular lenses. Eur J Ophthalmol 30(5):974–7. https://doi.org/10.1177/1120672119876532
Zhou T-a, Shen Y, Wang Y, Xia J-h (2012) Mid-long term follow-up results in correction of extreme myopia by posterior chamber phakic intraocular lens. Chin J Ophthalmol 48(4):307–311
Chen S, Hodge C, Sutton G, Versace P (2014) Lacquer cracks developing after phakic intraocular lens implantation. J Refract Surg 30(9):646–8. https://doi.org/10.3928/1081597x-20140728-01
Querques G, Delle Noci N (2006) Ultrastructure of the vitreomacular interface in full-thickness idiopathic macular holes: a consecutive analysis of 100 cases. Am J Ophthalmol 142(5):892. https://doi.org/10.1016/j.ajo.2006.08.022
Ripandelli G, Coppe AM, Parisi V et al (2007) Posterior vitreous detachment and retinal detachment after cataract surgery. Ophthalmology 114(4):692–7. https://doi.org/10.1016/j.ophtha.2006.08.045
Panozzo G, Parolini B (2001) Relationships between vitreoretinal and refractive surgery. Ophthalmology 108(9):1663–8. https://doi.org/10.1016/s0161-6420(01)00672-8
Bamashmus MA, Al-Salahim SA, Tarish NA et al (2013) Posterior vitreous detachment and retinal detachment after implantation of the Visian phakic implantable collamer lens. Middle East Afr J Ophthalmol 20(4):327–31. https://doi.org/10.4103/0974-9233.120019
Jun JH, Kim YC, Kim KS (2014) Macular hole after phakic intraocular lens implantation: two cases with divergent manifestations. Semin Ophthalmol 29(4):213–7. https://doi.org/10.3109/08820538.2013.835839
Kumar A, Padhy SK, Dhiman R, Kumar P, Parekh T, Varshney T (2019) Macular hole following phakic intraocular lens implantation and its management. Indian J Ophthalmol 67(10):1758. https://doi.org/10.4103/ijo.IJO_126_19
Martinez-Castillo V, Boixadera A, Verdugo A, Elies D, Coret A, Garcia-Arumi J (2005) Rhegmatogenous retinal detachment in phakic eyes after posterior chamber phakic intraocular lens implantation for severe myopia. Ophthalmology 112(4):580–5. https://doi.org/10.1016/j.ophtha.2004.09.025
Navarro R, Gris O, Broc L, Corcostegui B (2005) Bilateral giant retinal tear following posterior chamber phakic intraocular lens implantation. J Refract Surg 21(3):298–300
Domenech NP, Arias L, Prades S, Pujol O, Rubio M, Caminal JM (2008) Acute onset of retinal detachment after posterior chamber phakic intraocular lens implantation. Clin Ophthalmol 2(1):227–231
Atul K, Subijay S, Jaideep T, Varun G (2011) Early onset giant retinal tear after posterior chamber phakic IOL. Acta Ophthalmol 89(6):E537–E8. https://doi.org/10.1111/j.1755-3768.2010.01965.x
Mushawiahti M, Shaw A, Chiu D (2014) Retinal detachment associated with posterior chamber phakic intraocular lens implantation. Clin Exp Optom 97(5):471–2. https://doi.org/10.1111/cxo.12153
Al-Abdullah AA, Al-Falah MA, Al-Rasheed SA, Khandekar R, Suarez E, Arevalo JF (2015) Retinal complications after anterior versus posterior chamber phakic intraocular lens implantation in a myopic cohort. J Refract Surg 31(12):814. https://doi.org/10.3928/1081597x-20151111-05
Lapeyre G, Delyfer M-N, Touboul D (2018) Retinal detachment after acute posterior vitreous detachment resulting from posterior chamber phakic intraocular lens implantation. J Cataract Refract Surg 44(1):103–5. https://doi.org/10.1016/j.jcrs.2017.10.045
Xu W, Song Z, Huang Y et al (2020) Long-term outcomes of retinal detachment in phakic eyes after implantation of implantable collamer lens v4c for high myopia correction. Frontiers in medicine 7:582633. https://doi.org/10.3389/fmed.2020.582633
Allan BD, Argeles-Sabate I, Mamalis N (2009) Endophthalmitis rates after implantation of the intraocular Collamer lens: Survey of users between 1998 and 2006. J Cataract Refract Surg 35(4):766–9. https://doi.org/10.1016/j.jcrs.2008.12.027
Davis MJ, Epstein RJ, Dennis RF, Cohen JA (2009) Culture-positive endophthalmitis after implantation of intraocular Collamer lens. J Cataract Refract Surg 35(10):1826–8. https://doi.org/10.1016/j.jcrs.2009.05.020
Oum BS, Lee JS, Choi HY, Lee JE, Kim SJ, Lee J-E (2011) Endophthalmitis caused by Pseudomonas aeruginosa after phakic posterior chamber intraocular lens implantation to correct high myopia. Acta Ophthalmol 89(2):E209–E10. https://doi.org/10.1111/j.1755-3768.2009.01782.x
Jalili M, Hashemi H, Jabarvand M, Tabatabai SA (2012) Aspergillus endophthalmitis in one eye subsequent to bilateral anterior chamber phakic intraocular lens implantation. J Refract Surg 28(5):363. https://doi.org/10.3928/1081597x-20120306-01
Kaur M, Titiyal JS, Sharma N, Chawla R (2015) Successful re-implantation of implantable collamer lens after management of post-ICL methicillin-resistant Staphylococcus epidermidis endophthalmitis. BMJ Case Rep. https://doi.org/10.1136/bcr-2015-212708
Taneri S, Kiessler S, Rost A, Schultz T, Elling M, Dick HB (2018) Atypical endophthalmitis after intraocular collamer lens implantation. J Cataract Refract Surg 44(12):1521–3. https://doi.org/10.1016/j.jcrs.2018.08.010
Wilkinson S, Etheridge T, Monson BK, Larochelle MB (2022) Chronic postoperative Cutibacterium acnes endophthalmitis with implantable collamer lens. Am J Ophthalmol Case Rep 26:101500. https://doi.org/10.1016/j.ajoc.2022.101500
Eissa SA (2017) Management of pseudophakic myopic anisometropic amblyopia with piggyback Visian (R) implantable collamer lens. Acta Ophthalmol 95(2):188–93. https://doi.org/10.1111/aos.13203
Gomez-Bastar A, Jaimes M, Graue-Hernandez EO, Ramirez-Luquin T, Ramirez-Miranda A, Navas A (2014) Long-term refractive outcomes of posterior chamber phakic (spheric and toric implantable collamer lens) intraocular lens implantation. Ophthalmol Int 34(3):583–90. https://doi.org/10.1007/s10792-013-9860-1
Eissa SA, Sadek SH, El-Deeb MWA (2016) Anterior chamber angle evaluation following phakic posterior chamber collamer lens with CentraFLOW and its correlation with ICL Vault and intraocular pressure. J Ophthalmol. https://doi.org/10.1155/2016/1383289
Singh A, Gupta N, Kumar V, Tandon R (2018) Toxic anterior segment syndrome following phakic posterior chamber IOL: a rarity. BMJ Case Rep. https://doi.org/10.1136/bcr-2018-225806
Hernandez-Bogantes E, Ramirez-Miranda A, Olivo-Payne A, Abdala-Figuerola A, Navas A, Graue-Hernandez EO (2019) Toxic anterior segment syndrome after implantation of phakic implantable collamer lens. Int J Ophthalmol 12(1):175–7. https://doi.org/10.18240/ijo.2019.01.27
Mimouni M, Alió Del Barrio JL, Alió JL (2020) Occlusion of AquaPORT flow in a case of toxic anterior segment syndrome following implantable collamer lens surgery causing severe pupillary block. J Refract Surg 36(12):856–9. https://doi.org/10.3928/1081597x-20201015-01
Ieong A, Hau SC, Rubin GS, Allan BD (2010) Quality of life in high myopia before and after implantable Collamer lens implantation. Ophthalmology 117(12):2295–300. https://doi.org/10.1016/j.ophtha.2010.03.055
Bai Z, Nie D, Zhang J et al (2022) Visual function assessment of posterior-chamber phakic implantable collamer lenses with a central port. Ann Transl Med 10(4):194. https://doi.org/10.21037/atm-22-107
Zhao W, Zhao J, Han T, Wang J, Zhang Z, Zhou X (2022) A comprehensive investigation of contrast sensitivity and disk halo in high myopia treated With SMILE and EVO implantable collamer lens implantation. Transl Vis Sci Technol 11(4):23. https://doi.org/10.1167/tvst.11.4.23
Bamashmus MA, Al-Arabi AH, Alawad MA (2013) Visual outcomes and patient satisfaction after implantable collamer lens and Toric implantable collamer lens correction for moderate to high myopia and myopic astigmatism. Saudi Med J 34(9):913–919
Lim DH, Lyu IJ, Choi S-H, Chung E-S, Chung T-Y (2014) Risk factors associated with night vision disturbances after phakic intraocular lens implantation. Am J Ophthalmol 157(1):135–41. https://doi.org/10.1016/j.ajo.2013.09.004
Ji-Won K, 신경훈, 김근호 (2011) Two cases of glare after iridotomy for phakic intraocular lens implantation. J Korean Ophthalmol Soc 52(12):1537–1540
Qi M-y, Chen Q, Zeng Q-y (2017) The effect of the crystalline lens on central vault after implantable collamer lens implantation. J Refract Surg 33(8):519-U105. https://doi.org/10.3928/1081597x-20170602-02
Sarikkola AU, Sen HN, Uusitalo RJ, Laatikainen L (2005) Traumatic cataract and other adverse events with the implantable contact lens. J Cataract Refract Surg 31(3):511–24. https://doi.org/10.1016/j.jcrs.2004.06.084
Zhao J, Zhao J, Yang W et al (2021) Consecutive contralateral comparison of toric and non-toric implantable collamer lenses V4c in vault after implantation for myopia and astigmatism. Acta Ophthalmol 99(6):e852–e9. https://doi.org/10.1111/aos.14720
Zhu QJ, Chen WJ, Zhu WJ et al (2021) Prediction of the vaulting after posterior chamber intraocular lens implantation. Zhonghua Yan Ke Za Zhi 57(7):519–25. https://doi.org/10.3760/cma.j.cn112142-20201222-00837
Zhu QJ, Chen WJ, Zhu WJ et al (2021) Short-term changes in and preoperative factors affecting vaulting after posterior chamber phakic Implantable Collamer Lens implantation. BMC Ophthalmol 21(1):199. https://doi.org/10.1186/s12886-021-01963-x
Chen X, Wang X, Xu Y et al (2021) Five-year outcomes of EVO implantable collamer lens implantation for the correction of high myopia and super high myopia. Eye Vision (London, England) 8(1):40. https://doi.org/10.1186/s40662-021-00264-0
Oleszko AA, Marek JJ, Muzyka-Woźniak MM (2021) Horizontal and anterior chamber diameter for phakic intraocular lens sizing. Clin Exp Optom 104(1):62–8. https://doi.org/10.1111/cxo.13101
Chen X, Han T, Zhao W et al (2021) Effect of the difference between the white-to-white and sulcus-to-sulcus on vault and the related factors after ICL implantation. Ophthalmol Ther 10(4):947–55. https://doi.org/10.1007/s40123-021-00386-7
Kamiya K, Shimizu K, Komatsu M (2009) Factors affecting vaulting after implantable collamer lens implantation. J Refract Surg 25(3):259–64. https://doi.org/10.3928/1081597x-20090301-04
Alfonso JF, Fernandez-Vega L, Lisa C, Fernandes P, Jorge J, Montes MR (2012) Central vault after phakic intraocular lens implantation: correlation with anterior chamber depth, white-to-white distance, spherical equivalent, and patient age. J Cataract Refract Surg 38(1):46–53. https://doi.org/10.1016/j.jcrs.2011.07.035
Cerpa Manito S, Sánchez Trancón A, Torrado Sierra O, Baptista AM, Serra PM (2021) Biometric and ICL-related risk factors associated to sub-optimal vaults in eyes implanted with implantable collamer lenses. Eye Vision (London, England) 8(1):26. https://doi.org/10.1186/s40662-021-00250-6
Alfonso JF, Lisa C, Abdelhamid A, Fernandes P, Jorge J, Montes-Mico R (2010) Three-year follow-up of subjective vault following myopic implantable collamer lens implantation. Graefes Arch Clin Exp Ophthalmol 248(12):1827–35. https://doi.org/10.1007/s00417-010-1322-0
Kojima T, Maeda M, Yoshida Y et al (2010) Posterior chamber phakic implantable collamer lens: changes in vault during 1 year. J Refract Surg 26(5):327–32. https://doi.org/10.3928/1081597x-20090617-11
Du G-P, Huang Y-F, Wang L-Q et al (2012) Changes in objective vault and effect on vision outcomes after implantable Collamer lens implantation: 1-year follow-up. Eur J Ophthalmol 22(2):153–60. https://doi.org/10.5301/ejo.2011.8359
Alfonso JF, Lisa C, Fernandez-Vega Cueto L, Belda-Salmeron L, Madrid-Costa D, Montes-Mico R (2013) Clinical outcomes after implantation of a posterior chamber collagen copolymer phakic intraocular lens with a central hole for myopic correction. J Cataract Refract Surg 39(6):915–21. https://doi.org/10.1016/j.jcrs.2013.01.036
Cao X, Tong J, Wang Y et al (2014) Long-term ultrasound biomicroscopy observation of position changes of a copolymer posterior chamber phakic intraocular lens. J Cataract Refract Surg 40(9):1454–61. https://doi.org/10.1016/j.jcrs.2013.12.022
Igarashi A, Shimizu K, Kamiya K (2014) Eight-Year follow-up of posterior chamber phakic intraocular lens implantation for moderate to high myopia. Am J Ophthalmol 157(3):532–9. https://doi.org/10.1016/j.ajo.2013.11.006
Lisa C, Naveiras M, Alfonso-Bartolozzi B, Belda-Salmeron L, Montes-Mico R, Alfonso JF (2015) Posterior chamber collagen copolymer phakic intraocular lens with a central hole to correct myopia: one-year follow-up. J Cataract Refract Surg 41(6):1153–9. https://doi.org/10.1016/j.jcrs.2014.10.030
Cao X, Wu W, Wang Y, Xie C, Tong J, Shen Y (2016) Posterior chamber collagen copolymer phakic intraocular lens with a central hole for moderate-to-high myopia: first experience in China. Medicine (Baltimore). https://doi.org/10.1097/md.0000000000004641
Lee J, Kim Y, Park S et al (2016) Long-term clinical results of posterior chamber phakic intraocular lens implantation to correct myopia. Clin Exp Ophthalmol 44(6):481–7. https://doi.org/10.1111/ceo.12691
Lu Y, Yang N, Li X, Kong J (2017) Four-year follow-up of the changes in anterior segment after phakic collamer lens implantation. Am J Ophthalmol 178:140–9. https://doi.org/10.1016/j.ajo.2017.03.020
Fernandez-Vega-Cueto L, Lisa C, Esteve-Taboada JJ, Montes-Mico R, Alfonso JF (2018) Implantable collamer lens with central hole: 3-year follow-up. Clin Ophthalmol 12:2015–29. https://doi.org/10.2147/opth.S171576
Alfonso JF, Fernandez-Vega-Cueto L, Alfonso-Bartolozzi B, Montes-Mico R, Fernandez-Vega L (2019) Five-year follow-up of correction of myopia: posterior chamber phakic intraocular lens with a central port design. J Refract Surg 35(3):169. https://doi.org/10.3928/1081597x-20190118-01
Alfonso JF, Lisa C, Fernandez-Vega-Cueto L, Besteiro J, Alfonso-Bartolozzi B (2020) Posterior chamber phakic intraocular lens with central port design in 45 to 55 years old patients: one-year follow-up. J Cataract Refract Surg. https://doi.org/10.1097/j.jcrs.0000000000000486
Ye Y, Zhao J, Niu L, Shi W, Wang X, Zhou X (2021) Long-term evaluation of anterior lens density after implantable collamer lens V4c implantation in patients with myopia over 40 years old. Br J Ophthalmol. https://doi.org/10.1136/bjophthalmol-2021-319205
Schmidinger G, Lackner B, Pieh S, Skorpik C (2010) Long-term changes in posterior chamber phakic intraocular collamer lens vaulting in myopic patients. Ophthalmology 117(8):1506–11. https://doi.org/10.1016/j.ophtha.2009.12.013
Choi JH, Lim DH, Nam SW, Yang CM, Chung ES, Chung T-Y (2019) Ten-year clinical outcomes after implantation of a posterior chamber phakic intraocular lens for myopia. J Cataract Refract Surg 45(11):1555–61. https://doi.org/10.1016/j.jcrs.2019.06.015
Gonvers M, Bornet C, Othenin-Girard P (2003) Implantable contact lens for moderate to high myopia - Relationship of vaulting to cataract formation. J Cataract Refract Surg 29(5):918–24. https://doi.org/10.1016/s0886-3350(03)00065-8
Choi KH, Chung SE, Chung TY, Chung ES (2007) Ultrasound biomicroscopy for determining visian implantable contact lens length in phakic IOL implantation. J Refract Surg 23(4):362–367
Dougherty PJ, Rivera RP, Schneider D, Lane SS, Brown D, Vukich J (2011) Improving accuracy of phakic intraocular lens sizing using high-frequency ultrasound biomicroscopy. J Cataract Refract Surg 37(1):13–8. https://doi.org/10.1016/j.jcrs.2010.07.014
Maeng H-S, Chung T-Y, Lee D-H, Chung E-S (2011) Risk factor evaluation for cataract development in patients with low vaulting after phakic intraocular lens implantation. J Cataract Refract Surg 37(5):881–5. https://doi.org/10.1016/j.jcrs.2010.11.037
Sánchez-González JM, Alonso-Aliste F, Perea-Peña G, Rachwani-Anil R, Márquez-de-Aracena-Del-Cid R, Rocha-de-Lossada C (2020) Anterior chamber angle width, central vault and intraocular pressure changes after 12 months of Visian collamer lens implantation. Int Ophthalmol 40(8):2047–53. https://doi.org/10.1007/s10792-020-01381-w
Yang W, Zhao J, Zhao J et al (2020) Changes in anterior lens density after Implantable Collamer Lens V4c implantation: a 4-year prospective observational study. Acta Ophthalmol. https://doi.org/10.1111/aos.14584
Gimbel HV, LeClair BM, Jabo B, Marzouk H (2018) Incidence of implantable Collamer lens-induced cataract. Can J Ophthalmol 53(5):518–22. https://doi.org/10.1016/j.jcjo.2017.11.018
Wei R, Li M, Aruma A et al (2022) Factors leading to re-alignment or exchange after ICL implantation in 10,258 eyes. J Cataract Refract Surg. https://doi.org/10.1097/j.jcrs.0000000000000950
Zaldívar R, Adamek P, Zaldívar R, Domínguez MS, Cerviño A (2021) Intraoperative versus postoperative vault measurement after implantable collamer lens implantation in a large cohort of patients. J Refract Surg 37(7):477–83. https://doi.org/10.3928/1081597x-20210405-03
Kaufer RA, Kaufer GJ (2005) Late subluxation of an ICL. J Cataract Refract Surg 31(6):1254–5. https://doi.org/10.1016/j.jcrs.2005.04.015
Shi M, Kong J, Li X, Yan Q, Zhang J (2015) Observing implantable collamer lens dislocation by panoramic ultrasound biomicroscopy. Eye (Lond) 29(4):499–504. https://doi.org/10.1038/eye.2014.336
Wang R, Fu M, Savini G, Zhao J, Zhang H (2019) Pupillary capture of implantable collamer lens after oral antidepressants. Digit J Ophthalmol 25(4):65–7. https://doi.org/10.5693/djo.02.2019.09.002
Takagi Y, Nakamura T, Ichikawa K, Kojima T (2019) Recurrent prolapse of toric implantable collamer lens after blunt ocular trauma under mesopic conditions. Clin Case Rep 7(4):626–9. https://doi.org/10.1002/ccr3.2055
Zhang H, Deng Y (2022) Complications related to implantable collamer lens (ICL). Int Rev Ophthalmol. https://doi.org/10.3760/cma.j.issn.1673-5803.2022.02.001
Mori T, Yokoyama S, Kojima T et al (2012) Factors affecting rotation of a posterior chamber collagen copolymer toric phakic intraocular lens. J Cataract Refract Surg 38(4):568–73. https://doi.org/10.1016/j.jcrs.2011.11.028
Chen Q, Zeng Q, Wang Z, Pan C, Lei X, Tan W (2020) Spontaneous rotation of a toric implantable collamer lens related to abnormal ciliary body morphology: a case report. BMC Ophthalmol. https://doi.org/10.1186/s12886-020-01597-5
Fairaq R, Almutlak M, Almazyad E, Badawi AH, Ahad MA (2021) Outcomes and complications of implantable collamer lens for mild to advance keratoconus. Int Ophthalmol 41(7):2609–18. https://doi.org/10.1007/s10792-021-01820-2
Ju Y, Gao X-W, Ren B (2013) Posterior chamber phakic intraocular lens implantation for high myopia. Int J Ophthalmol 6(6):831–5. https://doi.org/10.3980/j.issn.2222-3959.2013.06.16
Peraka RP, Murthy SI, Reddy S, Narayanan R (2020) Tale of two complications following phakic intraocular lens implantation: secondary glaucoma and central serous retinopathy in one eye and inverted phakic IOL with cataract in the other eye. BMJ Case Rep. https://doi.org/10.1136/bcr-2020-238300
Edelhauser HF, Sanders DR, Azar R, Lamielle H, Myopia Study G (2004) Corneal endothelial assessment after ICL implantation. J Cataract Refract Surg 30(3):576–83. https://doi.org/10.1016/j.jcrs.2003.09.047
Joshi VP, Vaddavalli PK (2021) Corneal oedema with in situ implantable collamer lens: a challenging scenario for descemet membrane endothelial keratoplasty. BMJ Case Rep. https://doi.org/10.1136/bcr-2020-240709
Alfonso JF, Baamonde B, Fernandez-Vega L, Fernandes P, Gonzalez-Meijome JM, Montes-Mico R (2011) Posterior chamber collagen copolymer phakic intraocular lenses to correct myopia: five-year follow-up. J Cataract Refract Surg 37(5):873–80. https://doi.org/10.1016/j.jcrs.2010.11.040
Subudhi P, Patro S, Agarwal P et al (2020) Safety and efficacy of a new posterior chamber phakic intraocular lens in cases of high myopia: early results. Clin Ophthalmol 14:3681–9. https://doi.org/10.2147/opth.S270690
Moya T, Javaloy J, Montes-Mico R, Beltran J, Munoz G, Montalban R (2015) Implantable collamer lens for myopia: assessment 12 years after implantation. J Refract Surg 31(8):548-U54. https://doi.org/10.3928/1081597x-20150727-05
Olivo-Payne A, Gomez-Bastar A, Lichtinger A, Ramirez-Miranda A, Graue-Hernandez EO, Navas A (2015) More than a decade of experience with implantable collamer lens. J Refract Surg 31(12):854. https://doi.org/10.3928/1081597x-20151118-03
(2021). Long term efficacy and safety profiles following posterior chamber phakic intraocular lens implantation in eyes with ≥ 10-year follow-up. J Cataract Refract Surg. https://doi.org/10.1097/j.jcrs.0000000000000848
Pesando PM, Ghiringhello MP, Di Meglio G, Fanton G (2007) Posterior chamber phakic intraocular lens (ICL) for hyperopia: ten-year follow-up. J Cataract Refract Surg 33(9):1579–84. https://doi.org/10.1016/j.jcrs.2007.05.030
Nakamura T, Isogai N, Kojima T, Yoshida Y, Sugiyama Y (2019) Posterior chamber phakic intraocular lens implantation for the correction of myopia and myopic astigmatism: a retrospective 10-year follow-up study. Am J Ophthalmol 206:1–10. https://doi.org/10.1016/j.ajo.2019.04.024
Le Loir M, Cochener B (2012) Long-term results of posterior chamber phakic intraocular lens implantation for correction of high ametropia. J Fr Ophtalmol 35(6):402–11. https://doi.org/10.1016/j.jfo.2011.06.006
Goukon H, Kamiya K, Shimizu K, Igarashi A (2017) Comparison of corneal endothelial cell density and morphology after posterior chamber phakic intraocular lens implantation with and without a central hole. Br J Ophthalmol 101(11):1461–5. https://doi.org/10.1136/bjophthalmol-2016-309363
Kamiya K, Shimizu K, Igarashi A et al (2018) Posterior chamber phakic intraocular lens implantation: comparative, multicentre study in 351 eyes with low-to-moderate or high myopia. Br J Ophthalmol 102(2):177–81. https://doi.org/10.1136/bjophthalmol-2017-310164
Yasa D, Urdem U, Agca A et al (2018) Early results with a new posterior chamber phakic intraocular lens in patients with high myopia. J Ophthalmol. https://doi.org/10.1155/2018/1329874
Bohac M, Jagic M, Biscevic A, Shijakova V, Gabric N, Patel S (2019) Changes in endothelial cell count up to three years after implantation of toric implantable collamer lenses. Cornea 38(7):873–9. https://doi.org/10.1097/ico.0000000000001914
Shaaban YM, Badran TAF (2020) Three-year effect of phakic intraocular lenses on the corneal endothelial cell density. Clin Ophthalmol 14:149–55. https://doi.org/10.2147/opth.S236041
Yang W, Zhao J, Sun L et al (2021) Four-year observation of the changes in corneal endothelium cell density and correlated factors after implantable collamer lens V4c implantation. Br J Ophthalmol 105(5):625–30. https://doi.org/10.1136/bjophthalmol-2020-316144
Packer KT, Vlasov A, Greenburg DL et al (2021) United States military implantable collamer lens surgical outcomes: an 11 year retrospective review. J Cataract Refract Surg. https://doi.org/10.1097/j.jcrs.0000000000000818
Fernández-Vega-Cueto L, Alfonso-Bartolozzi B, Lisa C, Madrid-Costa D, Alfonso JF (2021) Seven-year follow-up of posterior chamber phakic intraocular lens with central port design. Eye Vision (London, England) 8(1):23. https://doi.org/10.1186/s40662-021-00247-1
Pinto C, Monteiro T, Franqueira N, Faria-Correia F, Mendes J, Vaz F (2021) Posterior chamber collamer phakic intraocular lens implantation: comparison of efficacy and safety for low and moderate-to-high myopia. Eur J Ophthalmol. https://doi.org/10.1177/11206721211012861
Miao HM, Zhao F, Niu LL, Zhao J, Wang XY, Zhou XT (2021) One-step viscoelastic agent technique for ICL V4c implantation for myopia. Int J Ophthalmol 14(9):1359–64. https://doi.org/10.18240/ijo.2021.09.10
Chen Z, Niu L, Zhao J, Yao P, Wang X, Zhou X (2022) One-year observation of safety of implantable collamer lens v4c implantation without using an ophthalmic viscosurgical device. Frontiers in medicine 9:790137. https://doi.org/10.3389/fmed.2022.790137
Pan AP, Wen LJ, Shao X et al (2020) A novel ophthalmic viscosurgical device-free phakic intraocular lens implantation makes myopic surgery safer. Eye Vision (London, England) 7:18. https://doi.org/10.1186/s40662-020-00185-4
Chen D, Cui G, Wang X, Li Y, Luo Y (2020) Safety of the minimum ophthalmic viscosurgical device technique in phakic implantable collamer lens implantation. J Refract Surg 36(1):42–8. https://doi.org/10.3928/1081597x-20191119-02
Peng M, Tang Q, Zhao L, Khan MA, Lin D (2020) Safety of implantable Collamer lens implantation without ophthalmic viscosurgical device: a retrospective cohort study. Med (Baltimore) 99(24):e20691. https://doi.org/10.1097/md.0000000000020691
Kim BK, Chung YT (2021) Comparison of clinical outcomes of implantable collamer lens implantation with and without use of an ophthalmic viscosurgical device. J Cataract Refract Surg 47(2):198–203. https://doi.org/10.1097/j.jcrs.0000000000000417
Qin Q, Bao L, He Z et al (2021) Pure ICL implantation: a novel ophthalmic viscosurgical device-free method. J Ophthalmol 2021:7363267. https://doi.org/10.1155/2021/7363267
Zhang Z, Niu L, Zhao J et al (2021) Safety of EVO ICL implantation with an ophthalmic viscosurgical device-free technique in the early 24 h after surgery. Front Med 8:764653. https://doi.org/10.3389/fmed.2021.764653
Zhao J, Zhao J, Yang W et al (2021) Peripheral anterior chamber depth and angle measurements using pentacam after implantation of toric and non-toric implantable collamer lenses. Frontiers in medicine 8:610590. https://doi.org/10.3389/fmed.2021.610590
Chung T-Y, Park SC, Lee MO, Ahn K, Chung E-S (2009) Changes in iridocorneal angle structure and trabecular pigmentation with STAAR implantable collamer lens during 2 years. J Refract Surg 25(3):251–8. https://doi.org/10.3928/1081597x-20090301-03
Wang X-y, Shen Y, Du C-x, Li Y-m, Dong Y (2009) Observation on changes of anterior chamber and chamber angle structures after posterior chamber phakic intraocular lens implantation by ultrasound biomicroscopy. [Zhonghua yan ke za zhi] Chin J Ophthalmol 45(10):908–12
Wang R-n, Zheng G-y, Wang S-t et al (2011) Quantitative observation on changes of anterior segment by ultrasound biomicroscopy after posterior chamber phakic intraocular lens implantation. [Zhonghua yan ke za zhi] Chin J Ophthalmol 47(9):815–9
Cao X-f, Wang Y, Shen Y et al (2013) Selection of the posterior chamber phakic intraocular lens length. [Zhonghua yan ke za zhi] Chin J Ophthalmol 49(3):235–41
Lim DH, Lee MG, Chung E-S, Chung T-Y (2014) Clinical results of posterior chamber phakic intraocular lens implantation in eyes with low anterior chamber depth. Am J Ophthalmol 158(3):447–54. https://doi.org/10.1016/j.ajo.2014.06.005
Coskunseven E, Kavadarli I, Sahin O, Kayhan B, Pallikaris I (2017) Refractive outcomes of 20 eyes undergoing ICL implantation for correction of hyperopic astigmatism. J Refract Surg 33(9):604–9. https://doi.org/10.3928/1081597x-20170504-06
Ignacio Fernandez-Vigo J, Macarro-Merino A, Fernandez-Vigo C et al (2017) Impacts of implantable collamer lens V4c placement on angle measurements made by optical coherence tomography: two-year follow-up. Am J Ophthalmol 181:37–45. https://doi.org/10.1016/j.ajo.2017.06.018
Galvis V, Tello A, Carreno NI, Nino CA, Berrospi RD (2018) Impacts of implantable collamer lens v4c placement on angle measurements made by optical coherence tomography: two-year follow-up. Am J Ophthalmol 186:171–2. https://doi.org/10.1016/j.ajo.2017.10.034
Kayhan B, Coskunseven E (2022) Changes of ocular biometry in eyes with posterior chamber phakic intraocular lens implantation. J Fr Ophtalmol 45(4):377–83. https://doi.org/10.1016/j.jfo.2021.10.006
Singh R, Vanathi M, Kishore A, Tandon R, Singh D (2020) An anterior segment optical coherence tomography study of the anterior chamber angle after implantable collamer lens-V4c implantation in Asian Indian Eyes. Indian J Ophthalmol 68(7):1418–23. https://doi.org/10.4103/ijo.IJO_1540_19
Fernandes P, Gonzalez-Meijome JM, Madrid-Costa D, Ferrer-Blasco T, Jorge J, Montes-Mico R (2011) Implantable collamer posterior chamber intraocular lenses: a review of potential complications. J Refract Surg 27(10):765–76. https://doi.org/10.3928/1081597x-20110617-01
Almalki S, Abubaker A, Alsabaani NA, Edward DP (2016) Causes of elevated intraocular pressure following implantation of phakic intraocular lenses for myopia. Ophthalmol Int 36(2):259–65. https://doi.org/10.1007/s10792-015-0112-4
Senthil S, Choudhari NS, Vaddavalli PK, Murthy S, Reddy J, Garudadri CS (2016) Etiology and management of raised intraocular pressure following posterior chamber phakic intraocular lens implantation in myopic eyes. PLoS One. https://doi.org/10.1371/journal.pone.0165469
Hu Z, Chen C, Sun M, Yuan R, Ye J (2020) The relationship between anterior chamber angle and intraocular pressure early after v4c implantable collamer lens implantation. J Ophthalmol 2020:4014512. https://doi.org/10.1155/2020/4014512
Chun YS, Park IK, Lee HI, Lee JH, Kim JC (2006) Iris and trabecular meshwork pigment changes after posterior chamber phakic intraocular lens implantation. J Cataract Refract Surg 32(9):1452–8. https://doi.org/10.1016/j.jcrs.2006.04.023
Strungaru MH, Rodriguez JG, Weisbrod DJ, Tayfour F, Buys YM (2020) Acute angle closure following implantable collamer lens for myopia. J Glaucoma 29(7):E74–E6. https://doi.org/10.1097/ijg.0000000000001533
Kamiya K, Shimizu K, Igarashi A, Hikita F, Komatsu M (2009) Four-year follow-up of posterior chamber phakic intraocular lens implantation for moderate to high myopia. Arch Ophthalmol 127(7):845–50. https://doi.org/10.1001/archophthalmol.2009.67
Kamiya K, Shimizu K, Aizawa D, Igarashi A, Komatsu M, Nakamura A (2010) One-year follow-up of posterior chamber toric phakic intraocular lens implantation for moderate to high myopic astigmatism. Ophthalmology 117(12):2287–94. https://doi.org/10.1016/j.ophtha.2010.03.054
Kangyeun P, Lee JW, 김해송 (2013) A case of pigmentary glaucoma after posterior chamber phakic intraocular lens implantation. J Korean Ophthalmol Soc 54(6):994–999
Kocova H, Vlkova E, Michalcova L, Rybarova N, Motyka O (2017) Incidence of cataract following implantation of a posterior-chamber phakic lens ICL (Implantable Collamer Lens) - long-term results. Cesk Slov Oftalmol 73(3):87–93
Shimizu K, Kamiya K, Igarashi A, Shiratani T (2012) Early clinical outcomes of implantation of posterior chamber phakic intraocular lens with a central hole (Hole ICL) for moderate to high myopia. Br J Ophthalmol 96(3):409–12. https://doi.org/10.1136/bjophthalmol-2011-300148
Gonzalez-Lopez F, Bilbao-Calabuig R, Mompean B et al (2013) Intraocular pressure during the early postoperative period after 100 consecutive implantations of posterior chamber phakic intraocular lenses with a central hole. J Cataract Refract Surg 39(12):1859–63. https://doi.org/10.1016/j.jcrs.2013.06.020
Tsintarakis T, Eppig T, Langenbucher A, Seitz B, El-Husseiny M (2015) Can the implantable collamer lens with AquaPORT technology safely prevent an angle block? Early experiences in the Homburg/Saar refractive surgery center. Ophthalmologe 112(5):418–23. https://doi.org/10.1007/s00347-015-3237-y
Badakere SV, Mandal AK (2017) Glaucoma following phakic posterior chamber intraocular lens implantation. Clin Exp Optom 100(2):195–7. https://doi.org/10.1111/cxo.12473
Rodriguez-Una I, Pablo Rodriguez-Calvo P, Fernandez-Vega Cueto L, Lisa C, Fernandez-Vega Cueto A, Alfonso FJ (2017) Intraocular pressure after implantation of a phakic collamer intraocular lens with a central hole. J Refract Surg 33(4):244. https://doi.org/10.3928/1081597x-20170110-01
Navarrete Arguello J, Bello Lopez Portillo H, Cantero Vergara MA et al (2019) Intraocular pressure fluctuations in patients implanted with an implantable collamer lens (ICL V4c). Three-month follow-up. Arch Soc Esp Oftalmol 94(8):367–76. https://doi.org/10.1016/j.oftal.2019.05.010
Gonzalez-Lopez F, Bilbao-Calabuig R, Alen R, Mompean B (2017) Pupillary block glaucoma secondary to central port occlusion following insertion of a phakic implantable copolymer lens. J Cataract Refract Surg 43(11):1468–70. https://doi.org/10.1016/j.jcrs.2017.10.018
Mansoori T, Agraharam SG (2019) Reverse pupillary block after retinal detachment surgery in an eye with toric implantable collamer lens. Ophthalmol Int 39(3):703–10. https://doi.org/10.1007/s10792-018-0848-8
Grover IG, Senthil S, Murthy S, Reddy JC (2017) A rare case of pupillary block glaucoma following centraflow implantable collamer lens surgery. J Glaucoma 26(8):694–6. https://doi.org/10.1097/ijg.0000000000000705
Frost A, Ritter DJ, Trotter A, Pulia MS (2019) Acute angle-closure glaucoma secondary to a phakic intraocular lens, an ophthalmic emergency. Clin Pract Cases Emerg Med 3(2):137–9. https://doi.org/10.5811/cpcem.2019.1.41399
Kodjikian L, Gain P, Donate D, Rouberol F, Burillon C (2002) Malignant glaucoma induced by a phakic posterior chamber intraocular lens for myopia. J Cataract Refract Surg 28(12):2217–21. https://doi.org/10.1016/s0886-3350(02)01213-0
Chanbour WA, Cherfan CG, Jarade EF, Khoury JM (2019) Unilateral malignant glaucoma postbilateral implantable collamer lens: effect of miotics. Middle East Afr J Ophthalmol 26(3):181–3. https://doi.org/10.4103/meajo.MEAJO_197_18
Hu R, Xu W, Huang B, Wang X (2021) Ex-PRESS shunt implantation for intractable glaucoma with posterior chamber phakic intraocular lens: a case report. BMC Ophthalmol 21(1):20. https://doi.org/10.1186/s12886-020-01784-4
Park IK, Lee JM, Chun YS (2008) Recurrent occlusion of laser iridotomy sites after posterior chamber phakic IOL implantation. Korean J Ophthalmol 22(2):130–2. https://doi.org/10.3341/kjo.2008.22.2.130
Winegar JW, Justin GA, Bower KS, Carlton DK (2018) Traumatic aniridia after implantable phakic intraocular lens placement. J Cataract Refract Surg 44(9):1155–7. https://doi.org/10.1016/j.jcrs.2018.06.027
Kocova H, Vlkova E, Michalcova L, Motyka O (2017) Implantation of posterior chamber phakic intraocular lens for myopia and hyperopia - long-term clinical outcomes. J Fr Ophtalmol 40(3):215–23. https://doi.org/10.1016/j.jfo.2016.10.009
Chen L-J, Chang Y-J, Kuo JC, Rajagopal R, Azar DT (2008) Metaanalysis of cataract development after phakic intraocular lens surgery. J Cataract Refract Surg 34(7):1181–200. https://doi.org/10.1016/j.jcrs.2008.03.029
Al-Swailem SA, Al-Rajhi AA (2006) Decentration and cataract formation 10 years following posterior chamber silicone phakic intraocular lens implantation. J Refract Surg 22(5):513–515
Sanders DR, Schneider D, Martin R et al (2007) Toric implantable collamer lens for moderate to high myopic astigmatism. Ophthalmology 114(1):54–61. https://doi.org/10.1016/j.ophtha.2006.08.049
Sanders DR (2008) Anterior subcapsular opacities and cataracts 5 years after surgery in the visian implantable collamer lens FDA trial. J Refract Surg 24(6):566–70. https://doi.org/10.3928/1081597x-20080601-04
Lindland A, Heger H, Kugelberg M, Zetterstrom C (2010) Vaulting of myopic and toric implantable collamer lenses during accommodation measured with visante optical coherence tomography. Ophthalmology 117(6):1245–50. https://doi.org/10.1016/j.ophtha.2009.10.033
Sari ES, Pinero DP, Kubaloglu A et al (2013) Toric implantable collamer lens for moderate to high myopic astigmatism: 3-year follow-up. Graefes Arch Clin Exp Ophthalmol 251(5):1413–22. https://doi.org/10.1007/s00417-012-2172-8
Vasavada V, Srivastava S, Vasavada SA, Sudhalkar A, Vasavada AR, Vasavada VA (2018) Safety and efficacy of a new phakic posterior chamber IOL for correction of myopia: 3 years of follow-up. J Refract Surg 34(12):817–23. https://doi.org/10.3928/1081597x-20181105-01
Kamiya K, Shimizu K, Takahashi M, Ando W, Hayakawa H, Shoji N (2021) Eight-year outcomes of implantation of posterior chamber phakic intraocular lens with a central port for moderate to high ametropia. Front Med 8:799078. https://doi.org/10.3389/fmed.2021.799078
Owaidhah O, Al-Ghadeer H (2021) Bilateral cataract development and pupillary block glaucoma following implantable collamer lens. J Curr Glaucoma Pract 15(2):91–5. https://doi.org/10.5005/jp-journals-10078-1309
Khalifa YM, Moshirfar M, Mifflin MD, Kamae K, Mamalis N, Werner L (2010) Cataract development associated with collagen copolymer posterior chamber phakic intraocular lenses: clinicopathological correlation. J Cataract Refract Surg 36(10):1768–74. https://doi.org/10.1016/j.jcrs.2010.04.039
Fujisawa K, Shimizu K, Uga S et al (2007) Changes in the crystalline lens resulting from insertion of a phakic IOL (ICL) into the porcine eye. Graefes Arch Clin Exp Ophthalmol 245(1):114–22. https://doi.org/10.1007/s00417-006-0338-y
Alfonso JF, Lisa C, Fernandez-Vega L, Almanzar D, Perez-Vives C, Montes-Mico R (2015) Prevalence of cataract after collagen copolymer phakic intraocular lens implantation for myopia, hyperopia, and astigmatism. J Cataract Refract Surg 41(4):800–5. https://doi.org/10.1016/j.jcrs.2014.07.039
Guber I, Mouvet V, Bergin C, Perritaz S, Othenin-Girard P, Majo F (2016) Clinical outcomes and cataract formation rates in eyes 10 years after posterior phakic lens implantation for myopia. JAMA Ophthalmol 134(5):487–94. https://doi.org/10.1001/jamaophthalmol.2016.0078
Petternel V, Koppl CM, Dejaco-Ruhswurm I, Findl O, Skorpik C, Drexler W (2004) Effect of accommodation and pupil size on the movement of a posterior chamber lens in the phakic eye. Ophthalmology 111(2):325–31. https://doi.org/10.1016/j.ophtha.2003.05.013
Maldonado MJ, Garcia-Feijoo J, Del Castillo JMB, Teutsch P (2006) Cataractous changes due to posterior chamber flattening with a posterior chamber phakic intraocular lens secondary to the administration of pilocarpine. Ophthalmology 113(8):1283–8. https://doi.org/10.1016/j.ophtha.2006.03.053
Sanchez-Galeana CA, Smith RJ, Sanders DR et al (2003) Lens opacities after posterior chamber phakic intraocular lens implantation. Ophthalmology 110(4):781–5. https://doi.org/10.1016/s0161-6420(02)01973-5
LeClair BM, Gimbel HV, Fan JT (2016) Long term follow-up of posterior chamber phakic intraocular lens for myopia. Invest Ophthalmol 57(12):3107
Chen X, Wang X, Xu Y et al (2021) Long-term comparison of vault and complications of implantable collamer lens with and without a central hole for high myopia correction: 5 years. Current Eye Res. https://doi.org/10.1080/02713683.2021.2012202
Kaur M, Sahu S, Sharma N, Titiyal JS (2016) Femtosecond laser-assisted cataract surgery in phakic intraocular lens with cataract. J Refract Surg 32(2):131–4. https://doi.org/10.3928/1081597x-20160106-01
Li S, Chen X, Kang Y, Han N (2016) Femtosecond laser-assisted cataract surgery in a cataractous eye with implantable collamer lens in situ. J Refract Surg 32(4):270–2. https://doi.org/10.3928/1081597x-20160217-03
Nath M, Gireesh P (2019) Challenges during femtosecond laser assisted cataract surgery with posterior chamber phakic intraocular lens. Indian J Ophthalmol 67(10):1744–6. https://doi.org/10.4103/ijo.IJO_1852_18
Yu Y, Zhang C, Zhu Y (2020) Femtosecond laser assisted cataract surgery in a cataract patient with a “0 vaulted” ICL: a case report. BMC Ophthalmol 20(1):179. https://doi.org/10.1186/s12886-020-01440-x
AlQahtani BS, Alshamrani AA, Alsulami RE, Vargas JM (2021) A case of implantable collamer lens (ICL) with reverse orientation for 10 years. Case Rep Ophthalmol Med 2021:6641475. https://doi.org/10.1155/2021/6641475
Arnalich-Montiel F, Ruiz-Casas D, Munoz-Negrete F, Reboileda G (2015) Inadvertent cyclodialysis cleft and annular ciliochoroidal detachment after hyperopic phakic intraocular lens implantation and prophylactic surgical iridectomy. J Cataract Refract Surg 41(10):2319–22. https://doi.org/10.1016/j.jcrs.2015.09.010
de Rojas V, Gonzalez-Lopez F, Baviera J (2013) Acetazolamide-induced bilateral choroidal effusion following insertion of a phakic implantable collamer lens. J Refract Surg 29(8):570–2. https://doi.org/10.3928/1081597x-20130719-07
Akkan JCU, Tuncer K, Elbay A (2015) Postsurgical cystoid macular edema following posterior chamber toric phakic intraocular lens implantation surgery: a case report. Case Rep Ophthalmol 6(2):223–7. https://doi.org/10.1159/000437013
Kumar A, Padhy SK, Dhiman R, Kumar P, Parekh T, Varshney T (2019) Macular hole following phakic intraocular lens implantation and its management. Indian J Ophthalmol 67(10):1758–60. https://doi.org/10.4103/ijo.IJO_126_19
Zhang X, Chen H, Li DH, Du H, Chen YY, Luo Y (2021) A case of microvascular anomalies in myopic retinoschisis. [Zhonghua yan ke za zhi] Chin J Ophthalmol 57(12):944–5. https://doi.org/10.3760/cma.j.cn112142-20210731-00360
Zhu QJ, Wang MY, Yu P et al (2020) Analysis of macular microvasculature and thickness after ICL implantation in patients with myopia using optical coherence tomography. Int J Ophthalmol 13(12):1948–54. https://doi.org/10.18240/ijo.2020.12.16
Tae-Hee L, Zheng-Yuan P, Xiang-Yu Po (2014) The change of retinal nerve fiber layer thickness after posterior chamber phakic intraocular lens implantation. J Korean Ophthalmol Soc 55(5):702–710
Hu X, Wang P, Zhu C, Yuan Y, Liu M, Ke B (2021) Transient reduction in the retinal microvascular network following implantation surgery of implantable collamer lens: an OCT angiography study. Mol Vis 27:466–479
Martínez-Plaza E, López-Miguel A, López-de la Rosa A, McAlinden C, Fernández I, Maldonado MJ (2022) EVO+ implantable collamer lens KS-aquaPORT location, stability, and impact on quality of vision and life. J Refract Surg 38(3):177–83. https://doi.org/10.3928/1081597x-20220106-01
Funding
No funding was received for this research.
Author information
Authors and Affiliations
Contributions
HZ wrote the first draft of the manuscript. XLZ and RG supplemented the manuscript. YPD perfected and revised the first draft of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript. All authors declare that they have no conflict of interest. Author Yingping Deng declares that he has no conflict of interest.
Human or animal rights participants
This article does not contain any studies with human participants performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhang, H., Gong, R., Zhang, X. et al. Analysis of perioperative problems related to intraocular Implantable Collamer Lens (ICL) implantation. Int Ophthalmol 42, 3625–3641 (2022). https://doi.org/10.1007/s10792-022-02355-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-022-02355-w