Abstract
Purpose
Our review explains the role of surfactant protein D (SP-D) in different kinds of bacterial infection based on its presence in different ocular surface tissues. We discuss the potential role of SP-D against invasion by pathogens, with the aim of identifying new prospects for the possible mechanism of SP-D-mediated immune processes, and the diagnosis, prognosis, or treatment of ocular bacterial infection.
Methods
We reviewed articles about the role of SP-D in various ocular bacterial infections or infection-related ocular diseases through PubMed, Google Scholar, and the Web of Science databases.
Results
SP-D acts as an important immune factor that can resemble molecules in different polymerization states and that defends against pathogen invasion. The increased SP-D production and secretion in tear fluid and the cornea after ocular bacterial infections such as Staphylococcus aureus, Pseudomonas aeruginosa keratitis, and infection-related ocular diseases, was shown to have potential anti-inflammatory effects. The mechanisms of SP-D’s action against ocular bacterial infections include presenting, aggregating, opsonizing, and phagocytizing antigens, as well as regulating anti-bacterial immunity processes, including toll-like receptor-5 (TLR-5) pathway and IL-8 effect, TLR-4 and TLR-2 pathways and other possible ways remained to be elucidated in more detail. The findings demonstrate the potential of SP-D as an important clinical diagnostic biomarker prognosis predictor, and target for ocular immunotherapy.
Conclusion
SP-D participates in invasion by different ocular bacteria and infection-related ocular diseases through multiple immune mechanisms. This finding provides new prospects for the diagnosis, prognosis and treatment of ocular bacterial infection.
Similar content being viewed by others
Introduction
Surfactant protein D (SP-D), a collagenous C-type lectin, is widely expressed in tissues and organs including the human lung, trachea, kidney, brain, salivary gland, and other extrapulmonary tissues [1]. SP-D is secreted mainly by the alveolar epithelium, and plays a vital role in the immunological and anti-inflammatory processes necessary for the homeostatic stabilization of the lungs [2]. The carbohydrate recognition domain (CRD), one of four domains comprising SP-D, enables ligands to recognize mannose-rich microbial molecular patterns and to surveil anti-bacterial innate immune responses [3]. The mechanisms of SP-D in immune activities include mediating the clearance of pathogens by aggregating them to bronchial mucociliary, macrophages or recruited neutrophils [4, 5], then enhancing phagocytosis of antimicrobial particles or upregulating recognition receptors [6]. SP-D also mediated the chemotaxis and degranulation of human eosinophils [7], which showed the potential to prevent the development and deterioration of lung inflammatory or allergic responses. Consequently, SP-D is closely related to several lung diseases and acts as a biomarker in pneumonia [8], chronic obstructive pulmonary disease (COPD) [9], and asthma [10].
In addition to its role SP-Din the lungs, SP-D was found recently on the human ocular surface and in tear fluid, and lacrimal glands and passages. SP-D is commonly produced from the superficial layers of the human cornea and conjunctiva in vivo, or human corneal and conjunctival epithelial cells in vitro, then diffused into the tear fluid through the efferent lacrimal system. The mRNA level of SP-D can be detected in the lacrimal gland, nasolacrimal ducts, conjunctiva, cornea and tear film [11]. The levels of SP-D transcription and protein production were higher after bacterial infection in human tear fluid and corneal epithelial cells, suggesting that SP-D is likely to act in defending against ocular bacterial infection [12, 13]. Recent studies focusing on other ocular diseases also showed the antifungal properties of SP-D [14] and its role in antiviral defense [15] and dry eye diseases [16], which indicated the potential anti-inflammatory effects of SP-D. However, its innate immune mechanisms need to be explored in more depth.
Ocular bacterial infection refers to the invasion of bacterial pathogens, especially gram-positive bacteria, into the eye immune barriers formed by oculofacial structures, damaging them and causing visual impairments and even severe blindness without proper treatment [17]. The most superficial layers of the oculofacial structure, including the conjunctival epithelium, corneal epithelium, and tear film, participate in the defense against external pathogenic microorganisms outside the intraocular structure and tissue. Moreover, a series of antibacterial substances and reactions also participate in the ocular immune defenses [18]. The balance between pro-and anti-inflammatory factors and responses, and the interplay between cellular apoptosis versus necrosis, also systematically regulates the ocular surface micro-environment. SP-D is involved in the anti-bacterial action of the human eye in two main aspects: (a) SP-D plays an opsonizing role, combining with bacteria and preventing them from invading the ocular surface barrier; and (b) SP-D adjusts the balance between pro- and anti-inflammatory factors to maintain the stability of the ocular surface microenvironment. Recent studies have discussed the action of SP-D in antigen presentation [19], aggregation, opsonization, and phagocytosis [20], as well as its effect in anti-bacterial immunity regulation processes, including the TLR-5 pathway and IL-8 effect [12], the TLR-4 pathway and the TLR-2 pathway [21]. Other possible mechanisms remain to be elucidated in more detail. Although the functional roles of SP-D and the relationship between SP-D and other aspects need to be explained, SP-D’s multiple mechanisms of action work together in the development or regression of bacterial keratitis in ocular bacterial infection. SP-D may be a vital protector in the defenses against ocular bacterial infection.
As acute ocular bacterial infection needs to be treated as an emergency, and antibiotic resistance generally occurs in regular treatment [22], non-invasive methods of diagnosis and prognosis and new therapies relying on immune defenses in the eyes seem to be vital. SP-D exists in most human tissues, including the upper surface of the eyes and tear fluids, and it might have the potential to help control keratitis, conjunctivitis, and other inflammatory-related ocular diseases. Therefore, our review first explains the role of SP-D in different kinds of bacterial infection in the eyes, with the aim of proposing its possible mechanisms, as well as methods of diagnosis, prognosis, and treatment of ocular bacterial infection using SP-D.
Materials and methods
Articles about the role of SP-D in various ocular bacterial infections and infection-related ocular diseases were thoroughly reviewed using PubMed, Google Scholar, and the Web of Science databases. Keywords included “surfactant protein D,” “ocular bacterial infection,” “bacterial keratitis,” “ocular surface,” “diagnosis,” “prevention,” “treatment,” “therapy,” “inflammation,” and “immunity.” We searched for relevant research using these words in different combinations.
SP-D structure
As part of the C-type lectins (CTLs) family of collectins, also called carbohydrate-binding lectins or pathogen recognition receptor proteins, SP-D is capable of recognizing and binding pathogens’ sugar moieties. The members of this family include classical surfactant protein-A (SP-A) and mannose-binding lectin, as well as novel members such as collectin liver 1(CL-L1), collectin kidney 1(CL-K1), and collectin placenta 1 (CL-P1) [23, 24]. SP-D, like SP-A, is encoded by the long arm of chromosome 10 [25]. The primary structure of this 43-kDa polypeptide consists of four domains: an N-terminal domain, a triple-helical collagen body, an alpha-helical coiled neck region, and a carbohydrate recognition domain (CRD) [26]. The CRD was specified to play the most important part in SP-D’s defense against bacterial invasion [27]. In humans, collectins have well-conserved oligomeric structures suited to their increasing need for functional affinity to their ligands with an extended range of their CRDs. SP-D was found to assemble into high-molecular forms, such as a cruciform of trimeric subunits, and even higher-order multimers including hexamers and dodecamers [28]. The largest collectin polymerization of SP-D monomers, also called fuzzy balls, contributed to triggering more effective bacteria aggregation [29] (Fig. 1).
SP-D structure. The primary structure of SP-D is formed by the N-terminal domain, collagen body, neck region, and carbohydrate recognition domain (CRD). SP-D forms a trimeric subunit as the minimal protein unit and polymerizes into hexamers, dodecamers, or fuzzy balls as functional proteins in anti-bacterial immune responses
The N-terminal domain contains seven amino acids that form the short peptide responsible for the oligomerization of disulfide bridges. A strong hydrophobic interaction between the collagen body and the neck region was found [30]. A repeating glycine (Gly)-X–Y peptide structure, with X and Y representing mostly proline and hydroxyproline, constitutes the collagen body. The CRD can recognize various carbohydrate ligands in microorganisms based on the presence of Ca2+. Ligands can be recognized broadly including not only a series of carbohydrates, such as glucose, fucose, N-acetylglucosamine, and N-acetylmannosamine, but also proteins, nucleic acids, and lipids [4, 31]. Although the members of the CTL family share a similar structural homology, SP-D is bound specifically with inositol, maltose and glucose in pathogens rather than with galactose and sialic acid in most vertebrate animals’ oligosaccharides [32]. The ability to distinguish pathogens from normal human cells endows SP-D with meaningful immunity function. Several studies proved that SP-D participates in the processes of opsonization [33], aggregation, ligand-receptor association [34], and the direct killing of pathogens [35].
Evidence of SP-D participation in ocular bacterial infections
Staphylococcus aureus infection
The Staphylococcus species of infection remains the cause of several leading clinical problems in bacterial keratitis, creating an increasing number of multidrug-resistant strains to be treated [36]. SP-D participates in innate immunity to corneal impairment by Staphylococcus aureus (S. aureus) through its function of binding bacteria and regulating the balance of protease inhibitors. The CRD structure of SP-D, which binds carbohydrate sites and thus exposes lipoteichoic acid and peptidoglycan on the surface of S. aureus, provides structural evidence for its binding function [37, 38]. Positive results of SP-D proteins were shown in normal superficial layers of corneal and conjunctival epithelia, instead of endothelial or stromal cells, using immunohistochemical staining. However, the positive staining reaction of SP-D could be found in the periphery of corneal ulcers, corneal stroma and endothelium areas when invaded by S. aureus, suggesting the induction of SP-D after bacterial stimulation [11]. In mice experiments, the expression of SP-D was also up-regulated in the corneal epithelium and endothelium, and acinar cells of the lacrimal gland, after S. aureus challenge. In addition, SP-D regulated the balance between proteases and protease inhibitors, ensuring the stable environment of the ocular surface [39]. Invasive bacteria could release cysteine protease that would impair SP-D functioning, but cysteine protease inhibitor inhibited this process. Therefore, cysteine protease inhibitor can enhance the protective function of SP-D and reduce bacterial adherence as a potential therapeutic agent for S. aureus keratitis [13]. The protective role of cysteine protease inhibitor was also shown in corneal tissue that underwent fusarium damage [40]. Overall, SP-D acts positively after S. aureus invasion to maintain the stable state of the ocular surface.
Pseudomonas aeruginosa infection
Pseudomonas aeruginosa (P. aeruginosa) represents the common gram-negative opportunistic bacterium causing keratitis, corneal ulcers and eventually sight loss. Ocular P. aeruginosa infection is most strongly related to contact lens wear [41], followed by ocular and systemic diseases and trauma [42]. P. aeruginosa can be divided into at least two strains, invasive and cytotoxic, both of which can damage corneal epithelial cells [43, 44]. Both of strains target corneal surface cells in vitro but fail to infect healthy corneas in vivo, indicating that protective factors, such as lactoferrin, lysozyme [45], secretory phospholipase A2 [46], defensins [47], and SP-D are present in the healthy ocular surface [12]. Therefore, studies usually focus on the epidemiology of patients wearing contact lenses [41] or models of mice with injured corneas [48]. In this section, we discuss the role of SP-D in ocular P. aeruginosa infection.
SP-D in tear fluid
As a protective factor in tear fluid, SP-D plays a role in ocular immune defenses. Fleiszig has confirmed that human tear fluid can protect the corneal epithelium from P. aeruginosa virulence [49]. This kind of cytoprotective effect could not be eliminated by boiling or diluting tear fluid, showing that this is not a heat-labile function and that the intervention of tear bacteriostatic activity and bacterial motility can be excluded from possible reasons for the protective effect. Therefore, the antimicrobial function of tear fluid is complex and multifactorial.
The function of some anti-bacterial factors relies on the participation of corneal epithelial cells. A previous study proved that SP-D existed in human tear fluid and corneal epithelia [50]. The higher expression of SP-D mRNA and proteins after P. aeruginosa infection in human corneal epithelial cells shows that SP-D could protect tear fluid by increasing SP-D productions [12]. Another study proved that the degradation of SP-D is related to P. aeruginosa elastase in vitro and in vivo, suggesting a possible interaction between SP-D and bacterial clearance. It is worth mentioning that proteases took part in the in vivo and in vitro immune responses to P. aeruginosa, as purified elastase could degrade SP-D in tear fluid in vivo, while P. aeruginosa proteases could enhance the virulence of the infection [51]. SP-D recognizes P. aeruginosa through its CRD structure and binds the pathogens in a calcium-dependent way. However, SP-D can be bound to P. aeruginosa wall via the probable calcium-independent connection of an additional tear component that cannot be removed by mannan-sepharose enzyme-linked immunosorbent assay [50]. The relationship of SP-D to other chemicals in tear fluid must be investigated separately.
The invasive and cytotoxic strains of P. aeruginosa highlight the various immunomodulatory properties of SP-D [52]. Cytotoxic strain 6206, which produces a lower quantity of protease compared to strain PAO1 and expresses a powerful cytotoxin, was found to have delayed clearance from the ocular surface in SP-D-deficient mice. However, the protease mutant of the PAO1 strain was less easily cleared than the wild-type strain in SP-D-deficient mice [51]. Therefore, the protective effects of SP-D and bacterial virulence were found to differ among strains.
SP-D in the cornea
Corneal epithelial cells function as both physical and biochemical barriers. The rapid clearance of a large amount of P. aeruginosa in healthy mouse corneas showed the effective protective function of SP-D in vivo [51], so the establishment of animal models with bacterial corneal keratitis has always been based on invasive procedures [53, 54]. However, non-damaged multilayers of corneal epithelial cells could still be traversed by P. aeruginosa in vitro [55]. This implies that there exist additional defenses against invasion of the cornea in vivo, other than physical barriers including intercellular tight junctions and basement membranes, and protective factors in tear fluids. A previous study proved that SP-D contributed to corneal defense, but called for more studies to identify the mechanisms of this defense [50]. Tissue paper blotting was proposed to test the damage caused by an ethylene glycol tetraacetic acid (EGTA) solution, which disrupts calcium-dependent junction barriers. Deeper bacterial penetration resulted from EGTA-treatment than from the absence of SP-D, which resulted only in superficial invasion, suggesting that calcium-dependent factors other than SP-D likely contribute to cornea protection [56]. Taken together, both EGTA-sensitive factors and SP-D limit the traversal of P. aeruginosa in the cornea, and corneal bacterial defenses may be multifactorial and redundant.
Infection with other pathogens
Lipoarabino-mannan of Mycobacterium tuberculosis, infection of which usually leads to ocular tuberculosis or tubercular retinochoroiditis, can bind to SP-D and reduce phagocytosis function by macrophages [57]. SP-D enhances the phagocytosis and aggregation of Chlamydia pneumoniae in THP-1 cells, suggesting that it may be involved in the eye’s innate host defense [58]. The specific relationship between human SP-D and Salmonella enterica lipopolysaccharide (LPS) was studied recently [59].
SP-D in infection related ocular diseases
SP-D in dry eye (DE)
The pathogenesis of contact lens-related infections may have relevance for ocular surface disorders. Studies have described the occurrence of dry eye (DE) as an inflammation process mediated by oxidative stress, lymphocytes, and proinflammatory cytokines, such as IL-8 or MMP-9, in the ocular surface [60, 61]. Conventional culture showed a higher mean number of bacteria in DE patients than in normal subjects, but no statistically significant difference between them was found using polymerase chain reaction amplification of 16S rDNA detection [62].
It is not yet known whether inflammatory factors, including SP-D, will benefit dry eye disease or experimentally induced dry eye (EDE) in a way similar to bacterial infection, especially contact lens related P. aeruginosa infection. SP-D contributes to corneal defense in EDE, despite barrier loss. Before and 6 h after bacterial inoculation, elevated expression of SP-D proteins and fewer bacteria (p = 0.049, Mann–Whitney test) were observed in ocular washes of EDE wild-type mice compared to normal controls, indicating the enhanced P. aeruginosa clearance function of SP-D. The result of increased P. aeruginosa corneal colonization (∼ fivefold) after bacterial inoculation was shown in SP-D knockout EDE mice [63]. However, a recent study suggested that EDE did not enhance the epithelium, stroma, or endothelium corneal layers and that the conjunctival surface is more susceptible to live bacterial colonization, regardless of the influence of the specific species of bacteria studied [64]. The significant upregulation (p < 0.05, one-way ANOVA) of SP-D proteins in tear fluids from DE patients compared to healthy controls reflects the potential antimicrobial and immune regulating functions of SP-D and requires the further experimental investigation [16].
SP-D in lacrimal apparatus diseases
SP-D has also been confirmed to play an important role in lacrimal apparatus diseases, such as functional nasolacrimal duct obstruction and infective dacryocystitis. It was proven that SP-D exists in the epithelium of the lacrimal sac and nasolacrimal ducts. Surfactant proteins (SPs) regulate tear flow speed and maintain the mucosal defenses of the lacrimal drainage system against microbes, and participate in the pathological processes of infectious dacryocystitis [65]. The strong expression of SPs in the canalicular system, including SP-D, provided some new hypotheses of their functions in lacrimal drainage defenses [66].
The immune mechanism of SP-D in ocular bacterial infection
SP-D mediated antigen presentation, aggregation, opsonization and phagocytosis
Considered to be a secreted pattern recognition molecule, SP-D was proven to serve as a mediator for the direct killing of pathogens as part of organism’s innate immunity. Previous studies claimed that the multiple trimeric lectin subunits of SP-D were served to connect Pseudomonas aeruginosa [67]. SP-D primarily stimulates dendritic cells presenting antigens, while SP-A inhibits processes of antigen presentation. Both of these SPs promote phagocytic cell uptake by increasing the expression of surface receptors and are then activated as models for binding and aggregating bacteria [19, 68]. The main antigens for aggregation in gram-negative bacteria are LPS, while gram-positive bacteria rely on lipoteichoic acid (LTA) and peptidoglycan [38, 69]. However, the binding of SP-D and bacteria is not sufficient to induce obvious aggregation, while SP-D acts mainly as an opsonin to enhance phagocytosis or other immune cell response [4, 67]. For instance, as a surface receptor, CD14 can bind to LPS, the process of which might be broken by the ligand-binding of SP-D in the solid phase or enhanced through the ligand-passing of SP-D to stimulate the following LPS-mediated pathways in the fluid phase [52].
Although not all LPS phenotypes induce collectin-mediated aggregation, other mechanisms of connection, (e.g., other cell wall glycoconjugates) can enhance aggregation by SP-D. Interestingly, SP-D interplayed with the core oligosaccharide of rough P. aeruginosa LPS and stimulated the release of tumor necrosis factor-ɑ (TNF-ɑ) by the human monocytic cell line Mono Mac 6, whereas the cytokine response was not activated by smooth LPS. The differences between LPS serotypes might be responsible for the diversity of their binding proteins or their presentation toward target cells, as well as for changing the signal transduction and the activation of proinflammatory cytokines [70]. Furthermore, the direct killing effect of SP-D and SP-A was reflected in the increasing permeability of the Escherichia coli K12 membrane for the clearance of gram-negative bacteria without the assistance of phagocytosis [35]. Rough LPS is more susceptible to permeabilization, with oxidative damage aggravating this function [71]. A study assumed that SP-D-mediated antigen immune responses might have two-step mechanisms, including direct killing, primarily, and LPS-mediated cytokine responses, secondarily. The smooth P. aeruginosa–LPS seemed to need more complex immune responses [52].
In conclusion, multiple factors contribute to the interactions among antigen presentation, aggregation, opsonization, and phagocytosis of different bacteria strains. SP-D may take part in the various host responses found in in vitro studies. The inter-reaction between SP-D and LPS might be effective for bacterial immune defenses when LPS is exposed to tear fluid. The diversity of connections between bacteria strains and LPS results from the presence of glycoconjugate structures, and density, or the micro-organization of LPS.
In an experiment using a mice model, significantly lower slit-lamp scores (p ≤ 0.0185) were presented in SP-D deficient Black Swiss mice than in wild-type mice 3 and 6 days after infection, and the bacteria count per cornea was be significantly lower (p ≤ 0.0233) in wild-type mice than in Black Swiss mice. It was proven that SP-D-deficient mice have lower resistance to P. aeruginosa infection than wild-type mice. The numbers of gathered polymorphonuclear neutrophils (PMNs) or other phagocytic cells 2 or 3 days after infection was revealed. SP-D likely acts as a host defense molecule to uptake pathogens against P. aeruginosa keratitis but must be supported by phagocytosis [20].
SP-D regulating anti-bacterial immunity processes
Flagellin-mediated toll-like receptor-5 pathway and IL-8 effect
Human corneal epithelial cells can up-regulate SP-D in response to P. aeruginosa, and purified flagellin or LPS can mediate this up-regulation. A previous study showed that P. aeruginosa flagellin interact with innate Toll-like receptor-5(TLR-5) in the internal layers of corneal stratified epithelium when bacteria enter or break the epithelial barrier, and the flagellin then induce IL-8 expression to trigger the defensive NF-kappaB (NF-κB) signal system in cultured human corneal epithelial cells [72]. Although SP-D can be induced by flagellin, flagellin receptor-binding sites were observed to be separated from the receptors for IL-8 induction, as there was no reduction in the upregulation of SP-D mRNA when treated with the SP-D mutations, which reduced the IL-8 response [12]. Another study suggested that IL-8 mediates neutrophil infiltration in corneal infections and could work synergistically with the defensive functions of SP-D [54]. Therefore, the relationship between IL-8 and SP-D can be either synergistic or separable, and the separation of receptor-binding sites allows IL-8 and SP-D to activate one response without the other, which may be beneficial for the limitation of excessive anti-inflammatory actions in ocular bacterial infection. Further clear evidence for flagellin-induced SP-D upregulation through TLR-5 processes is required, as other complex regulatory pathways may contribute to this upregulation.
IL-8 contributes importantly to corneal tissue repair, relying on activated corneal stromal fibroblasts that induce the mitogen-activated protein kinase (MAPK) pathway to stabilize the expression of IL-8 mRNA and proteins [73]. As a member of the MAPK family, JNK1 played an important role in anti-inflammatory processes as it served as positive feedback controlled by NF-κB for increased IL-8 release [74]. Conclusion of the participation of IL-8 and JNK1 in anti-inflammatory processes provided possible explanations for the results of a previous study that showed the involvement of MAPK signaling in SP-D secretion, suggesting that MAPK inhibitors reduce the secretion rather than the level of SP-D in human corneal epithelial cell lysates [12]. Addition evidence at the genetic level included that various transcription factor-binding sites were found in the SP-D gene promoter, including the MAPK-activated AP-1 transcription factors [75]. MAPK was found to play a similar role in corneal inflammation caused by DE [76] and hyperosmolar stress [77]. Therefore, the regulation of MAPK signaling is complex, and other common pathways or negative regulation between SP-D and IL-8 responses need to be further determined. The circumstances under which TLR5 and MAPK pathways may be of benefit for IL-8 are still unclear.
LPS mediated toll-like receptor-4 pathway
Toll-Like Receptor-4(TLR-4) is one of the most important receptors in the innate ocular immune system for the recognition of LPS. In a BALB/c mice model, the expression of TLR4 mRNA was significantly upregulated (p < 0.001, p < 0.0001, p < 0.0001, and p < 0.01 at 1, 3, 5, and 7 days postinfection) in P. aeruginosa corneal infection. The TLR-4-deficient mice had higher bacterial loads in the cornea compared with the wild type mice, together with significantly increased PMN recruitment and proinflammatory cytokine production, including interleukin-1β (IL-1β), macrophage inflammatory protein-2 (MIP-2), and interferon-γ(IFN-γ) production, therefore resulting in the increased occurrence of inflammation processes. Moreover, the reduced mRNA levels of nitric oxide (NO) and defensin-β-2 indicated impaired bacterial killing [21]. Studies have presumed that SP-D limits the interaction among pathogens and TLR-4 in the infected state. However, it was reported that natural or recombinant SP-D is bound to the extracellular domains of TLR2 and TLR4 differently from the way it combines with Escherichia coli LPS. Both combinations with TLR-2 and TLR-4 required binding sites in the CRD structure of SP-D; these sites were spatially proximal to each other, having the relatively direct effect of regulating the LPS-mediated TLR-4 pathway [78]. In addition, as the coreceptor of TLR-4, the myeloid differentiation protein 2(MD-2) was responsible for initiating LPS signaling when formed in the TLR4/MD-2 complex. SP-D hypo-activates the LPS-elicited inflammatory responses by decreasing the bond between MD-2 and LPS, specifically resulting in the down-regulation of TNF-αand NF-κB activation [79].
A recent study showed that the mRNA and protein levels of SP-D increased in human corneal epithelial cells after Aspergillus fumigatus infection but decreased 24 h and 36 h later. This negative feedback control of SP-D might be due to the synthesis and consumption of mRNA. As TLR4 inhibitors reduced the IL-1β and IL-8 production activated by A. fumigatus, SP-D was proven to connect LPS recognition and IL-8 response through TLR4-MyD88/NF-kB pathway, the expression of which might conversely be regulated by TLR4-Jnk activation. SP-D down-regulated the immune reaction against fungal infection, but not bacterial infection clearly via the TLR-4 signaling pathway [80]. The direct link between SP-D and the LPS-mediated TLR-4 pathway in ocular bacterial infection thus needs to be proven by further experiments.
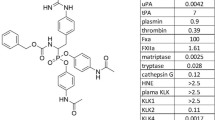
The toll-like receptor-2 pathway
SP-D is also the ligand for TLR-2 and mediates a similar expression of cytokines as SP-A [78]. Although the peptidoglycan of S. aureus was regarded as a TLR-2 activator [81], its lipoprotein seemed to play a critical role in activating TLR2 and MyD88 in the processes of inflammatory cytokine production and neutrophil recruitment in the cornea [82]. The connection between SP-D and the TLR-2 pathway is worth investigating for the clinical application (Table 1).
The role of SP-D in the diagnosis, prognosis, and treatment of ocular bacterial infection
The present rapid method of diagnosing infectious keratitis relies on the patient’s clinical history and empirical examination of typical ocular characteristics under a slit lamp by optometrists. This diagnostic method can be misleading due to differential pathogen virulence, topical administration at an early stage of infection or a history of corneal disease. Corneal smears and bacterial cultures are commonly used as gold-standard diagnostic methods, but their limitations include invasive sampling operations, long-duration cultivation, and low positive detection rates. Recent studies have shown elevated SP-D levels after viral [83], fungal [80], and bacterial infection [13], as well as allergic reactions on the ocular surface [84], which are significant factors in ocular immune defenses and assist in distinguishing between infectious and non-infectious keratitis. SP-D has been used to diagnose and evaluate bacterial infection-related inflammation. SP-D in serum or bronchoalveolar lavage fluid acts as an important biomarker reflecting lower airway inflammation for differential diagnosis, evaluation of severity, or prediction of prognosis of chronic obstructive pulmonary disease [85], Idiopathic pulmonary fibrosis [86], asthma [87], and pneumonia [8, 88], but the methods of collecting serum and lavage fluid are invasive. The higher level of SP-D in nasal lavage fluid from patients with chronic rhinosinusitis was found to be a useful adjunct to identification methods for upper airway inflammation [89]. Elevated salivary SP-D might reflect small airways and could help monitor the degree of exacerbation of childhood asthma [10]. Hence, elevated levels of SP-D expression in ocular bacterial infection could provide new information for the diagnosis of early infection in the lacrimal system and tear fluid, as well as untypical corneal damage. The quantitative determination of SP-D may reflect ocular inflammation in human tear fluid and corneas, and could be used as a non-invasive and easily obtainable diagnostic biomarker for monitoring the degree of inflammatory response in place of invasive methods of collecting biomarkers. The specificity and sensibility of SP-D are worthy of further study in clinical trials, as SP-D can be induced by various types of infectious keratitis and ocular allergic inflammation.
The N-terminal domain of SP-D shows its polymorphic variation at the genetic level and could influence the oligomerization, function, and concentration of its production in the ocular surface [90]. The genetic single nucleotide polymorphisms (SNP) of SP-D have been studied in lung diseases [91, 92], allergic rhinitis [93], and acute kidney injury [94], indicating the ability of specific SP-D genotypes to predict susceptibility to and prognosis of these diseases. SP-D SNP could influence the function and concentration of SP-D protein, therefore resulting in a higher degree of oligomerization for ocular bacterial inhibition [95]. The genetic polymorphism of SP-D may act as a predictor of susceptibility to and prognosis of bacterial keratitis.
Although the most effective treatment for bacterial keratitis is still topical antibiotics therapy, the frequent occurrence of drug resistance remains an emergent problem. Elucidating the mechanisms of SP-D’s participation in innate ocular immune systems provides ideas for the treatment of ocular bacterial infection. Such treatments could be multidimensional and involve the application of multiple factors and related therapies, for example, the cysteine protease inhibitor mentioned above or recombinant fragments of human (rfh) SP-D. rfhSP-D, which consists of an a-helical neck with three CRDs, can recognize and bind to pathogens, activate immune cells, and release cytokine and chemokine products, showing its potential as an immunotherapy target [96]. Smaller rfhSP-D proteins have been developed and are easy to access in an economical way from E. coli [97]. rfhSP-D has been under development recently for the treatment of pulmonary inflammatory diseases, such as bronchopulmonary dysplasia, chronic obstructive pulmonary disease, asthma, and even COVID-19 [83, 98]. Multiple studies discussed above have suggested the anti-bacterial function and therapeutic potential of SP-D in ocular bacterial infection, and it would be worthwhile to conduct more clinical trials in the future.
Conclusion
SP-D, which belongs to the CTL family, comprises four domains, among which CRD is an important antigenic domain with a role in ocular bacterial defenses. Previous studies have proven that the expression of SP-D increases in tear fluid and corneas after bacterial infection, such as S. aureus infection and P. aeruginosa infection, and infection-related ocular diseases, including DE and lacrimal apparatus diseases. The immune mechanisms of SP-D consist of two main aspects: (a) assisting and enhancing the recognition, presentation, aggregation, opsonization, and phagocytosis of various antigens, and (b) regulating different immune pathways, including the flagellin-mediated TLR-5 pathway and IL-8 effect, the LPS- mediated TLR-4 pathway and TLR-2 pathways, therefore maintaining the micro-environment of the ocular surface. Recent studies have shown potential clinical applications of SP-D for the diagnosis, prognosis, and treatment of ocular bacterial infection, and more clinical trials should be conducted, such as studies in the SNP of SP-D, or the potential value of SP-D as a diagnostic biomarker and a therapeutic target in ocular bacterial infection.
References
Madsen J, Kliem A, Tornoe I, Skjodt K, Koch C, Holmskov U (2000) Localization of lung surfactant protein D on mucosal surfaces in human tissues. J Immunol 164:5866–5870
Kendall M, Ding P, Mackay RM, Deb R, McKenzie Z, Kendall K, Madsen J, Clark H (2013) Surfactant protein D (SP-D) alters cellular uptake of particles and nanoparticles. Nanotoxicology 7:963–973
Sano H, Kuroki Y (2005) The lung collectins, SP-A and SP-D, modulate pulmonary innate immunity. Mol Immunol 42:279–287
Wright JR (2005) Immunoregulatory functions of surfactant proteins. Nat Rev Immunol 5:58–68
Sorensen GL (2018) Surfactant protein D in respiratory and non-respiratory diseases. Front Med (Lausanne) 5:18
Beharka AA, Crowther JE, McCormack FX, Denning GM, Lees J, Tibesar E, Schlesinger LS (2005) Pulmonary surfactant protein A activates a phosphatidylinositol 3-kinase/calcium signal transduction pathway in human macrophages: participation in the up-regulation of mannose receptor activity. J Immunol 175:2227–2236
von Bredow C, Hartl D, Schmid K, Schabaz F, Brack E, Reinhardt D, Griese M (2006) Surfactant protein D regulates chemotaxis and degranulation of human eosinophils. Clin Exp Allergy 36:1566–1574
Spoorenberg SM, Vestjens SM, Rijkers GT, Meek B, van Moorsel CH, Grutters JC, Bos WJ (2017) YKL-40, CCL18 and SP-D predict mortality in patients hospitalized with community-acquired pneumonia. Respirology 22:542–550
Patyk I, Rybacki C, Kalicka A, Rzeszotarska A, Korsak J, Chciałowski A (2019) Simvastatin therapy and bronchoalveolar lavage fluid biomarkers in chronic obstructive pulmonary disease. Adv Exp Med Biol 1150:43–52
Okazaki S, Murai H, Kidoguchi S, Nomura E, Itoh N, Hashimoto N, Hamada T, Kawakita A, Yasutomi M, Ohshima Y (2017) The biomarker salivary SP-D may indicate small airway inflammation and asthma exacerbation. J Investig Allergol Clin Immunol 27:305–312
Bräuer L, Kindler C, Jäger K, Sel S, Nölle B, Pleyer U, Ochs M, Paulsen FP (2007) Detection of surfactant proteins A and D in human tear fluid and the human lacrimal system. Investig Ophthalmol Vis Sci 48:3945–3953
Ni M, Tam C, Verma A, Ramphal R, Hawgood S, Evans DJ, Fleiszig SM (2008) Expression of surfactant protein D in human corneal epithelial cells is upregulated by Pseudomonas aeruginosa. FEMS Immunol Med Microbiol 54:177–184
Zhang Z, Abdel-Razek O, Hawgood S, Wang G (2015) Protective role of surfactant protein D in ocular Staphylococcus aureus infection. PLoS ONE 10:e0138597
Che CY, Jia WY, Xu Q, Li N, Hu LT, Jiang N, Lin J, Wang Q, Zhao GQ (2012) The roles of surfactant protein D during Aspergillus fumigatus infection in human corneal epithelial cells. Int J Ophthalmol 5:13–17
Hartshorn KL (2010) Role of surfactant protein A and D (SP-A and SP-D) in human antiviral host defense. Front Biosci (Schol Ed) 2:527–546
Posa A, Paulsen F, Dietz R, Garreis F, Sander R, Schicht M, Sel S, Scholz M, Hammer CM, Bräuer L (2018) Quantification of surfactant proteins in tears of patients suffering from dry eye disease compared to healthy subjects. Ann Anat 216:90–94
Teweldemedhin M, Gebreyesus H, Atsbaha AH, Asgedom SW, Saravanan M (2017) Bacterial profile of ocular infections: a systematic review. BMC Ophthalmol 17:212
Limberg MB (1991) A review of bacterial keratitis and bacterial conjunctivitis. Am J Ophthalmol 112:2s–9s
Pastva AM, Wright JR, Williams KL (2007) Immunomodulatory roles of surfactant proteins A and D: implications in lung disease. Proc Am Thorac Soc 4:252–257
McCormick CC, Hobden JA, Balzli CL, Reed JM, Caballero AR, Denard BS, Tang A, O’Callaghan RJ (2007) Surfactant protein D in Pseudomonas aeruginosa keratitis. Ocul Immunol Inflamm 15:371–379
Huang X, Du W, McClellan SA, Barrett RP, Hazlett LD (2006) TLR4 is required for host resistance in Pseudomonas aeruginosa keratitis. Investig Ophthalmol Vis Sci 47:4910–4916
Subedi D, Vijay AK, Willcox M (2018) Overview of mechanisms of antibiotic resistance in Pseudomonas aeruginosa: an ocular perspective. Clin Exp Optom 101:162–171
Mayer S, Raulf MK, Lepenies B (2017) C-type lectins: their network and roles in pathogen recognition and immunity. Histochem Cell Biol 147:223–237
Hansen SW, Ohtani K, Roy N, Wakamiya N (2016) The collectins CL-L1, CL-K1 and CL-P1, and their roles in complement and innate immunity. Immunobiology 221:1058–1067
Kölble K, Reid KB (1993) The genomics of soluble proteins with collagenous domains: C1q, MBL, SP-A, SP-D, conglutinin, and CL-43. Behring Inst Mitt 93:81–86
Crouch E, Persson A, Chang D, Heuser J (1994) Molecular structure of pulmonary surfactant protein D (SP-D). J Biol Chem 269:17311–17319
Vieira F, Kung JW, Bhatti F (2017) Structure, genetics and function of the pulmonary associated surfactant proteins A and D: The extra-pulmonary role of these C type lectins. Ann Anat 211:184–201
Casals C, Campanero-Rhodes MA, García-Fojeda B, Solís D (2018) The role of collectins and galectins in lung innate immune defense. Front Immunol 9:1998
Arroyo R, Echaide M, Moreno-Herrero F, Perez-Gil J, Kingma PS (2020) Functional characterization of the different oligomeric forms of human surfactant protein SP-D. Biochim Biophys Acta Proteins Proteom 1868:140436
Haagsman HP, White RT, Schilling J, Lau K, Benson BJ, Golden J, Hawgood S, Clements JA (1989) Studies of the structure of lung surfactant protein SP-A. Am J Physiol 257:L421-429
Palaniyar N, Nadesalingam J, Clark H, Shih MJ, Dodds AW, Reid KB (2004) Nucleic acid is a novel ligand for innate, immune pattern recognition collectins surfactant proteins A and D and mannose-binding lectin. J Biol Chem 279:32728–32736
Persson A, Chang D, Crouch E (1990) Surfactant protein D is a divalent cation-dependent carbohydrate-binding protein. J Biol Chem 265:5755–5760
McIntosh JC, Swyers AH, Fisher JH, Wright JR (1996) Surfactant proteins A and D increase in response to intratracheal lipopolysaccharide. Am J Respir Cell Mol Biol 15:509–519
Kudo K, Sano H, Takahashi H, Kuronuma K, Yokota S, Fujii N, Shimada K, Yano I, Kumazawa Y, Voelker DR, Abe S, Kuroki Y (2004) Pulmonary collectins enhance phagocytosis of Mycobacterium avium through increased activity of mannose receptor. J Immunol 172:7592–7602
Wu H, Kuzmenko A, Wan S, Schaffer L, Weiss A, Fisher JH, Kim KS, McCormack FX (2003) Surfactant proteins A and D inhibit the growth of Gram-negative bacteria by increasing membrane permeability. J Clin Invest 111:1589–1602
Peterson JC, Durkee H, Miller D, Maestre-Mesa J, Arboleda A, Aguilar MC, Relhan N, Flynn HW Jr, Amescua G, Parel JM, Alfonso E (2019) Molecular epidemiology and resistance profiles among healthcare- and community-associated Staphylococcus aureus keratitis isolates. Infect Drug Resist 12:831–843
Kishore U, Greenhough TJ, Waters P, Shrive AK, Ghai R, Kamran MF, Bernal AL, Reid KB, Madan T, Chakraborty T (2006) Surfactant proteins SP-A and SP-D: structure, function and receptors. Mol Immunol 43:1293–1315
van de Wetering JK, van Eijk M, van Golde LM, Hartung T, van Strijp JA, Batenburg JJ (2001) Characteristics of surfactant protein A and D binding to lipoteichoic acid and peptidoglycan, 2 major cell wall components of gram-positive bacteria. J Infect Dis 184:1143–1151
de Souza GA, Godoy LM, Mann M (2006) Identification of 491 proteins in the tear fluid proteome reveals a large number of proteases and protease inhibitors. Genome Biol 7:R72
Ananthi S, Venkatesh Prajna N, Lalitha P, Valarnila M, Dharmalingam K (2013) Pathogen induced changes in the protein profile of human tears from Fusarium keratitis patients. PLoS ONE 8:e53018
Stapleton F, Carnt N (2012) Contact lens-related microbial keratitis: how have epidemiology and genetics helped us with pathogenesis and prophylaxis. Eye (Lond) 26:185–193
Lin TY, Yeh LK, Ma DH, Chen PY, Lin HC, Sun CC, Tan HY, Chen HC, Chen SY, Hsiao CH (2015) Risk factors and microbiological features of patients hospitalized for microbial keratitis: a 10-year study in a referral center in Taiwan. Medicine (Baltimore) 94:e1905
Fleiszig SM, Zaidi TS, Fletcher EL, Preston MJ, Pier GB (1994) Pseudomonas aeruginosa invades corneal epithelial cells during experimental infection. Infect Immun 62:3485–3493
Fleiszig SM, Lee EJ, Wu C, Andika RC, Vallas V, Portoles M, Frank DW (1998) Cytotoxic strains of Pseudomonas aeruginosa can damage the intact corneal surface in vitro. Clao J 24:41–47
Hanstock HG, Edwards JP, Walsh NP (2019) Tear lactoferrin and lysozyme as clinically relevant biomarkers of mucosal immune competence. Front Immunol 10:1178
Qu XD, Lehrer RI (1998) Secretory phospholipase A2 is the principal bactericide for staphylococci and other gram-positive bacteria in human tears. Infect Immun 66:2791–2797
Haynes RJ, Tighe PJ, Dua HS (1999) Antimicrobial defensin peptides of the human ocular surface. Br J Ophthalmol 83:737–741
Hazlett LD (2007) Bacterial infections of the cornea (Pseudomonas aeruginosa). Chem Immunol Allergy 92:185–194
Fleiszig SM, Kwong MS, Evans DJ (2003) Modification of Pseudomonas aeruginosa interactions with corneal epithelial cells by human tear fluid. Infect Immun 71:3866–3874
Ni M, Evans DJ, Hawgood S, Anders EM, Sack RA, Fleiszig SM (2005) Surfactant protein D is present in human tear fluid and the cornea and inhibits epithelial cell invasion by Pseudomonas aeruginosa. Infect Immun 73:2147–2156
Mun JJ, Tam C, Kowbel D, Hawgood S, Barnett MJ, Evans DJ, Fleiszig SM (2009) Clearance of Pseudomonas aeruginosa from a healthy ocular surface involves surfactant protein D and is compromised by bacterial elastase in a murine null-infection model. Infect Immun 77:2392–2398
Bufler P, Schikor D, Schmidt B, Griese M (2004) Cytokine stimulation by Pseudomonas aeruginosa—strain variation and modulation by pulmonary surfactant. Exp Lung Res 30:163–179
O’Callaghan RJ, McCormick CC, Caballero AR, Marquart ME, Gatlin HP, Fratkin JD (2007) Age-related differences in rabbits during experimental Staphylococcus aureus keratitis. Investig Ophthalmol Vis Sci 48:5125–5131
Hazlett LD (2004) Corneal response to Pseudomonas aeruginosa infection. Prog Retin Eye Res 23:1–30
Alarcon I, Kwan L, Yu C, Evans DJ, Fleiszig SM (2009) Role of the corneal epithelial basement membrane in ocular defense against Pseudomonas aeruginosa. Infect Immun 77:3264–3271
Alarcon I, Tam C, Mun JJ, LeDue J, Evans DJ, Fleiszig SM (2011) Factors impacting corneal epithelial barrier function against Pseudomonas aeruginosa traversal. Investig Ophthalmol Vis Sci 52:1368–1377
Zhou KL, Li X, Zhang XL, Pan Q (2019) Mycobacterial mannose-capped lipoarabinomannan: a modulator bridging innate and adaptive immunity. Emerg Microbes Infect 8:1168–1177
Oberley RE, Ault KA, Neff TL, Khubchandani KR, Crouch EC, Snyder JM (2004) Surfactant proteins A and D enhance the phagocytosis of Chlamydia into THP-1 cells. Am J Physiol Lung Cell Mol Physiol 287:L296-306
Littlejohn JR, da Silva RF, Neale WA, Smallcombe CC, Clark HW, Mackay RA, Watson AS, Madsen J, Hood DW, Burns I, Greenhough TJ, Shrive AK (2018) Structural definition of hSP-D recognition of Salmonella enterica LPS inner core oligosaccharides reveals alternative binding modes for the same LPS. PLoS ONE 13:e0199175
Perez-Garmendia R, de Eguileta L, Rodriguez A, Ramos-Martinez I, Zuñiga NM, Gonzalez-Salinas R, Quiroz-Mercado H, Zenteno E, Hernández ER, Hernández-Zimbrón LF (2020) Interplay between oxidative stress, inflammation, and amyloidosis in the anterior segment of the eye; its pathological implications. Oxid Med Cell Longev 2020:6286105
Hessen M, Akpek EK (2014) Dry eye: an inflammatory ocular disease. J Ophthalmic Vis Res 9:240–250
Graham JE, Moore JE, Jiru X, Moore JE, Goodall EA, Dooley JS, Hayes VE, Dartt DA, Downes CS, Moore TC (2007) Ocular pathogen or commensal: a PCR-based study of surface bacterial flora in normal and dry eyes. Investig Ophthalmol Vis Sci 48:5616–5623
Heimer SR, Evans DJ, Mun JJ, Stern ME, Fleiszig SM (2013) Surfactant protein D contributes to ocular defense against Pseudomonas aeruginosa in a murine model of dry eye disease. PLoS ONE 8:e65797
Wan SJ, Ma S, Evans DJ, Fleiszig SMJ (2020) Resistance of the murine cornea to bacterial colonization during experimental dry eye. PLoS ONE 15:e0234013
Ali MJ, Paulsen F (2019) Surfactant proteins: role in lacrimal drainage disorders. Med Hypotheses 124:35–36
Ali MJ, Kumar NS, Bräuer L, Paulsen F, Schicht M (2018) Expression of surfactant proteins in the human canaliculus: evidence and potential insights into the tear flow dynamics. Ophthalmic Plast Reconstr Surg 34:594–597
Restrepo CI, Dong Q, Savov J, Mariencheck WI, Wright JR (1999) Surfactant protein D stimulates phagocytosis of Pseudomonas aeruginosa by alveolar macrophages. Am J Respir Cell Mol Biol 21:576–585
Haagsman HP, Hogenkamp A, van Eijk M, Veldhuizen EJ (2008) Surfactant collectins and innate immunity. Neonatology 93:288–294
Lim BL, Wang JY, Holmskov U, Hoppe HJ, Reid KB (1994) Expression of the carbohydrate recognition domain of lung surfactant protein D and demonstration of its binding to lipopolysaccharides of gram-negative bacteria. Biochem Biophys Res Commun 202:1674–1680
Bufler P, Schmidt B, Schikor D, Bauernfeind A, Crouch EC, Griese M (2003) Surfactant protein A and D differently regulate the immune response to nonmucoid Pseudomonas aeruginosa and its lipopolysaccharide. Am J Respir Cell Mol Biol 28:249–256
Kuzmenko AI, Wu H, McCormack FX (2006) Pulmonary collectins selectively permeabilize model bacterial membranes containing rough lipopolysaccharide. Biochemistry 45:2679–2685
Zhang J, Xu K, Ambati B, Yu FS (2003) Toll-like receptor 5-mediated corneal epithelial inflammatory responses to Pseudomonas aeruginosa flagellin. Investig Ophthalmol Vis Sci 44:4247–4254
Kowtharapu BS, Murín R, Jünemann AGM, Stachs O (2018) Role of corneal stromal cells on epithelial cell function during wound healing. Int J Mol Sci 19:464
Wang Z, Yang Y, Yang H, Capó-Aponte JE, Tachado SD, Wolosin JM, Reinach PS (2011) NF-κB feedback control of JNK1 activation modulates TRPV1-induced increases in IL-6 and IL-8 release by human corneal epithelial cells. Mol Vis 17:3137–3146
He Y, Crouch E (2002) Surfactant protein D gene regulation. Interactions among the conserved CCAAT/enhancer-binding protein elements. J Biol Chem 277:19530–19537
Seo MJ, Kim JM, Lee MJ, Sohn YS, Kang KK, Yoo M (2010) The therapeutic effect of DA-6034 on ocular inflammation via suppression of MMP-9 and inflammatory cytokines and activation of the MAPK signaling pathway in an experimental dry eye model. Curr Eye Res 35:165–175
Li DQ, Luo L, Chen Z, Kim HS, Song XJ, Pflugfelder SC (2006) JNK and ERK MAP kinases mediate induction of IL-1beta, TNF-alpha and IL-8 following hyperosmolar stress in human limbal epithelial cells. Exp Eye Res 82:588–596
Ohya M, Nishitani C, Sano H, Yamada C, Mitsuzawa H, Shimizu T, Saito T, Smith K, Crouch E, Kuroki Y (2006) Human pulmonary surfactant protein D binds the extracellular domains of Toll-like receptors 2 and 4 through the carbohydrate recognition domain by a mechanism different from its binding to phosphatidylinositol and lipopolysaccharide. Biochemistry 45:8657–8664
Yamazoe M, Nishitani C, Takahashi M, Katoh T, Ariki S, Shimizu T, Mitsuzawa H, Sawada K, Voelker DR, Takahashi H, Kuroki Y (2008) Pulmonary surfactant protein D inhibits lipopolysaccharide (LPS)-induced inflammatory cell responses by altering LPS binding to its receptors. J Biol Chem 283:35878–35888
Wu X, Zhao G, Lin J, Jiang N, Li C, Hu L, Peng X, Xu Q, Wang Q, Li H, Zhang Y (2015) The production mechanism and immunosuppression effect of pulmonary surfactant protein D via toll like receptor 4 signaling pathway in human corneal epithelial cells during Aspergillus fumigatus infection. Int Immunopharmacol 29:433–439
Dziarski R, Gupta D (2005) Staphylococcus aureus peptidoglycan is a toll-like receptor 2 activator: a reevaluation. Infect Immun 73:5212–5216
Sun Y, Hise AG, Kalsow CM, Pearlman E (2006) Staphylococcus aureus-induced corneal inflammation is dependent on Toll-like receptor 2 and myeloid differentiation factor 88. Infect Immun 74:5325–5332
Watson A, Madsen J, Clark HW (2020) SP-A and SP-D: dual functioning immune molecules with antiviral and immunomodulatory properties. Front Immunol 11:622598
Pandit H, Madhukaran SP, Nayak A, Madan T (2012) SP-A and SP-D in host defense against fungal infections and allergies. Front Biosci (Elite Ed) 4:651–661
El-Deek SE, Makhlouf HA, Saleem TH, Mandour MA, Mohamed NA (2013) Surfactant protein D, soluble intercellular adhesion molecule-1 and high-sensitivity C-reactive protein as biomarkers of chronic obstructive pulmonary disease. Med Princ Pract 22:469–474
Wang K, Ju Q, Cao J, Tang W, Zhang J (2017) Impact of serum SP-A and SP-D levels on comparison and prognosis of idiopathic pulmonary fibrosis: a systematic review and meta-analysis. Medicine (Baltimore) 96:e7083
Principe S, Benfante A, Battaglia S, Maitland Van Der Zee AH, Scichilone N (2021) The potential role of SP-D as an early biomarker of severity of asthma. J Breath Res 15:041001
Shu LH, Lu Q, Han LY, Dong GH (2015) SP-D, KL-6, and HTI-56 levels in children with mycoplasma pneumoniae pneumonia. Int J Clin Exp Pathol 8:11185–11191
Uhliarova B, Kopincova J, Adamkov M, Svec M, Calkovska A (2016) Surfactant proteins A and D are related to severity of the disease, pathogenic bacteria and comorbidity in patients with chronic rhinosinusitis with and without nasal polyps. Clin Otolaryngol 41:249–258
Leth-Larsen R, Garred P, Jensenius H, Meschi J, Hartshorn K, Madsen J, Tornoe I, Madsen HO, Sørensen G, Crouch E, Holmskov U (2005) A common polymorphism in the SFTPD gene influences assembly, function, and concentration of surfactant protein D. J Immunol 174:1532–1538
Heidinger K, König IR, Bohnert A, Kleinsteiber A, Hilgendorff A, Gortner L, Ziegler A, Chakraborty T, Bein G (2005) Polymorphisms in the human surfactant protein-D (SFTPD) gene: strong evidence that serum levels of surfactant protein-D (SP-D) are genetically influenced. Immunogenetics 57:1–7
Shakoori TA, Sin DD, Bokhari SN, Ghafoor F, Shakoori AR (2012) SP-D polymorphisms and the risk of COPD. Dis Markers 33:91–100
Deng YQ, Tao ZZ, Kong YG, Xiao BK, Chen SM, Xu Y, Wang Y, He Q (2009) Association between single nucleotide polymorphisms of surfactant protein D and allergic rhinitis in Chinese patients. Tissue Antigens 73:546–552
Liu J, Li G, Li L, Liu Z, Zhou Q, Wang G, Chen D (2017) Surfactant protein-D (SP-D) gene polymorphisms and serum level as predictors of susceptibility and prognosis of acute kidney injury in the Chinese population. BMC Nephrol 18:67
Sorensen GL, Hoegh SV, Leth-Larsen R, Thomsen TH, Floridon C, Smith K, Kejling K, Tornoe I, Crouch EC, Holmskov U (2009) Multimeric and trimeric subunit SP-D are interconvertible structures with distinct ligand interaction. Mol Immunol 46:3060–3069
Shrive AK, Tharia HA, Strong P, Kishore U, Burns I, Rizkallah PJ, Reid KB, Greenhough TJ (2003) High-resolution structural insights into ligand binding and immune cell recognition by human lung surfactant protein D. J Mol Biol 331:509–523
Watson A, Sørensen GL, Holmskov U, Whitwell HJ, Madsen J, Clark H (2020) Generation of novel trimeric fragments of human SP-A and SP-D after recombinant soluble expression in E. coli. Immunobiology 225:151953
Arroyo R, Kingma PS (2021) Surfactant protein D and bronchopulmonary dysplasia: a new way to approach an old problem. Respir Res 22:141
Acknowledgements
We are grateful for the contributions of all the authors and suggestions from our colleagues.
Funding
No funding sources were required for the production of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the work. XH searched the related references and drafted the full manuscript. XZ and ZZ ensured the logic and rationality of the manuscript. All the authors commented on the previous manuscript and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hou, X., Zhang, X. & Zhang, Z. Role of surfactant protein-D in ocular bacterial infection. Int Ophthalmol 42, 3611–3623 (2022). https://doi.org/10.1007/s10792-022-02354-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-022-02354-x