Abstract
Purpose
To determine the impact of failed ab-interno trabeculectomy on the postoperative outcome of subsequent XEN45 gel stent (Allergan, CA, USA) implantation in pseudophakic eyes.
Methods
In this retrospective single-center study, we included 60 pseudophakic eyes from 60 participants who underwent XEN45 gel stent implantation. Thirty eyes each underwent primary stent implantation (control group) or had previously undergone a failed ab-interno trabeculectomy (trabectome group). The groups were matched at a 1:1 ratio based on the following criteria: preoperative and maximum Intraocular pressure (IOP), preoperative medication score, cup/disk-ratio, follow-up time, best-corrected visual acuity at baseline, age, and the proportion of patients classified as primary open angle glaucoma or exfoliation glaucoma. We defined a successful surgery by the following three scores: an IOP reduction > 20% and IOP at the longest follow-up < 21 mmHg (Score A) or < 18 mmHg (Score B) or IOP ≤ 15 mmHg and an IOP reduction ≥ 40% (Score C). One open conjunctival revision was allowed in all scores, and a repeat surgery was considered a failure.
Results
Following an average follow-up period of 22 ± 12 months, we observed a mean IOP reduction of 38%, from 23.5 ± 5.2–14.5 ± 5.0 mmHg. Comparative analyses between the groups did not reveal a significant difference in the postoperative IOP, postoperative medication score, side effects, revision rate, repeat surgery rate, or success rate.
Conclusions
Trabectome is a viable first-line procedure for medically uncontrolled glaucoma before filtering ab-interno microstent surgery is considered.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In addition to established procedures that are used to treat uncontrolled glaucoma, Microinvasive glaucoma surgery (MIGS), which targets the iridocorneal angle, has been used in routine clinical practice in recent years. trabectome surgery (Microsurgical Technology, Redmond, WA, USA), being just one of them, pursues an ab-interno approach. Thus, it does not require the penetration of the conjunctiva. It facilitates an electroablation of the trabecular meshwork and improves access to the physiological system of aqueous outflow through the Schlemm’s canal [1,2,3,4,5,6,7,8].
Jea et al. [9] postulated that Trabectome surgery is a reasonable choice of primary surgery to treat glaucoma and should be considered before traditional filtering surgery. They demonstrated that in terms of success rates and complications, there is no disadvantage in performing trabeculectomy after a failed trabectome surgery.
In addition, the spectrum of filtering surgery is enhanced through MIGS procedures as well. XEN45 gel stent implantation (Allergan, Dublin, CA, USA) is conducted ab-interno via the anterior chamber through the trabecular meshwork and the scleral wall. Moreover, it targets the formation of a subconjunctival bleb. The implant has a small lumen, which assures a moderate drainage of the aqueous humor into the subconjunctival space with minimal side effects, such as hypotony. Several researchers have reported on their favorable safety profile, along with the promising IOP-lowering potential [10,11,12,13,14,15,16].
More recently, a comparative analysis between pseudophakic eyes that underwent prior trabeculectomy and a matched pseudophakic control group demonstrated that a failed trabeculectomy does not affect the outcome of XEN gel stent implantation [17]. However, there is no evidence for the viability of the aforementioned procedure after a failed ab-interno trabeculectomy. Therefore, we compared the outcomes of XEN45 gel stent implantation of two matched groups comprising patients with pseudophakia who had either undergone a previous failed trabectome surgery or had undergone primary stent implantation.
Methods
Study design and patients
This single-center retrospective study was based on the data acquired from the Department of Ophthalmology, St. Martinus-Krankenhaus Düsseldorf, Germany. The retrospective study protocol and data accumulation were conducted with the approval of the Institutional Review Board (Ethik und Kommission Klinische Studien, Dernbacher Gruppe Katharina Kasper, Germany). We adhered to all tenets of the declaration of Helsinki. For the Trabectome group, we reviewed our database and identified patients who underwent secondary stent implantation after a failed ab-interno trabeculectomy from 2015–2020. We excluded patients with a history of previous eye surgery, including trabeculectomy, deep sclerectomy, iStent inject implantation (Glaukos, CA, USA), cyclophotocoagulation, vitrectomy, canaloplasty, and selective laser trabeculoplasty. We also excluded those with a follow-up < 6 months. Performing trabectome surgery mostly as a combined procedure the majority of patients receiving XEN stent surgery after trabecome surgery were pseudophakic. Therefore, the small group of phakic patients who received secondary XEN Gel Stent implantation were excluded from the study to maintain group homogeneity.
The inclusion criteria for the control group were as follows: (i) no history of previous eye surgery, other than cataract surgery, (ii) absence of concomitant eye disease, such as neovascular glaucoma and uveitis, and (iii) follow-up data of at least 6 months.
The eligible patients were matched with those who had undergone ab-interno trabeculectomy at a 1:1 ratio, based on the following criteria: preoperative IOP, maximum known preoperative IOP, preoperative medication score, cup/disk-ratio, follow-up time, best-corrected visual acuity (BCVA) at baseline, and age. Moreover, we matched the proportion of patients classified as Exfoliation glaucoma (XFG) between the groups. If both eyes of a patient were eligible, we included the eye with a longer follow-up.
The IOP was assessed by Goldmann applanation tonometry. We collected a maximum of three IOP measurements, prior to the surgery, and averaged them to evaluate the baseline IOP. The medication score comprised the number of IOP—lowering medication classes administered at baseline and follow-up. The BCVA was measured using standard Snellen charts.
Surgical technique
XEN45 gel stent implantation was performed according to procedures described in previous studies [10, 17]. Initially, mitomycin C (0.1 mg/mL) was injected under the conjunctiva of the upper nasal quadrant, at a distance of 6 mm from the limbus. Following a temporal paracentesis and paracentesis at the 5 or 7 o’clock position, and anterior chamber stabilization using viscoelastic substance, the stent was placed via its injector device. The apex of the injector was driven through the trabecular meshwork and sclera, at a distance of 3 mm from the limbus. The stent was then injected under the conjunctiva, and the injector was removed. The position of the stent was confirmed via gonioscopy. Moreover, the viscoelastic substance was removed from the anterior chamber by irrigation. The aim of surgery was to regulate the IOP without using anti-glaucomatous medications.
Therefore, all patients, without sufficiently reduced postoperative IOP, underwent surgical revision. Instead of needling, the patients were treated via an open conjunctival approach [10, 18]. Following the incision of the conjunctiva at the limbus, the stent was prepared. Following the removal of the scar tissues, the conjunctiva was refixated at the limbus with two absorbable 9.0 sutures.
The patients were subjected to a standardized postoperative topical therapy, including an antibiotic ointment (Floxal AS, Bausch & Lomb, Frankfurt, Germany) and steroid ointment (Ultracortenol AS, Agepha, Senec, Slovakia) thrice a day, the dose was tapered over 4 weeks. Previously prescribed topical anti-glaucomatous medications were discontinued.
Outcome measurement
Changes in the IOP and medication scores at the longest follow-up examination were the primary clinical endpoints. These outcomes were further defined as success or failure by three separate scores. According to scores A and B, an absolute IOP < 21 mmHg or < 18 mmHg at the follow-up examination and a postoperative IOP reduction > 20%, respectively, qualified for success. The aforementioned scores were chosen based on the tube versus trabeculectomy study [19]. In contrast, the criteria for Score C were an absolute IOP ≤ 15 mmHg and a postoperative IOP reduction ≥ 40%, based on the criteria of the World Glaucoma Association [20]. In all scores, one open conjunctival revision was allowed. Repeat surgeries, including an additional glaucoma surgery other than open conjunctival revision was considered a failure in all scores.
Statistical analyses
We performed the statistical analyses using SPSS (Version 24.0, IBM Corp. Armonk, NY, USA) and the statistical programming language R V3.2.2 (R Foundation for Statistical Computing, Vienna, Austria). We compared the outcome measurements between the trabectome group and the control group via a Mann–Whitney U-test and Fisher’s exact test. Moreover, we conducted a log-rank test and visualized the differences using Kaplan–Meier curves. The threshold for statistical significance was defined as p < 0.05.
Results
We identified a total of 751 eyes of 581 patients, with 81 (11%) patients undergoing secondary XEN45 gel stent implantation after a failed ab-interno trabeculectomy. Of these patients, 76 (94%) and five (6%) patients were pseudophakic and phakic, respectively. We eventually retained 30 eyes of 30 patients in the trabectome group, of which 16 (53%) eyes were classified as Primary open angle glaucoma (POAG), 14 (47%) were classified as XFG. Standalone Trabectome surgery and combined surgery with phacoemulsification or phacoemulsification and trabecular aspiration surgery were performed in 11 (37%), 13 (43%), and six eyes (20%), respectively [21,22,23]. The mean latency between primary ab-interno trabeculectomy and XEN Gel stent implantation was 3.2 ± 1.9 years.
Of the 380 pseudophakic eyes in the control group, 108 eyes of 108 patients met the inclusion criteria. After matching 30 eyes of 30 patients were included in the control group, with proportions of eyes with POAG and XFG similar to those in the Trabectome group. Table 1 summarizes the baseline data.
Following an average follow-up of 22 ± 12 months, we observed a mean IOP reduction of 38%, from 23.5 ± 5.2–14.5 ± 5.0 mmHg. Moreover, the mean medication score reduced by 84%, from 2.5 ± 1.1–0.4 ± 0.8 mmHg in the entire cohort.
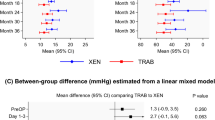
The comparative analysis between the trabectome and control groups did not reveal any significant difference in the postoperative IOP, postoperative medication score, revision rate, repeat surgery rate, or success rate (Table 2).
Side effects in the trabectome and control groups included self-limited intraoperative subconjunctival bleeding and choroidal effusion because of transient hypotony in one and two patients, respectively. There were no severe side effects, such as retinal detachment, leakage, blebitis, and endophthalmitis, in either groups (Table 3).
The Kaplan–Meier curves showing the comparison of success rates between the two groups according to the applied scores displayed corresponding trends, which remained parallel throughout (Fig. 1).
Kaplan–Meier survival curves comparing success rates in the control group and the Trabectome group following XEN45 Gel Stent implantation. Score A: The intraocular pressure (IOP) at follow-up is < 21 mmHg, IOP reduction is > 20%, one revision surgery is allowed, and no repeat surgeries. Score B: The IOP at follow-up is < 18 mmHg, IOP reduction is > 20%, one revision surgery allowed, and no repeat surgeries. Score C: The IOP at follow-up is ≤ 15 mmHg, IOP reduction is ≥ 40%, one revision surgery allowed, and no repeat surgeries
Discussion
We found that a failed trabectome surgery does not affect the outcomes, including postoperative IOP, postoperative medication score, side effects, revision rate, repeat surgery rate, and success rate, of a subsequent XEN45 gel stent implantation. Our findings, which were consistent with those of previous studies, provided further evidence for the efficacy of XEN gel stent implantation in reducing both IOP and medication scores while retaining a favorable safety profile [10,11,12,13,14,15,16].
Our findings confirm that ab-interno surgery in the iridocorneal angle does not interfere with the outcome of a subsequent filtering surgery, affirming the results of the study by Jea et al. [9] This could be attributed to the fact that trabectome surgery does not require the penetration of the conjunctiva [9]. It was postulated that previous conjunctival incisional surgery leads to an increased proliferation of fibroblasts and inflammatory cells of the conjunctiva, which contributes to a higher probability of filtering bleb failure as a result of postoperative inflammation [24]. Our results suggest that, by sparing the conjunctiva, Trabectome surgery allows a more predictable response of IOP after secondary filtering surgery. We conclude that sufficient subconjuctival aqueous drainage can succeed independently from trabecular meshwork excision procedures, which have been carried out previously ab-interno.
To date, there have been no investigations on the histopathological properties of a failed trabectome surgery. Nonetheless, a recent histological examination has investigated two cases with insufficient outcomes after non-ablative ab-interno trabeculotomy using specially designed microhooks [25]. Tsutsui et al. postulated that IOP reduction via microhook ab-interno trabeculotomy occurs either due to a decrease in the resistance of the trabecular meshwork or an addition of an unconventional aqueous outflow path. The authors determined the tissue response via immunohistochemistry and found it not extend beyond the Schlemm’s canal and the collector channels toward structures on the ocular surface.
Previous surgeries, such as trabeculectomy, cataract surgery, vitrectomy, and keratoplasty, increase susceptibility to subconjunctival scarring. This in turn is of crucial importance for the long-term effectiveness of the subsequent filtering surgery, including XEN Gel Stent implantation [26]. However, following prior trabeculectomy, the outcomes of XEN Gel Stent implantation are not inferior to that of primary stent implantation [17]. We validated a similar trend in post-trabectome eyes, which were compared to those that underwent primary XEN Gel Stent implantation.
Among our entire cohort, there was a mean IOP reduction of 38%, a postoperative IOP of 14.5 ± 5.0 mmHg, and a postoperative medication score of 0.4 ± 0.8. While 42% of the patients underwent an open conjunctival revision surgery, 12% underwent a repeat surgery. Our results are concordant with those of previous studies on efficacy of XEN gel stent implantation [10, 11, 27, 28].
The retrospective study design and limited sample size were the major limitations of our study. Additionally, eyes that had undergone trabectome surgery prior to XEN gel stent implantation might have not been initially considered suitable for primary stent implantation. This possibly introduced a selection bias. However, it did not generate inferior results. Therefore, we hypothesized that this did not have a considerable impact on the study findings.
We validated that a failed trabectome surgery does not affect the outcome of subsequent XEN45 gel stent implantation. Therefore, we believe that trabectome surgery is a viable first-line procedure for medically uncontrolled glaucoma before filtering ab-interno microstent surgery is considered.
Despite little or no evidence, we assume that our findings might be applicable to other trabecular meshwork excision procedures, such as goniotome (Microsurgical Technology, Redmond, WA, USA) or Kahook Dual Blade surgery (KDB, New World Medical, Rancho Cucamonga, CA).
References
Minckler DS, Baerveldt G, Alfaro MR, Francis B (2005) Clinical results with the trabectome for treatment of open-angle glaucoma. Ophthalmology 112(6):962–967
Minckler D, Mosaed S, Dustin L, Francis B (2008) Trabectome (trabeculectomy-internal approach) additional experience and extended follow-up. Trans Am Ophthalmol Soc 106(1):149–159
Francis BA, Minckler D, Dustin L, Kawji S, Yeh J, Sit A, Mosaed S, Johnstone M, Trabectome Study G (2008) Combined cataract extraction and trabeculotomy by the internal approach for coexisting cataract and open-angle glaucoma: initial results. J Cataract Refract Surg 34(7):1096–1103
Francis BA, See RF, Rao NA, Minckler DS, Baerveldt G (2006) Ab interno trabeculectomy: development of a novel device (Trabectome) and surgery for open-angle glaucoma. J Glaucoma 15(1):68–73
Ahmed SF, Bhatt A, Schmutz M, Mosaed S (2018) Trabectome outcomes across the spectrum of glaucoma disease severity. Graefes Arch Clin Exp Ophthalmol 256(9):1703–1710
Esfandiari H, Shah P, Torkian P, Conner IP, Schuman JS, Hassanpour K, Loewen N (2019) Five-year clinical outcomes of combined phacoemulsification and trabectome surgery at a single glaucoma center. Graefes Arch Clin Exp Ophthalmol 257(2):357–362
Nazarali SA, Damji KF (2018) Ab interno trabeculectomy with trabectome: outcomes in African American versus Caucasian patients. Can J Ophthalmol 53(4):361–364
Grover DS, Godfrey DG, Smith O, Feuer WJ, Montes de Oca I, Fellman RL (2014) Gonioscopy-assisted transluminal trabeculotomy, ab interno trabeculotomy: technique report and preliminary results. Ophthalmology 121(4):855–861
Jea SY, Mosaed S, Vold SD, Rhee DJ (2012) Effect of a failed trabectome on subsequent trabeculectomy. J Glaucoma 21(2):71–75
Widder RA, Dietlein TS, Dinslage S, Kühnrich P, Rennings C, Rössler G (2018) The XEN45 gel stent as a minimally invasive procedure in glaucoma surgery: success rates, risk profile, and rates of re-surgery after 261 surgeries. Graefes Arch Clin Exp Ophthalmol 256(4):765–771
Schlenker MB, Gulamhusein H, Conrad-Hengerer I, Somers A, Lenzhofer M, Stalmans I, Reitsamer H, Hengerer FH, Ahmed IIK (2017) Efficacy, safety, and risk factors for failure of standalone ab interno gelatin microstent implantation versus standalone trabeculectomy. Ophthalmology 124(11):1579–1588
Reitsamer H, Sng C, Vera V, Lenzhofer M, Barton K, Stalmans I (2019) Two-year results of a multicenter study of the ab interno gelatin implant in medically uncontrolled primary open-angle glaucoma. Graefes Arch Clin Exp Ophthalmol 257(5):983–996
Reitsamer H, Vera V, Ruben S, Au L, Vila-Arteaga J, Teus M, Lenzhofer M, Shirlaw A, Bai Z, Balaram M, Stalmans I (2021) Three-year effectiveness and safety of the XEN gel stent as a solo procedure or in combination with phacoemulsification in open-angle glaucoma: a multicentre study. Acta Ophthalmol. https://doi.org/10.1111/aos.14886
Gabbay IE, Goldberg M, Allen F, Lin Z, Morley C, Pearsall T, Muraleedharan V, Ruben S (2021) Efficacy and safety data for the Ab interno XEN45 gel stent implant at 3 Years A retrospective analysis. Eur J Ophthalmol. https://doi.org/10.1177/11206721211014381
Grover DS, Flynn WJ, Bashford KP, Lewis RA, Duh YJ, Nangia RS, Niksch B (2017) Performance and safety of a new ab interno gelatin stent in refractory glaucoma at 12 months. Am J Ophthalmol 183:25–36
Smith OU, Grover DS, Emanuel ME, Godfrey DG, Fellman RL (2020) XEN gel stent in pediatric glaucoma. J Glaucoma 29(4):e19–e22
Widder RA, Lappas A, Rennings C, Hild M, Dietlein TS, Rößler GF (2020) Primary versus Post-trabeculectomy XEN45 Gel Stent Implantation. J Glaucoma 29(12):1115-1119
Widder RA, Rennings C, Rössler GF (2020) Open conjunctival revision after XEN45 gel stent implantation as a standardized procedure a step by step guide. Ophthalmologe 117(8):806–810
Gedde SJ, Schiffman JC, Feuer WJ, Herndon LW, Brandt JD, Budenz DL (2009) Three-year follow-up of the tube versus trabeculectomy study. Am J Ophthalmol 148(5):670–684
Shaarawy TM, Sherwood MB, Grehn F (2009) Guidelines on design and reporting of glaucoma surgical trials. Kugler, Amsterdam
Widder RA, Dinslage S, Rosentreter A, Jordan JF, Kuhnrich P, Cursiefen C, Lemmen KD, Dietlein TS (2014) A new surgical triple procedure in pseudoexfoliation glaucoma using cataract surgery, trabectome, and trabecular aspiration. Graefes Arch Clin Exp Ophthalmol 252(12):1971–1975
Widder RA, Jordan JF, Kuhnrich P, Luebke J, Roessler GF, Anton A (2018) The effect of additional trabecular aspiration to phacoemulsification and trabectome as a triple procedure in pseudoexfoliation glaucoma: a case-matched study. Int Ophthalmol 38(6):2341–2347
Widder RA, Hild M, Dietlein TS, Kühnrich P, Rennings C, Szumniak A, Lappas A, Roessler GF (2020) Trabectome, trabecular aspiration and phacoemulsification in a triple procedure for treating exfoliation glaucoma A long-term follow-up. Eur J Ophthalmol. https://doi.org/10.1177/1120672120956505
Broadway DC, Grierson I, Hitchings RA (1998) Local effects of previous conjunctival incisional surgery and the subsequent outcome of filtration surgery. Am J Ophthalmol 125(6):805–818
Tsutsui A, Hamanaka T, Manabe K, Kaidzu S, Kumasaka T, Tanito M (2020) Histologic findings of trabecular meshwork and schlemm’s canal after microhook ab interno trabeculotomy. J Glaucoma 30(2):03-2052
Broadway DC, Chang LP (2001) Trabeculectomy, risk factors for failure and the preoperative state of the conjunctiva. J Glaucoma 10(3):237–249
Gillmann K, Bravetti GE, Rao HL, Mermoud A, Mansouri K (2020) Combined and stand-alone XEN 45 gel stent implantation 3-year outcomes and success predictors. Acta Ophthalmol 99(4):e531-e539
Lenzhofer M, Kersten-Gomez I, Sheybani A, Gulamhusein H, Strohmaier C, Hohensinn M, Dick HB, Hitzl W, Eisenkopf L, Sedarous F, Ahmed IIK, Reitsamer HA (2019) Four-year results of a minimally invasive transscleral glaucoma gel stent implantation in a prospective multi-centre study. Clin Exp Ophthalmol 47(5):581–587
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation and data collection was performed by Randolf A. Widder, statistical analysis was performed by David Kiessling. The first draft of the manuscript was written by Randolf A. Widder and David Kiessling, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional review board as well as the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The Institutional Review Board (Ethik und Kommission Klinische Studien, Dernbacher Gruppe Katharina Kasper, Germany) approved the study.
Consent to publish
For this type of study (anonymized data, retrospective analysis), formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kiessling, D., Rennings, C., Hild, M. et al. Impact of failed ab-interno trabeculectomy (trabectome) on subsequent XEN45 gel stent implantation in pseudophakic eyes. Int Ophthalmol 41, 4047–4053 (2021). https://doi.org/10.1007/s10792-021-01977-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-021-01977-w