Abstract
Purpose
In this retrospective case series multicentric study, we assessed the efficiency and safety of micropulse transscleral cyclophotocoagulation (MP-TSCPC) among several types of advanced uncontrolled glaucoma cases. This study was intended to be a real-life study.
Methods
We treated 55 eyes with the Iridex Cyclo G6 device with the MP3 handpiece (IRIDEX Laser Systems) using a standardized protocol. Patients were followed up for a period of one year with an intention-to-treat protocol. Observation points are day 1, week 1, month 1, month 3, month 6, month 9 and year 1 after treatment. The primary outcome is a significant decrease in intra-ocular pressure (IOP) with a threshold of 20% reduction. The secondary outcomes are a reduction in the number of topical molecules needed to control glaucoma progression and the discontinuation of oral acetazolamide.
Results
We observed a significant IOP reduction at every observation point with a mean preoperative IOP of 24.19 mmHg (SEM: 0.96) and mean IOP at final follow-up was 19.50 mmHg (SEM: 1.20). At least 50% of patients reached the significant threshold of 20% IOP reduction at every observation point except for month 6 follow-up. No significant reduction was achieved in the number of topical medications necessary to control glaucoma progression. Mean number of topical medications used at final follow-up is 3.00 (SEM: 0.134). Mean number of topical molecules preoperatively was 3.08 (SEM: 0.138). The discontinuation of oral acetazolamide was obtained with a statistically significant difference (p = 0.003).
Conclusion
Thanks to the design of this study, we add some proofs about the efficiency and the safety of MP-TSCPC for the treatment of uncontrolled advanced glaucoma cases in a real-life practice.
Similar content being viewed by others
Introduction
Micropulse transscleral cyclophotocoagulation (MP-TSCPC) is a relatively new weapon in our therapeutic arsenal for treating refractory advanced glaucoma cases. Previously available treatment possibilities were continuous wave transscleral cyclophotocoagulation (CW-TSCPC) and closed- or open-eye surgical procedures.
MP-TSCPC safety profile as compared to CW-TSCPC has largely been demonstrated [1] which afford us to use it in a much wider variety of indications.
Both MP-TSCPC and CW-TSCPC are designed to target the pigmented epithelium of the ciliary body, thereby reducing aqueous production and obtaining intra-ocular pressure (IOP, TIO) lowering. By using a micropulse protocol, it has been made possible to reach a coagulative threshold in the targeted pigmented epithelium without reaching it in the adjacent tissues (stroma, non-pigmented epithelium, …) we want to preserve and thereby assuming a more tolerable benefits-side effects balance [2]. In histologic studies, only minimal changes were noted in the architecture of the tissues surrounding the ciliary body [3]. Furthermore, to support this, no major anterior segment modification, neither by optical coherence tomography nor by ultrasound biomicroscopy, were reported [4].
In this article, we want to demonstrate the efficiency of a standardized protocol of MP-TSCPC in a real-life practice among a wide variety of indications.
Methods
In this retrospective case series multicentric study (UCL Saint-Luc, Brussels and CHIREC Delta, Brussels), we treated 55 eyes with several types of uncontrolled advanced glaucoma (primary open angle, primary closed angle, juvenile, inflammatory, pigment dispersion, pseudo-exfoliation and neovascular) under multitherapy during the year 2019 (02/2019–12/2019) (Table 1). «Intention to treat» is the study design.
We included patients with advanced glaucoma according to HODAPP classification showing signs of progression on visual field testing [5]. No exclusion criteria were held back.
All patients underwent a preoperative comprehensive ophthalmological examination including anamnesis with review of the glaucoma therapy, best corrected visual acuity (BCVA), slit lamp biomicroscopic examination, IOP measurement with Goldmann applanation tonometry and fundus examination using a 90D lens. No anterior chamber optical coherence tomography (OCT) nor ultrasound biomicroscopy (UBM) were performed.
During follow-up, patients were examined at day 1, week 1, month 1, month 3, month 6, month 9 and month 12. The same examination as preoperatively was performed. The postoperative treatment consisted of a sub-conjunctival injection of betamethasone 0.5 mg/mL and topical dexamethasone 0.1% q.i.d. initially and slowly tapered over 1 month. The usual glaucoma medications were continued unless significant hypotony was observed. This point was left to the appreciation of the physician.
The used device was the Iridex Cyclo G6 with the original MP3 handpiece (IRIDEX Laser Systems). The following parameters were used: power of 2000mW, duty cycle of 31.33% («ON» 0.5 s, «OFF» 1.1 s), duration of 80’’ for 180°, 5 passes per hemisphere, 360° treated at once (avoiding the 3 and 9 o’clock meridian), individual probe for every treated eye [2]. The handpiece was swiped over the bulbar conjunctiva covered with an hydroxypropyl methylcellulose-based ophthalmic viscosurgical device.
The primary outcome of the study is a significant decrease in IOP. The chosen threshold is a decrease of 20% as compared to the preoperative IOP. The secondary outcomes are a decrease in the number of topical medications/molecules necessary to stabilize glaucoma progression and the discontinuation of acetazolamide per os. Observation timings are the following: day 1, week 1, month 1, month 3, month 6, month 9 and year 1.
Continuous variables were summarized by their means and their standard error of the mean (SEM) and qualitative variables as numbers and percentages. Differences in continuous variables (IOP and number of molecules) were compared between groups using an analysis of variance (ANOVA), followed by Sidak tests for multiple comparisons if required. Differences in qualitative variables (acetazolamide orally) were compared between preoperative time and final follow-up using a Mac Nemar exact Chi-square test. Statistical significance was considered when p was < 0.05. All statistical tests were performed using IBM-SPSS (version 27.0) software (IBM Corp, Armonk, NY, USA).
Results
A total of 55 eyes of patients suffering from advanced glaucoma were included in this study. Varied types of glaucoma were included in the study design in a way to be as «real-life practice» as possible. Study design is « intention to treat». The follow-up time lasted 1 year for 10 eyes (18.18%) but we reached 6 months for 30 eyes (54.55%). Mean age preoperatively was 64.19 years (SEM: 2.7). Our cohort consisted of 65.5% males and 34.5% females. Mean preoperative IOP was 24.19 mmHg (SEM: 0.96). Mean number of topical molecules preoperatively was 3.08 (SEM: 0.138). The percentage of our cohort using acetazolamide per os preoperatively was 31.91%.
Based on the difference in IOP between preoperative time and month 1, we can conclude in the absence of correlation between IOP lowering and age (p = 0.159).
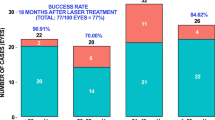
During follow-up, we observe a statistically significant decrease in IOP at every observation time (Figs. 1, 2). There is no statistically significant difference between day 1 postoperatively and other observation points (Fig. 1). Mean IOP at final follow-up is 19.50 mmHg (SEM: 1.20). Mean preoperative IOP was 24.19 mmHg (SEM: 0.96). Except for observation point «6 months», we are able to reach our threshold of 20% IOP reduction in at least 50% of the cases at every observation time (Table 2).
Considering the number of medications used, based on the difference between preoperative time and 1 month postoperatively, there is no correlation with age (p = 0.085).
There is no statistically significant decrease in the number of drops used to control glaucoma progression after MP-TSCPC during our follow-up (Fig. 3). Mean number of topical medications used at final follow-up is 3.00 (SEM: 0.134). Mean number of topical molecules preoperatively was 3.08 (SEM: 0.138).
For the last chosen outcome, the use of acetazolamide orally, we observe a significant decrease in its use (p = 0.003). Among the patients using acetazolamide preoperatively, only 40% still need to use some to control IOP (Fig. 4).
Discussion
Based on the results presented in this study, we can conclude MP-TSCPC is an effective treatment for the control of IOP in uncontrolled advanced glaucoma cases. The design of this study was intended to be as real life as possible (multicentric, intention to treat, several types of glaucoma included) which makes it interesting for physicians in their own practice.
Up until one year after treatment (the end of our follow-up period), we can assert the efficiency of our treatment. We demonstrate, with this procedure, a significant reduction in IOP in advanced uncontrolled glaucoma cases that usually require open-eye surgical procedure. More than half of the patients included reach 20% reduction in IOP after one session of MP-TSCPC at every observation point. These results meet the ones produced by several other studies. Nguyen et al. applied the treatment to several types of refractory glaucoma cases and obtained similar results concerning IOP lowering (20% IOP lowering obtained in 76.8% of the treated eyes) at 12 months follow-up [6]. Zaarour et al. obtained 20% IOP lowering in 56.7% of their patients at 1-year follow-up [2].
Unfortunately, due to the size of our cohort, we were not able to produce evidence about the correlation between response in IOP lowering and glaucoma type nor glaucoma severity. Some studies show slightly better results concerning IOP lowering after MP-TSCPC [7]. These are not comparable with ours in terms of treated population given only primary open-angle glaucoma patients were included. As Tan et al. reported, neovascular glaucoma patients show a higher failure rate [8]. Thus, glaucoma type probably influences response in terms of IOP lowering to MP-TSCPC.
An interesting fact, which was only rarely discussed before, is the following: statistically, the response at day one after treatment is predictive of long-term response. Tan et al. came to the same conclusion concerning this point [8]. Only one patient in our cohort underwent several sessions of MP-TSCPC and always failed to respond. Each time, he was unresponsive from the first day. From this single observation, we would be tempted to conclude that an unresponsive patient to a first trial won’t respond to others. Although Nguyen et al. reported successful retreatment in several patients [6]. To note, Nguyen et al. used an other setting concerning the power when retreatment was performed. It was increased up to 3000 mW.
Correlation can be made between preoperative IOP and response in terms of IOP lowering to MP-TSCPC. Pearson’s correlation coefficient at observation points month 1 and month 6 show moderate-to-high correlation (0.452 and 0.486 respectively). Our analysis is statistically significant for month 1 (p = 0.002) and significant for month 6 (p = 0.006) (Figs. 5, 6). The higher the preoperative IOP, the best result in IOP reduction is to be expected after micropulse cyclophotocoagulation. Aquino et al. also came to the conclusion of better predictability after MP-TSCPC than CW-TSCPC [1].
We failed to demonstrate a statistically significant decrease in the number of topical medications used to lower IOP after MP-TSCPC. Two main reasons may be moved forward: no clear protocol to discontinue medications and the advanced cases included in our study. Zaarour and colleagues, who demonstrated a significant decrease in the number of molecules used, also included moderate cases of glaucoma [2]. Nguyen et al., who came to the same conclusion of drop reduction, did not mention the severity of the glaucoma cases included [6]. Thus, comparison cannot be made. The reduction of glaucoma medications to lower IOP is an outcome with perspectives for the future. Reduction of Ocular Surface Disease, pharmacoeconomic concern, improved compliance to treatment, ….
The use of oral acetazolamide is significantly reduced in a population that underwent MP-TSCPC. The contradiction between this result and the result obtained concerning the other secondary outcome lies probably in the benefits-side effects balance of systemic drug administration as compared with topical therapy. Zaarour et al. published in 2018 similar results concerning discontuniation of oral acetazolamide on a comparable cohort [2]. Interesting fact, we observe an increase in the use of acetazolamide among patients that were not using before MP-TSCPC (Fig. 4). This was in most cases a temporary measure to control IOP spikes.
Classical adverse effect of this kind of procedure is a mild anterior chamber inflammation [2]. We observed only very few serious adverse reactions. One patient suffered from loss of accommodation. A second from severe intra-ocular inflammation with vitritis and inflammatory epimacular membrane that needed vitrectomy. One of the patients under anti-coagulation suffered from intra-ocular bleeding. At last, we noticed one case of severe Dellen effect, spontaneously recovering under intensive cornea hydration.
The classical technical difficulty encountered with the positioning of the original MP3 probe is now over with the new handpiece developed by Iridex. It gives a better access to the sclera with a better oriented laser beam. Better results, thanks to diminished fluctuation in probe positioning, are to be expected in the future.
The main bias of our study lies probably in the size of our cohort and the design of our study. The retrospective and non-randomized character may lead to selection bias as individual characteristics of the treated population may affect treatment effect [9]. So, these results probably require wider cohorts to confirm ours.
The design of the study is also an advantage. As we said before, it is as real-life practice as possible which makes it interesting for a practicing physician in its own office.
Conclusion
One more time, thanks to this article, we add some proofs about the efficiency and the safety of this kind of procedures. Micropulse instead of continuous wave protocol makes cyclodestructive procedures much more relevant in our therapeutic arsenal against glaucoma. It could be used as first-line treatment in advanced uncontrolled glaucoma cases to gain some time before open-eye surgical procedures with their well-known complications and difficult follow-up period. A not insignificant advantage during COVID-19 pandemic situation with frequent periods of postponed non-urgent eyecare procedures.
Availability of data and material
Our gros data and the statistical analysis are available if required.
Code availability
All statistical tests were performed using IBM-SPSS (version 27.0) software (IBM Corp, Armonk, NY, USA).
References
Aquino MC, Barton K, Tan A, Sng C, Li X, Loon SC, Chew PT (2015) Micropulse versus continuous wave transscleral diode cyclophotocoagulation in refractory glaucoma: a randomized exploratory study. Clin Exp Ophtalmol. 43(1):40–46
Zaarour K, Abdelmassih Y, Arej N, Cherfan G, Tomey K, Khoueir Z (2019) Outcomes of micropulse transscleral3 cyclophotocoagulation in uncontrolled glaucoma patients. J Glaucoma 28(3):270–275
Maslin J, Chen P, Noecker RJ (2016) Comparison of acute histological changes in human cadaver eyes after micropulse and continuous wave transscleral cyclophotocoagulation [Abstract]. In: 26th annual meeting of the American Glaucoma Society, Fort Lauderdale, FL
Amoozgar B, Phan EN, Lin SC et al (2017) Update on ciliary body laser procedures. Curr Opin Ophthalmol 28:181–186
Hodapp E, Parrish RK, Anderson DR (1993) Clinical decisions in glaucoma. The CV Mosby Co, St Louis, pp 52–61
Nguyen AT, Maslin J, Noecker RJ (2020) Early results of micropulse transscleral cyclophotocoagulation for the treatment of glaucoma. Eur J Ophthalmol 30(4):700–705
Toyos M, Toyos R (2016) Clinical outcomes of micropulse transscleral cyclophotocoagulation in moderate to severe glaucoma. J Clin Exp Ophthalmol 7:6
Tan AM, Chockalingam M, Aquino MC et al (2010) Micropulse transscleral diode laser cyclophotocoagulation in the treatment of refractory glaucoma. Clin Exp Ophthalmol 38:266–272
Sanchez F, Peirano-Bonomi J, Brossard Barbosa N, Khoueir Z, Grippo T (2020) Update on micropulse transscleral cyclophotocoagulation. J Glaucoma 29:598–603
Funding
No particular funding was required for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declares that they have no competing interests with IRIDEX Laser Systems.
Ethical approval
Not applicable because of the retrospective character of our study and the anonymized data.
Consent to participate
Not applicable because of the retrospective character of our study and the anonymized data.
Consent to publication
Not applicable because of the retrospective character of our study and the anonymized data.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Laruelle, G., Pourjavan, S., Janssens, X. et al. Real-life experience of micropulse transscleral cyclophotocoagulation (MP-TSCPC) in advanced and uncontrolled cases of several glaucoma types: a multicentric retrospective study. Int Ophthalmol 41, 3341–3348 (2021). https://doi.org/10.1007/s10792-021-01896-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-021-01896-w