Abstract
Aim
To evaluate the neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR) in idiopathic epiretinal membrane (IERM) patients, and their relations with visual acuity.
Method
Fifty-seven IERM and 51 control patients were included. All patients underwent comprehensive ophthalmological examination and complete blood count tests, and NLR and PLR values were calculated. Patients with IERM were compared with the control group, and associations with visual prognosis were evaluated. These ratios’ cut-off values for IERM were also calculated
Results
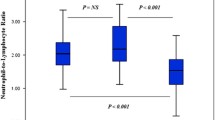
NLR values were statistically significantly higher in the IERM group than in the control group (p = 0.001). No significant difference was observed between the IERM and control groups in terms of PLR (p = 0.43). No significant correlation was determined between visual acuity and NLR or PLR (r = 0.05, p = 0.66; and r = 0.18, p = 0.16, respectively). The cut-off value for NLR was 1.91.
Conclusion
Patients with IERM showed significantly increased NLR compared to control subjects suggesting that IERM patients may be prone to have high NLR values.


Similar content being viewed by others
References
Hillenkamp J, Saikia P, Herrmann WA et al (2007) Surgical removal of idiopathic epiretinal membrane with or without the assistance of indocyanine green: a randomised controlled clinical trial. Graefes Arch Clin Exp Ophthalmol 245(7):97979
Bu SC, Kuijer R, Li XR et al (2014) Idiopathıc epiretinal membrane. Retina 34(12):2317–2335
Pearlstone AD (1985) The incidence of idiopathic preretinal macular gliosis. Ann Ophthalmol 17(6):378–380
Hiscott PS, Grierson I, McLeod D (1985) Natural history of fibrocellular epiretinal membranes: a quantitative, autoradiographic, and immunohistochemical study. Br J Ophthalmol 69(11):810–823
Joshi M, Agrawal S, Christoforidis JB (2013) Inflamatory mechanisms of idiopathic epiretinal membrane formation. Mediat Inflamm 2013:192582
Kose N, Akın F, Yıldırım T et al (2019) The association between the lymphocyte to monocyte ratio and coronary artery disease severity in patients with stable coronary arter disease. Eur Rev Med Pharmacol Sci 23:2570–2575
Song X, Chen D, Yuan M et al (2018) Total lymphocyte count, neutrophil–lymphocyte ratio and platelet–lymphocyte ratio as prognostic factors in advanced non-small cell lung cancer with chemoradiotherapy. Cancer Manag Res 5(10):6677–6683
Lee YH, Song GG (2018) Neutrophil-to-lymphocyte ratio, mean platelet volume and platelet-to-lymphocyte ratio in Behçet’s disease and their correlation with disease activity: a meta-analysis. Int J Rheum Dis 21(12):2180–2187
Vakili H, Shirazi M, Charkhkar M et al (2017) Correlation of platelet-to-lymphocyte ratio and neutrophil-to-lymphocycte ratio with thrombolysis in myocardial infarction frame count in ST-segment elevation myocardial infarction. Eur J Clin Investig 47(4):322–327
Wang Q, Ma J, Jiang Z et al (2018) Prognostic value of neutrophil-to-lymphocycte ratio and platelet-to-lymphocyte ratio in acute pulmonary embolism: a systematic review and meta-analysis. Int Angiol 37(1):4–11
Ozgonul C, Sertoğlu E, Mumcuooglu T et al (2016) Neutrophil to-lymphocyte ratio and platelet-to-lymphocyte ratio as novel biomarkers of primary open-angle glaucoma. J Glaucoma 25(10):e815–e820
Karaca EE, Ozmen MC, Ekici F et al (2014) Neutrophil-to-lymphocyte ratio may predict progression in patients with keratoconus. Cornea 33:1168–1173
Ilhan N, Daglioglu MC, Ilhan O et al (2015) Assessment of neutrophil/lymphocyte ratio in patients with age-related macular degeneration. Ocul Immunol Inflamm 23(4):287–290
Dursun A, Ozturk S, Yucel H et al (2015) Association of neutrophil/lymphocyte ratio and retinal vein occlusion. Eur J Ophthalmmol 25(4):343–346
Mandelcorn E, Khan Y, Javorska L et al (2003) Idiopathic epiretinal membranes: cell type, growth factor expression, and fluorescein angiographic and retinal photographic correlations. Can J Ophthalmol 38:457–463
Minchiotti S, Stampachiacchiere B, Micera A et al (2008) Human idiopathic epiretinal membranes express NGF and NGF receptors. Retina 28:628–637
Bu SC, Kuijer R, van der Worp RJ et al (2015) Immunohistochemical evaluation of idiopathic epiretinal membranes and in vitro studies on the effect of TGF-b on Muller cells. Investig Ophthalmol Vis Sci 56:6506–6514
Kanda A, Noda K, Hirose I et al (2019) TGF-B-SNAIL axis induces Müller glial-mesenchymal transition in the pathogenesis of idiopathic epiretinal membrane. Sci Rep 9:673
Iannetti L, Accorinti M, Malagola R et al (2011) Role of the intravitreal growth factors in the pathogenesis of idiopathic epiretinal membrane. Investig Ophthalmol Vis Sci 52:5786–5789
Dikkaya F, Erdur SK, Ozsutcu M et al (2018) The significance of neutrophil-to-lymphocycte ratio in idiopathic epiretinal membrane. Int Ophthalmol 38:1393–1397
Acknowledgements
Approval of the Institutional Review Board (IRB). The study was approved by Karadeniz Technical University, Faculty of Medicine.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article. There is no funding statement.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by Karadeniz Technical University, Faculty of Medicine, Ethic Council on 2019/268.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Uzlu, D., Erdöl, H., Somuncu, A.M. et al. The role of simple inflammatory blood parameters in idiopathic epiretinal membrane patients. Int Ophthalmol 41, 107–112 (2021). https://doi.org/10.1007/s10792-020-01557-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-020-01557-4