Abstract
Purpose
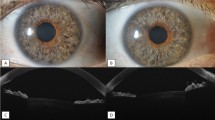
To evaluate the outcomes and complications of deep anterior lamellar keratoplasty (DALK) performed for pediatric keratoconus.
Methods
This retrospective study enrolled 44 consecutive eyes of 39 keratoconus-affected children (≤ 18 years of age). All patients underwent big-bubble DALK from March 2004 to June 2016. The outcome measures included postoperative best spectacle-corrected visual acuity (BSCVA), manifest refraction, keratometry readings, and complications.
Results
The mean participant age was 16.8 ± 1.4 years, and the mean follow-up period was 68.5 ± 39.9 months. Successful big bubble was achieved in 33 eyes (75.0%), while the surgical technique was predescemetic DALK in 11 (25.0%). The mean BSCVA changed from 1.34 ± 0.49 LogMAR preoperatively to 0.24 ± 0.10 LogMAR postoperatively (P < 0.001). The mean keratometry decreased from 59.54 ± 5.17 D preoperatively to 46.23 ± 2.17 D postoperatively (P < 0.001). The complications encountered during the study period were intraoperative Descemet’s membrane perforation (n = 5, 11.4%), the Urrets Zavalia syndrome (n = 1, 2.3%), graft epithelial problems (n = 3, 6.8%), subepithelial graft rejection (n = 5, 11.4%), high intraocular pressure (n = 8, 18.2%), and traumatic wound dehiscence (n = 2, 4.6%). Suture-related complications included premature loosening (n = 13, 29.6%), broken sutures (n = 12, 27.3%), suture-tract vascularization (n = 6, 13.6%), suture-associated abscesses (n = 5, 11.4%), and suture cheese wiring (n = 2, 4.6%). A clear graft was found in 40 eyes (90.9%) at the last follow-up examination.
Conclusion
This study showed promising results with big-bubble DALK in keratoconus-affected children. A frequent and close follow-up with dedicated parental involvement is essential for the early recognition and management of postoperative complications.

Similar content being viewed by others
References
Al Suhaibani AH, Al-Rajhi AA, Al-Motowa S et al (2007) Inverse relationship between age and severity and sequelae of acute corneal hydrops associated with keratoconus. Br J Ophthalmol 91:984–985
Arora R, Jain P, Jain P et al (2016) Results of deep anterior lamellar keratoplasty for advanced keratoconus in children less than 18 years. Am J Ophthalmol 162:191–198
Aasuri MK, Garg P, Gokhle N et al (2000) Penetrating keratoplasty in children. Cornea 19:140–144
Limaiem R, Chebil A, Baba A et al (2011) Pediatric penetrating keratoplasty: indications and outcomes. Transplant Proc 43:649–651
McClellan K, Lai T, Grigg J et al (2003) Penetrating keratoplasty in children: visual and graft outcome. Br J Ophthalmol 87:1212–1214
Huang C, O’Hara M, Mannis MJ (2009) Primary pediatric keratoplasty: indications and outcomes. Cornea 28:1003–1008
Vanathi M, Panda A, Vengayil S et al (2009) Pediatric keratoplasty. Surv Ophthalmol 54:245–271
Lowe MT, Keane MC, Coster DJ et al (2011) The outcome of corneal transplantation in infants, children, and adolescents. Ophthalmology 118:492–497
Feizi S, Javadi MA, Fekri Y (2016) Use of deep anterior lamellar keratoplasty (DALK) for keratoconus: indications, techniques and outcomes. Exp Rev Ophthalmol 11:347–359
Ashar JN, Pahuja S, Ramappa M et al (2013) Deep anterior lamellar keratoplasty in children. Am J Ophthalmol 155:570–574
Buzzonetti L, Ardia R, Petroni S et al (2016) Four years of corneal keratoplasty in Italian paediatric patients: indications and clinical outcomes. Graefes Arch Clin Exp Ophthalmol 254:2239–2245
Harding SA, Nischal KK, Upponi-Patil A et al (2010) Indications and outcomes of deep anterior lamellar keratoplasty in children. Ophthalmology 117:2191–2195
Buzzonetti L, Petrocelli G, Valente P (2012) Big-bubble deep anterior lamellar keratoplasty assisted by femtosecond laser in children. Cornea 31:1083–1086
Elbaz U, Kirwan C, Shen C et al (2018) Avoiding big bubble complications: outcomes of layer-by-layer deep anterior lamellar keratoplasty in children. Br J Ophthalmol 102:1103–1108
Feizi S, Javadi MA, Jamali H et al (2010) Deep anterior lamellar keratoplasty in patients with keratoconus: big-bubble technique. Cornea 29:177–182
Javadi MA, Feizi S, Yazdani S et al (2010) Deep anterior lamellar keratoplasty versus penetrating keratoplasty for keratoconus: a clinical trial. Cornea 29:365–371
Feizi S, Javadi MA, Javadi F et al (2015) Deep anterior lamellar keratoplasty in keratoconic patients with versus without vernal keratoconjunctivitis. J Ophthalmic Vis Res 10:112–117
Reinhart WJ, Musch DC, Jacobs DS et al (2011) Deep anterior lamellar keratoplasty as an alternative to penetrating keratoplasty a report by the american academy of ophthalmology. Ophthalmology 118:209–218
Ardjomand N, Hau S, McAlister JC et al (2007) Quality of vision and graft thickness in deep anterior lamellar and penetrating corneal allografts. Am J Ophthalmol 143:228–235
Feizi S, Javadi MA, Rastegarpour A (2010) Visual acuity and refraction after deep anterior lamellar keratoplasty with and without successful big-bubble formation. Cornea 29:1252–1255
Gonzalez A, Price MO, Feng MT et al (2017) Immunologic rejection episodes after deep anterior lamellar keratoplasty: incidence and risk factors. Cornea 36:1076–1082
Huang OS, Mehta JS, Htoon HM et al (2016) Incidence and risk factors of elevated intraocular pressure following deep anterior lamellar keratoplasty. Am J Ophthalmol 170:153–160
Chaurasia S, Ramappa M (2011) Traumatic wound dehiscence after deep anterior lamellar keratoplasty. J AAPOS 15:484–485
Lee WB, Mathys KC (2009) Traumatic wound dehiscence after deep anterior lamellar keratoplasty. J Cataract Refract Surg 35:1129–1131
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
An informed consent was obtained from the parents or legally authorized representatives of minors who participated in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Feizi, S., Javadi, M.A., Najafi, M. et al. Outcomes of big-bubble deep anterior lamellar keratoplasty for pediatric keratoconus. Int Ophthalmol 40, 1253–1259 (2020). https://doi.org/10.1007/s10792-020-01291-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-020-01291-x