Abstract
Purpose
To evaluate the long-term course of primary angle-closure ocular hypertension and primary open-angle ocular hypertension and possible risk factors for progression to glaucoma.
Methods
A total of 109 eyes of 109 ocular hypertension (OHT) patients with a minimum follow-up period of 5 years having complete ocular/medical records were evaluated. They were classified into primary angle closure or primary open angle based on gonioscopy at baseline. Baseline and review data of Humphrey field analyser, HFA, and Heidelberg retinal tomography, HRT, were recorded. Guided progression analysis (GPA) and univariate Cox regression were used for time to event analysis in identifying progression to glaucoma.
Results
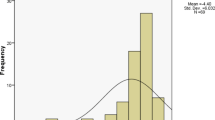
Over a mean follow-up of 12.18 ± 4.8 years, progression to glaucoma was 17.43% (19 eyes), out of whom 5.5% (6 eyes) showed ≥ 3 loci on GPA. Sub-classifying them, progression to primary angle-closure glaucoma was 19.72%, and that of primary open-angle glaucoma was 13.16%. The mean time to progression was 9.34 ± 3.6 years. Significant risk factors included small disc area (≤ 1.99 sq.mm on HRT), requirement of ≥ 2 drugs to maintain target IOP and those engaged in activities yielding a Valsalva effect in daily life. Coronary artery disease (CAD) and systemic use of steroids were associated with increased severity.
Conclusion
Overall progression of OHT to glaucoma was 17.43% over a mean of 9 years, with target IOP of ≤ 18 mm Hg. Patients with smaller discs, CAD, exercising Valsalva type activities and using ≥ 2 glaucoma medications or systemic steroids should be closely monitored.


Similar content being viewed by others
References
Ramakrishnan R, Nirmalan PK, Krishnadas R et al (2003) Glaucoma in a rural population of southern India: the Aravind comprehensive eye survey. Ophthalmology 110:1484–1490
Varma R, Ying-Lai M, Francis BA et al (2004) Prevalence of open-angle glaucoma and ocular hypertension in Latinos: the Los Angeles Latino Eye Study. Ophthalmology 111:1439–1448
Kass MA, Heuer DK, Higginbotham EJ et al (2002) The ocular hypertension treatment study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol Chic Ill 1960 120:701–713 (discussion 829–830)
Sihota R (2011) An Indian perspective on primary angle closure and glaucoma. Indian J Ophthalmol 59:76
Thomas R, Parikh R, Muliyil J et al (2003) Five-year risk of progression of primary angle closure to primary angle closure glaucoma: a population-based study. Acta Ophthalmol Scand 81:480–485
Kim YY, Jung HR (1997) Clarifying the nomenclature for primary angle-closure glaucoma. Surv Ophthalmol 42:125–136
Arnalich-Montiel F, Casas-Llera P, Muñoz-Negrete FJ et al (2009) Performance of glaucoma progression analysis software in a glaucoma population. Graefes Arch Clin Exp Ophthalmol Albrecht Von Graefes Arch Klin Exp Ophthalmol 247:391–397
Kass MA, Gordon MO, Gao F et al (1960) Delaying treatment of ocular hypertension: the ocular hypertension treatment study. Arch Ophthalmol Chic Ill 2010(128):276–287
Gordon MO, Gao F, Beiser JA et al (1960) The 10-year incidence of glaucoma among patients with treated and untreated ocular hypertension. Arch Ophthalmol Chic Ill 2011(129):1630–1631
Thomas R, Parikh R, George R et al (2003) Five-year risk of progression of ocular hypertension to primary open angle glaucoma. A population-based study. Indian J Ophthalmol 51:329–333
Medeiros FA, Sample PA, Weinreb RN (2003) Corneal thickness measurements and visual function abnormalities in ocular hypertensive patients. Am J Ophthalmol 135:131–137
Chauhan BC, McCormick TA, Nicolela MT et al (2001) Optic disc and visual field changes in a prospective longitudinal study of patients with glaucoma: comparison of scanning laser tomography with conventional perimetry and optic disc photography. Arch Ophthalmol 119:1492–1499
Fayers T, Strouthidis NG, Garway-Heath DF (2007) Monitoring glaucomatous progression using a novel Heidelberg Retina Tomograph event analysis. Ophthalmology 114:1973–1980
Vizzeri G, Weinreb RN, Martinez de la Casa JM et al (2009) Clinicians agreement in establishing glaucomatous progression using the Heidelberg retina tomograph. Ophthalmology 116:14–24
Sihota R, Sony P, Gupta V et al (2005) Comparing glaucomatous optic neuropathy in primary open angle and chronic primary angle closure glaucoma eyes by optical coherence tomography. Ophthalmic Physiol Opt J Br Coll Ophthalmic Opt Optom 25:408–415
Hayamizu F, Yamazaki Y, Nakagami T et al (2013) Optic disc size and progression of visual field damage in patients with normal-tension glaucoma. Clin Ophthalmol Auckl NZ 7:807–813
Salvetat ML, Zeppieri M, Tosoni C et al (2016) Baseline factors predicting the risk of conversion from ocular hypertension to primary open-angle glaucoma during a 10-year follow-up. Eye Lond Engl 30:784–795
Landers J, Goldberg I, Graham SL (2002) Analysis of risk factors that may be associated with progression from ocular hypertension to primary open angle glaucoma. Clin Exp Ophthalmol 30:242–247
Gupta V (2010) Constipation-related migraine is linked to the effect of the Valsalva maneuver on the eye: a case report and a mechanistic review. http://www.webmedcentral.com/. Accessed 4 Dec 2016
Sihota R, Dada T, Aggarwal A et al (2007) Does an iridotomy provide protection against narrowing of the anterior chamber angle during Valsalva maneuvre in eyes with primary angle closure. Eye 22:389–393
Sihota R, Konkal VL, Dada T et al (2008) Prospective, long-term evaluation of steroid-induced glaucoma. Eye Lond Engl 22:26–30
Giraud J-M, May F, Manet G et al (2010) Analysis of progression with GPA (guided progression analysis) and mean deviation (MD) indexes of automated perimetry in ocular hypertension and glaucoma. Invest Ophthalmol Vis Sci 51:3997
Renard JPG, Giraud JM, Aryal-Charles N et al (2014) Progression of visual field in patients with ocular hypertension and primary open-angle glaucoma: PROG-F study1 Preliminary results. Invest Ophthalmol Vis Sci 55:5618
Delbarre M, Giraud J, Aptel F et al (2014) Analyze of visual field indices in ocular hypertension: PROG-F3 study. ResearchGate. https://doi.org/10.1111/j.1755-3768.2014.t038.x (Epub ahead of print 1 September 2014)
Rao HL, Kumbar T, Kumar AU et al (2013) Agreement between event-based and trend-based glaucoma progression analyses. Eye 27:803–808
Casas-Llera P, Rebolleda G, Muñoz-Negrete FJ et al (2009) Visual field index rate and event-based glaucoma progression analysis: comparison in a glaucoma population. Br J Ophthalmol 93:1576–1579
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Human and animal rights
The procedures performed in this report involving human subject were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments.
Informed consent
Informed consent was obtained from all the participants of this study.
Rights and permissions
About this article
Cite this article
Sihota, R., Selvan, H., Sharma, A. et al. Long-term evaluation of ocular hypertension with primary angle closure and primary open angles. Int Ophthalmol 39, 803–812 (2019). https://doi.org/10.1007/s10792-018-0872-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-018-0872-8