Abstract
Purpose
To study the indications and variables correlating with graft survival in optical penetrating keratoplasty in a tertiary care hospital in north India.
Participants
All patients who underwent optical keratoplasty, except those undergoing lamellar grafts, tectonic grafts transplants and penetrating keratoplasty done for therapeutic purposes were included in the study. Patients with follow-up less than 2 years were excluded from the study.
Materials and methods
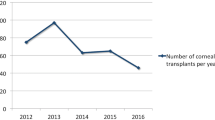
Data were obtained by reviewing the records of 101 patients who underwent optical penetrating keratoplasty from 2008 to 2013 for various indications.
Results
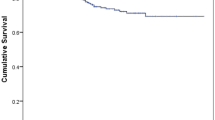
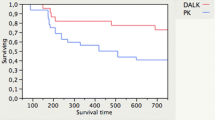
Out of 101 patients who underwent optical penetrating keratoplasty, 71 were males and 30 were females. The mean age of the recipient was 48.53 years with range 1–82 years. The main indications were previous failed graft (29.7%), healed keratitis except HSV (15.8%), pseudophakic or aphakic bullous keratopathy (14.8%), corneal dystrophies/degenerations (12.9%), adherent leucoma (9.9%), post-HSV scars (8.9%), and others like anterior staphyloma, congenital corneal opacities, buphthalmos and keratoconus (7.9%). The graft survival rate was 67.33% at 1-year follow-up and 59.4% at 2-year follow-up. The mean survival time of the grafts was 22.42 months. The mean time for graft failure was 7.12 (±0.9) months.
Conclusion
One- and 2-year survival of grafts at our center is lower as compared to western studies, probably due to higher percentage of poor prognosis indications for surgery and a relative scarcity of excellent-quality donor corneas.







Similar content being viewed by others
References
Population census of India (2011) http://censusindia.gov.in
MOH& FW (NPCB) Rapid Assessment of Avoidable Blindness-India. Report 2006–2007
Siganos CS, Tsiklis NS, Miltsakakis DG, Georgiadis NS, Georgiadou IN, Kymionis GD, Pallikaris IG (2010) Changing indications for penetrating keratoplasty in Greece, 1982–2006: a multicenter study. Cornea 29:372–374
Patel SV, Diehl NN, Hodge DO, Bourne WM (2010) Donor risk factors for graft failure in a 20-year study of penetrating keratoplasty. Arch Ophthalmol 128:418–425
Tan DT, Janardhanan P, Zhou H, Chan YK, Htoon HM, Ang LP et al (2008) Penetrating keratoplasty in Asian eyes, the Singapore corneal transplant study. Ophthalmology 115:975–982
Williams KA, Lowe M, Bartlett C, Kelly TL, Coster DJ (2008) Risk factors for human corneal graft failure within the Australian corneal graft registry. Transplantation 86:1720–1724
Dunn SP, Gal RL, Kollman C, Raghinaru D, Dontchev M, Blanton CL, Holland EJ, Lass JH, Kenyon KR, Mannis MJ, Mian SI, Rapuano CJ, Stark WJ, Beck RW (2014) Writing committee for the Cornea donor study research group. Corneal graft rejection 10 years after penetrating keratoplasty in the cornea donor study. Cornea 33(10):1003–1009
Joshi SA, Jagdale SS, More PD, Deshpande M (2012) Outcome of optical penetrating keratoplasties at a tertiary care eye institute in Western India. Indian J Ophthalmol 60(1):15–21
Mathur V, Parihar JK, Srivastava VK, Avasthi A (2013) Clinical evaluation of Deep Anterior Lamellar Keratoplasty (DALK) for stromal corneal opacities. Med J Armed Forces India 69(1):21–26
Jadeja JN, Patel BD, Shanbhag SS (2013) The grave necessity to make eye bank specular microscopy mandatory in all eye banks in the subcontinent to improve utilization of scarce donor corneas. Indian J Ophthalmol 61(12):711–717
Ang M, Htoon HM, Cajucom-Uy HY, Tan D, Mehta JS (2011) Donor and surgical risk factors for primary graft failure following Descemet’s stripping automated endothelial keratoplasty in Asian eyes. Clin Ophthalmol 5:1503–1508
Tan DT, Dart JK, Holland EJ, Kinoshita S (2012) Corneal transplantation. Lancet 379(9827):1749–1761
Borderie VM, Guilbert E, Touzeau O, Laroche L (2011) Graft rejection and graft failure after anterior lamellar versus penetrating keratoplasty. Am J Ophthalmol 151(6):1024–1029
Keenan TD, Carley F, Yeates D, Jones MN, Rushton S, Goldacre MJ (2011) Trends in corneal graft surgery in the UK. Br J Ophthalmol 95(4):468–472
Bidaut-Garnier M, Monnet E, Prongué A, Montard R, Gauthier AS, Desmarets M, Mariet AS, Ratajczak C, Binda D, Saleh M, Delbosc B (2015) Evolution of corneal graft survival over a 30-year Period and comparison of surgical techniques: a cohort study. Am J Ophthalmol. doi:10.1016/j.ajo.2015.12.014
Figueiredo GS, Jones MN, Krishna Y, Figueiredo FC, Larkin DF, Kaye SB (2015) National health service blood and transplant ocular tissue advisory group (OTAG). Transplant rejection following endothelial keratoplasty and penetrating keratoplasty in the United Kingdom: incidence and survival. Am J Ophthalmol 160(3):416–421
Coster DJ, Lowe MT, Keane MC, Williams KA (2014) Australian corneal graft registry contributors. A comparison of lamellar and penetrating keratoplasty outcomes: a registry study. Ophthalmology 121(5):979–987
Zare M, Javadi MA, Einollahi B, Karimian F, Rafie AR, Feizi S, Azimzadeh A (2012) Changing indications and surgical techniques for corneal transplantation between 2004 and 2009 at a tertiary referral center. Middle East Afr J Ophthalmol 19(3):323–329
Pan Q, Li X, Gu Y (2012) Indications and outcomes of penetrating keratoplasty in a tertiary hospital in the developing world. Clin Exp Ophthalmol 40(3):232–238
Yamamoto S, Shimmura-Tomita M, Satake Y, Shimazaki-Den S, Shimmura S, Shimazaki J (2015) Factors affecting outcomes of repeated penetrating keratoplasty. Nippon Ganka Gakkai Zasshi 119(9):625–631
Varghese AC, Aneeta Jabbar MS, Reesha KR (2011) Outcome of a large series of penetrating keratoplasties in a tertiary eye care centre—a 6 year retrospective study. Kerala J Ophthalmol 23(1):47–53
Fasolo A, Capuzzo C, Fornea M, Franch A, Birattari F, Carito G, Cucco F, Prosdocimo G, Sala M, Delle Noci N, Primavera V, Frigo AC, Grigoletto F, Ponzin D (2011) CORTES Study Group. Risk factors for graft failure after penetrating keratoplasty: 5-year follow-up from the corneal transplant epidemiological study. Cornea 30(12):1328–1335
Writing Committee for the Cornea Donor Study Research Group, Sugar A, Gal RL, Kollman C, Raghinaru D, Dontchev M, Croasdale CR, Feder RS, Holland EJ, Lass JH, Macy JI, Mannis MJ, Smith PW, Soukiasian SH, Beck RW (2015) Factors associated with corneal graft survival in the cornea donor study. JAMA Ophthalmol 133(3):246–254
Wakefield MJ, Armitage WJ, Jones MN, Kaye SB, Larkin DF, Tole D (2015) Prydal J; National Health Service Blood and Transplant Ocular Tissue Advisory Group (OTAG Audit Study 19). The impact of donor age and endothelial cell density on graft survival following penetrating keratoplasty. Br J Ophthalmol. doi:10.1136/bjophthalmol-2015-306871
Funding
No funding was received for this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership or other equity interest; and expert testimony or patent licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies were in accordance with the 1964 Helsinki declaration. For this type of retrospective study, formal consent was not required. The identifying particulars of participants were not revealed in the study.
Rights and permissions
About this article
Cite this article
Arya, S.K., Raj, A., Bamotra, R.K. et al. Indications and graft survival analysis in optical penetrating keratoplasty in a tertiary care center in North India: a 5-year study. Int Ophthalmol 38, 1669–1679 (2018). https://doi.org/10.1007/s10792-017-0641-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-017-0641-0