Abstract
Aim
Multifaceted long COVID caused by SARS-COV-2 affects all populations in the World and takes priority over any other research topics for health care. The purpose of study is to identify physiology-centered risks, prevalence, symptoms and laboratory findings in patients with long COVID in Ukraine.
Methods
A prospective, cohort study was carried out on 332 patients with long COVID after 4 weeks and more after acute infection COVID-19 from Jul 1, 2021, to Jul 1, 2022. Physiology-centered risks related to age, gender, body mass index (BMI), marital status and educational capacity, smoking, lifestyle, physical activity, and laboratory findings (before disease), and symptom distribution were analyzed.
Results
The cohort for the study consisted of 166 females and 107 males (mean age = 42; including young 18 (5.4%) and middle- and old-aged adults 314 (96.4%)). Increased BMI was in 61%, and less physical activity—65%. There were 4 clusters of symptoms related to physical, neurocognitive, pulmonary, and pain conditions. 95% of participants had ≥ 3 symptoms. The most common symptoms were fatigue (90%), muscular pain (85%), anosmia (70%), hair loss (70%), sleep disorders (70%), dyspnea (30%), and brain fog (25%). Among laboratory finding increased CRP (92.6%) and fibrinogen (82.7%) dominated. There are no differences between hospitalized and non-hospitalized patients in distribution symptoms.
Conclusions
The prevalence of long COVID is 23%, and its physiology-centered risk factors are related to age more 38 years, female sex, unhealthy lifestyle, increased BMI, and increased inflammatory markers during COVID-19. The most common symptoms are associated with neurocognitive and pain clusters.
Similar content being viewed by others
Introduction
Recently World Health Organization (WHO) introduced a physiology-centered approach for providing 4P health strategy, Predictive, Preventive, Personalized, and Participatory, which is a new global tactic for understanding how to provide an update in modern health care and prevention of the appearance of lifestyle-associated or chronic diseases (WHO 2018). Modern-day scientific knowledge related to health care is focusing on combating with twenty-first century’s biggest medical problems: the spread and outcomes of the coronavirus (COVID-19) outbreak, as well as the metabolic disorders pandemics. On Sep 22, 2022, despite introduced specific prevention, the number of estimated cases of COVID-19 in the World extends 612 million, with 6.5 million COVID-19-related deaths (Global map of COVID-19, CSSE, JHU). One of the latest new medical illnesses related to COVID-19 which attracts the attention of the global medical community is the condition referred to as “long COVID” (Chen et al. 2022). From October 2021, it associated to introduced by the Centers for Disease Control and Prevention (CDC) and ICD-10 code: U09.9 (post-COVID-19 condition, unspecified, synonym: long COVID) for all healthcare situations (Levine 2022). Previous studies had shown that long COVID is still a major global medical problem related to previous SARS-CoV-2 infections with a wide variety of conditions and its preventive measures are unclear (Aiyegbusi et al. 2021; Abbasi 2022; Bell et al. 2021). Previous studies have been conducted to assess changes in health related to autonomic dysfunction in patients with long COVID (Dani et al. 2021). Moreover, another significant medical and public health challenge in the World for the last decades is the sharply increased distribution of wide-spectrum metabolic disorders (WHO 2021). We theorized that chronic low-grade inflammation associated with metabolic disorders would be an additional pathogenic factor in long COVID. Because of the heterogeneity of evidence, we hypothesized that the population study of the distribution of physiology-centered risk factors could predict the development long COVID and help to promote prevention based on positive lifestyle changes. The assessment of long COVID symptoms prevalence will help to personalize the treatment strategy. Data were generated in a cohort-based study of treated cases of COVID-19 in the Novoyavorivsk district hospital located in the Lviv region in the western part of Ukraine.
Methods
Study design
A prospective, cohort study was carried out at Novoiavorivsk District Hospital named after Yuri Lypa, Lviv region, Ukraine (approval from the ethical committee of author’s university Danylo Halytsky Lviv National Medical University, N3, 22.03.2021).
Participants and data
All participants provided written informed consent to take part. The study was conducted from July 1 2021 until July 1, 2022, according to eligibility criteria of diagnosis U09.9 in patients whose infection was positively notified for a SARS-CoV-2 polymerase chain reaction (PCR) test between January 2021 and June 2022. The exclusion criteria were pregnancy, severe mental or therapeutic illnesses, acute musculoskeletal diseases, orthopedic injuries, and identified cancer.
Measurements
For the detection of participants’ general information about age, sex, body mass index (BMI), diet, marital, educational status, laboratory findings, and cumulative duration of sick leave, the original medical record’s dataset was used. The self-reported survey questionnaires about lifestyle grading into sedentary behavior, moderate- and vigorous-intensive activities, and physical activity based on guidelines of the WHO Global Physical Activity Questionnaire, grading into low, modest, and intensive were used as well (WHO 2018). For the detection of autonomic nervous system (ANS) status in young patients aged 18–27 years, heart rate variability rheoencephalographic recording analysis using RHEO-TEST computer software complex (Kharkiv, Ukraine) was used.
Statistical analysis
Obtained data were imported into an Excel sheet using Statistical Analysis System and visualization program «Statistica 7.0» (StatSoft, Informer Technologies, Inc.) to perform all analyses. Results are expressed as mean ± standard deviation (SD). The descriptive analysis of quantitative variables which represented the central tendency and qualitative variables was formatted in percentages from total numbers and presented using histograms.
Results
General characteristics and lifestyle risk factors
The total number of treated cases of COVID-19 in the Novoiavorivsk District Hospital named after Yuri Lypa for the period from July 1, 2021, to July 1, 2022, was 1980 patients aged 18–92, including 1229 (62%) females and 851 (38%) males. Table 1 reflects the number of distribution patients with COVID-19 during the time of study for which response rates varied between 73.3% and 26.7% for 2021 and 2022, respectively.
The number of patients who died in the hospital was 238 (11%). Despite women being treated in our hospital more frequently, the male patients (65%) died further often.
In the beginning, we included 620 patients of both sexes aged 28–70 years (the average age was 42–45). About 70% of these patients were dependent on oxygen support during treatment. Signs of long COVID regarding the guidelines and criteria of exclusion in the study group were found in 332 out of 620 examinees, which was 53.5%. Among them are 230 (69.2%) females and 102 (30.7%) males.
The follow-up time of participants was from 4 to 50 weeks. The general information, including age, sex, body mass index (BMI), diet, marital, educational, and social status, cumulative duration of sick leave, as well as lifestyle factors (sedentary behavior, moderate or vigorous-intensive activity), grades of physical activity and smoking status of participants in the study group of long COVID are presented in Table 2.
The long COVID was more often diagnosed in patients with increased BMI (61%) in comparison to those with normal or decreased BMI, and who had a sedentary lifestyle and/or low physical activity.
During recognition of ANS status, the signs of sympathetic hyperactivity dysautonomia were in 40% of people in the group aged 18–27 years. Most of them (80%) had a sedentary lifestyle and/ or low physical activity.
Long COVID symptoms and factors influencing on them
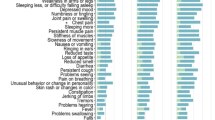
An interesting fact was that 315 examinees (95%) of the total number of patients with long COVID had ≥ 3 somatic or mental health symptoms. The symptoms we observed in our patients can be divided into several clusters: (1) physical; (2) neurocognitive; (3) pulmonary; (4) pain related as well. The core symptoms for physical cluster were fatigue and hair loss; for neurocognitive—brain fog, anosmia, and fear; for pulmonary—dyspnea; for pain-related—muscular pain. The distribution and period differences of these core symptoms are presented in Figs. 1 and 2. The symptoms were more severe in patients who were hospitalized during COVID-19 treatment (Fig. 1) in comparison to non-hospitalized patients during acute infection of SARS-CoV-2 (Fig. 2). The most common long COVID symptoms (about or more than 50% of total cases) with duration more than 2 weeks were anosmia, muscular pain, and hair loss among hospitalized patients during acute infection than in those with hair loss among non-hospitalized patients. Additional common symptoms were problems with concentration and paying attention (25%), trouble with memory and focus (20%), thoughts that can be described as sluggish or fuzzy (20%), and executive functioning problems (20%). There were recognized signs of depression and fear too. Among long COVID study groups’ participants were patients with post-traumatic stress disorder (6%), and one patient had the debut of schizophrenia.
Laboratory findings in the study group’s participants during COVID-19 illness reflect Fig. 3. They were related to increasing D-dimers, C-reactive proteins, fibrinogen levels, changes in white blood cells (WBC, leukopenia at the beginning of the disease, and leukocytosis on day 8–12 of the disease in 84%), increased ESR at the 10th day of the beginning of the disease (69%), increased hematocrit level in patients, who depended of oxygen more than 7 days (81%).
The discussion and conclusions
One of the important topics in modern research is related to the long-term complications after COVID-19 (Soriano et al. 2022). It is described also as long COVID (synonym: post-acute COVID-19 syndrome, long-haul COVID, post-acute sequelae of SARS-CoV-2 infection) and was introduced to MESH on November 30, 2020. Our study was designed to identify the prevalence of long COVID in the Ukrainian population and recognize physiology-centered risk factors and lifestyle changes among these patients. Our study shows that long COVID distribution was detected in 27% of cases from the total number of patients with SARS-CoV-2 infection treated in the Novoiavorivsk District Hospital named after Yuri Lypa. Two-thirds of patients included in the study group with long COVID were treated in hospital in 2021. It could be explained by the appearance of the novel Omicron subvariants of SARS-CoV-2 infections in autumn 2021 which were identified as the leading circulating strains among cases of COVID-19. It increased the new “wave” of the pandemic in the world despite globally introduced specific vaccination, as well as in Ukraine. Another factor is related to wartime in Ukraine. The beginning of wartime on February 24, 2022, connected with the relocation of the population to safe regions, thus, the number of people who sought help for long COVID decreased, esp. after the bombing of the biggest military base in Novoiavorivsk at the March 2022 (The New York Times, March 2022). This is a reason that can explain the difference in the distribution and prevalence of long COVID compared to the results of other scientific groups (Levine 2022; Peter et al. 2022a, b). Our data on persistent symptoms’ distribution and their duration match with reports of Nasserie et al. (2021), and Peter et al. (2022a, b). According to our results about physiology-centered risk factors, long COVID was observed more often among women. Our findings about age differences showed that long COVID is the most common among persons of age groups 62–70 years (67.7%). Another physiology-centered risk factor in patients with long COVID is increased BMI which characterizes overweight obesity. According to the literature overweight and obese people are characterized by chronic low-grade inflammation (Khanna et al. 2022). In addition, long COVID is more often diagnosed in patients, who suffered from diabetes mellitus type 2 and other metabolic disorders, such as hypothyroidism, autoimmune thyroiditis, and allergic diseases. The distribution of physiology-centered risk factors and their impact on the pathogenesis of long COVID were observed by other study groups (Li et al. 2021; Yong 2021; Castanares-Zapatero et al. 2022), thus the interventions related to prevention increased BMI is urgently needed. The negative changes in behavior, such as a sedentary lifestyle or low physical activity previous to COVID-19, were risk factors for long COVID. Smoking is likely another risk factor for long COVID in older adults 38–70 years. In addition to these risk factors, in patients with long COVID aged 18–27 years was dysautonomia which may have been related to severe COVID-19-associated distress (Szabo 2020), and less activity of the parasympathetic nervous system which is related to the development of low-grade inflammation too (Bonaz et al. 2016). The potential COVID-19 treatments around the world have shown that prescription of corticosteroids improved outcomes, including survival, reflects key role of distress in pathogenesis of long COVID and dexamethasone therapy as option for prevention, as well as treatment for long-term infection (Baraniuk 2021).
To sum up, the prevalence of long COVID in Ukrainian population is 23%. The analysis of the dominance of multifaceted symptoms in the study group’s patients with long COVID indicates clusters with neurocognitive, pulmonary, and pain symptoms. The negative changes in laboratory findings related to increased D-dimers, C-reactive proteins, and fibrinogen levels during the COVID-19 acute phase were other risk factors in the development of long COVID. Our results suggest that the problem of recognizing long COVID should be associated with a complex analysis of obtained physiology-centered risk factors and their prevalence. A new strategy concerning the improved lifestyle of the population and metabolic health is important and it will help in the prevention development of long COVID illness.
Limitations
This study has limitations. It was conducted in rapid response to the distribution of long COVID which symptoms were not standardized by definitions or instruments. There was difficulty in comparing the frequency and severity of dysautonomia in all age groups because many adults aged 29–70 years have cardio-vascular diseases; thus, we limited our study to dysautonomia only in 18–27-year-old adults.
Data availability
Enquiries about data availability should be directed to the authors.
References
Abbasi J, The US (2022) Now has a research plan for long COVID—is it enough? JAMA. https://doi.org/10.1001/jama.2022.14536
Aiyegbusi OL, Hughes SE, Turner G, Rivera SC, McMullan C, Chandan JS, Haroon S, Price G, Davies EH, Nirantharakumar K, Sapey E (2021) Symptoms, complications and management of long COVID: a review. J R Soc Med 114(9):428–442. https://doi.org/10.1177/01410768211032850
Baraniuk C (2021) Where are we with drug treatments for covid-19? BMJ. https://doi.org/10.1136/bmj.n1109
Bashkirtsev O, Gaevska V, Zimba O, Sagan V (2021) Biological age estimation based on heart rate variability: А pilot study. Proc Shevchenko Sci Soc Med Sci 65(2):218–239. https://doi.org/10.25040/ntsh2021.02.21
Bell ML, Catalfamo CJ, Farland LV, Ernst KC, Jacobs ET, Klimentidis YC et al (2021) Post-acute sequelae of COVID-19 in a non-hospitalized cohort: Results from the Arizona CoVHORT. PLoS ONE 16(8):e0254347. https://doi.org/10.1371/journal.pone.0254347
Bonaz B, Sinniger V, Pellissier S (2016) Anti-inflammatory properties of the vagus nerve: potential therapeutic implications of vagus nerve stimulation. J Physiol 594(20):5781–5790. https://doi.org/10.1113/JP271539. (Epub 2016 May 1. PMID: 27059884; PMCID: PMC5063949)
Castanares-Zapatero D, Chalon P, Kohn L, Dauvrin M, Detollenaere J, Maertens de Noordhout C, Primus-de Jong C, Cleemput I, Van den Heede K (2022) Pathophysiology and mechanism of long COVID: a comprehensive review. Ann Med 54(1):1473–1487
Chen C, Haupert SR, Zimmermann L, Shi X, Fritsche LG, Mukherjee B (2022) Global prevalence of post COVID-19 condition or long COVID: A meta-analysis and systematic review. J Infect Dis. https://doi.org/10.1093/infdis/jiac136
Dani M, Dirksen A, Taraborrelli P, Torocastro M, Panagopoulos D, Sutton R, Lim PB (2021) Autonomic dysfunction in “long COVID”: rationale, physiology and management strategies. Clin Med (Lond) 21(1):e63–e67. https://doi.org/10.7861/clinmed.2020-0896. (Epub 2020 Nov 26. PMID: 33243837; PMCID: PMC7850225. doi: 10.1080/07853890.2022.2076901)
Global map of COVID-19 by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). https://coronavirus.jhu.edu/map.html
Khanna D, Khanna S, Khanna P, Kahar P, Patel BM (2022) Obesity: a chronic low-grade inflammation and its markers. Cureus 14(2):e22711. https://doi.org/10.7759/cureus.22711
Levine RL (2022) Addressing the Long-term Effects of COVID-19. JAMA. Published online August 03, 2022. https://doi.org/10.1001/jama.2022.14089https://jamanetwork.com/journals/jama/article-abstract/2795139
Li J, Huang DQ, Zou B, Yang H, Hui WZ, Rui F, Yee NTS, Liu C, Nerurkar SN, Kai JCY, Teng MLP, Li X, Zeng H, Borghi JA, Henry L, Cheung R, Nguyen MH (2021) Epidemiology of COVID-19: a systematic review and meta-analysis of clinical characteristics, risk factors, and outcomes. J Med Virol 93(3):1449–1458. https://doi.org/10.1002/jmv.26424. (Epub 2020 Aug 25. PMID: 32790106; PMCID: PMC7436673)
Nasserie T, Hittle M, Goodman SN (2021) Assessment of the frequency and variety of persistent symptoms among patients with COVID-19: a systematic review. JAMA Netw Open 4(5):e2111417. https://doi.org/10.1001/jamanetworkopen.2021.11417
Peter RS, Nieters A, Kräusslich HG, Brockmann SO, Göpel S, Kindle G, Merle U, Steinacker JM, Rothenbacher D, Kern WV, EPILOC Phase 1 Study Group (2022a) Post-acute sequelae of covid-19 six to 12 months after infection: population based study. BMJ 379:e071050. https://doi.org/10.1136/bmj-2022-071050. (PMID: 36229057; PMCID: PMC9557001)
Peter RS, Nieters A, Brockmann SO, Göpel S, Kindle G, Merle U, Wolfers K (2022b) Association of body mass index with general health, working capacity recovered, and post-acute sequelae of COVID-19. Obesity. https://doi.org/10.1002/oby.23611
Soriano JB, Murthy S, Marshall JC, Relan P, Diaz JV, WHO Clinical Case Definition Working Group on Post-COVID-19 Condition (2022) A clinical case definition of post-COVID-19 condition by a Delphi consensus. Lancet Infect Dis 22(4):e102–e107. https://doi.org/10.1016/S1473-3099(21)00703-9. (Epub 2021 Dec 21. PMID: 34951953; PMCID: PMC8691845)
Szabo S (2020) COVID-19: new disease and chaos with panic, associated with stress. Proc Shevchenko Sci Soc Med Sci [internet]. https://doi.org/10.25040/ntsh2020.01.14
WHO (2018) ACTIVE: a technical package for increasing physical activity. World Health Organization, Geneva, 2018. Licence: CC BY-NC-SA 3.0 IGO. ISBN: 9789241514804 9789241514187-eng.pdf (who.int)
Yong SJ (2021) Long COVID or post-COVID-19 syndrome: putative pathophysiology, risk factors, and treatments. Infect Dis (Lond). 53(10):737–754. https://doi.org/10.1080/23744235.2021.1924397. (Epub 2021 May 22. PMID: 34024217; PMCID: PMC8146298)
Acknowledgements
Acknowledgments to Nataliya Ivanchenko, MD (State institution “Lviv Oblast Center for Diseases Control and Prevention of Ministry of Health of Ukraine, Lviv, Ukraine”) for support study.
Funding
The authors have not disclosed any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors have not disclosed any competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Muzyka, I., Yakhnytska, M., Savytska, M. et al. Long COVID prevalence and physiology-centered risks: population-based study in Ukraine. Inflammopharmacol 31, 597–602 (2023). https://doi.org/10.1007/s10787-023-01177-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10787-023-01177-1