Abstract
Introduction
The non-steroid anti-inflammatory drugs (NSAIDs) are among the drugs that can commonly cause injury in the esophagus, such as non-reflux oesophagitis, with important clinical consequences. This injury may be ‘silent’ and therefore often overlooked. Recently, we established that hydrogen sulfide (H2S) is a critical mediator of esophageal mucosal protection and repair. The aim of the study was to determine the effect of naproxen, the most commonly used NSAIDs, on the oesophagus and oesophagogastric junction and its relation with suppression or stimulation of endogenous H2S synthesis during naproxen-induced oesophageal injury.
Methods
Rats were treated with vehicle (control) or naproxen, with or without being subjected to water immersion restricted stress (Takagi et al. Chem Pharm Bul 12:465–472, 1964). Subgroups of rats were pre-treated with an inhibitor of H2S synthesis cystathionine γ-lyase (CSE) or cystathionine β-synthase (CBS), or with the Sodium sulphide (NaHS), which spontaneously generates H2S in solution. Damage of the oesophageal mucosa and oesophagogastric junction was estimated and scored using a histological damage index.
Results
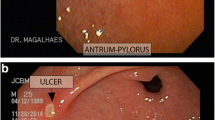
Treatment with naproxen increased the thickness of the corneal and epithelial layers of the oesophagus, as well as producing disorganization of the muscle plate and irregular submucosal oedema. Both injury factors, stress and suppression of H2S synthesis resulted in the development of severe esophagitis and damage to the oesophagogastric junction. The damage was exacerbated by inhibitors of H2S biosynthesis, and attenuated by treatment with NaHS.
Conclusions
Inhibition of endogenous H2S synthesis provides a novel experimental model that can be useful in preclinical studies NSAID-related non-reflux oesophagitis. H2S contributes significantly to mucosal defence in the oesophagus.







Similar content being viewed by others
Abbreviations
- CBS:
-
Cystathionine β-synthase
- CHH:
-
O-carboxymethylhydroxylamine
- CSE:
-
Cystathionine γ-lyase
- EGJ:
-
Oesophagogastral junction
- H2S:
-
Hydrogen sulfide
- HE:
-
Hematoxylin and eosin
- NaHS:
-
Sodium sulfide
- NSAIDs:
-
Non-steroid anti-inflammatory drugs
- PAG:
-
l-propargylglycine
References
Abid S, Mumatz K, Jafri W et al (2005) Pill-induced oesophageal injury: endoscopic features and clinical outcomes. Endoscopy 37:740–744
Almashat SJ, Duan L, Goldsmith JD (2014) Non-reflux oesophagitis: a review of inflammatory diseases of the oesophagus exclusive of reflux oesophagitis. Semin Diagn Pathol 31(2):89–99
Anderson LA, Johnston BT, Watson RP, Murphy SJ, Ferguson HR, Comber H, Murray LJ (2006) Nonsteroidal anti-inflammatory drugs and the oesophageal inflammation—metaplasia–adenocarcinoma sequence. Cancer Res 66(9):4975–4982
Avidan B, Sonnenberg A, Schnell TG, Budiman-Mak E, Sontag SJ (2001) Risk factors of oesophagitis in arthritic patients. Eur J Gastroenterol Hepatol 13(9):1095–1099
Blackler R, Syer S, Bolla M, Ongini E, Wallace JL (2012) Gastrointestinal-sparing effects of novel NSAIDs in rats with compromised mucosal defence. PLoS One 7:e35196
Blackler RW, Gemic B, Manko A, Wallace JL (2014) NSAID-gastroenteropathy: new aspects of pathogenesis and prevention. Curr Opin Gastroenterol 19C:11–16
Bordea MA, Pirvan A, Sarban C, Margescu C, Leucuta D, Samasca G, Miu N (2014) Pill-induced erosive oesophagitis in children. Clujul Med 87(1):15–18
Bula N, Gavriluk E, Zayachkivska O (2014) Animal model of non-reflux oesophagitis via NSAID-induced injury and modification biosynthesis of hydrogen sulfide. Dig Dis Sci 59(8):1651–1652
Chan MV, Wallace JL (2013) Hydrogen sulfide-based therapeutics and gastrointestinal diseases: translating physiology to treatments. Am J Physiol Gastrointest Liver Physiol 305(7):G467–G473
Ecker GA, Karsh J (1992) Naproxen induced ulcerative oesophagitis. J Rheumatol 19(4):646–647
El-Serag HB, Sonnenberg A (1997) Association of oesophagitis and oesophageal strictures with diseases treated with nonsteroidal anti-inflammatory drugs. Am J Gastroenterol 92(1):52–56
Hvid-Jensen F, Pedersen L, Funch-Jensen P, Drewes AM (2014) Proton pump inhibitor use may not prevent high-grade dysplasia and oesophageal adenocarcinoma in Barrett’s oesophagus: a nationwide study of 9,883 patients. Aliment Pharmacol Ther 39:984–991. doi:10.1111/apt.12693
Kadayifci A, Gulsen MT, Koruk M, Savas MC (2004) Doxycycline-induced pill oesophagitis. Dis Oesophagus 17:168–171
Kandulski A, Malfertheiner P (2012) Gastroesophageal reflux disease—from reflux episodes to mucosal inflammation. Nat Rev Gastroenterol Hepatol 9:15–22
Khalaf N, Nguyen T, Ramsey D, El–Serag HB (2014) Nonsteroidal anti-inflammatory drugs and the risk of Barrett’s oesophagus. Clin Gastroenterol Hepatol 12(11):1832–1839
Kikendall JW (2007) Pill-induced oesophagitis. Gastroenterol Hepatol 3(4):275
Kuramoto T, Umegaki E, Nouda S, Narabayashi K, Kojima Y, Yoda Y, Higuchi K (2013) Preventive effect of irsogladine or omeprazole on non-steroidal anti-inflammatory drug-induced oesophagitis, peptic ulcers, and small intestinal lesions in humans, a prospective randomized controlled study. BMC Gastroenterol 13(1):85
Majka J, Rembiasz K, Migaczewski M, Budzynski A, Ptak-Belowska A, Pabianczyk R, Brzozowski T (2010) Cyclooxygenase-2 (COX-2) is the key event in pathophysiology of Barrett’s oesophagus. Lesson from experimental animal model and human subjects. J Physiol Pharmacol 61(4):409
Marlicz W, Loniewski I, Grimes DS, Quigley EM (2014) Nonsteroidal anti-inflammatory drugs, proton pump inhibitors, and gastrointestinal injury: contrasting interactions in the stomach and small intestine. Mayo Clin Proc. doi:10.1016/j.mayocp.2014.07.015
Modlin IM, Hunt RH, Malfertheiner P, Moayyedi P, Quigley EM, Tytgat GN, Moss SF (2009) Diagnosis and management of non-erosive reflux disease—the Vevey NERD Consensus Group. Digestion 80(2):74–88
Mózsik G, Past T, Salam OMA, Kuzma M, Perjési P (2009) Interdisciplinary review for correlation between the plant origin capsaicinoids, non-steroidal antiinflammatory drugs, gastrointestinal mucosal damage and prevention in animals and human beings. Inflammopharmacology 17(3):113–150
Namasivayam V, Murray JA (2013) Drug-induced oesophageal injury. Springer, New York
Nguyen Dang M, Richardson Peter, Hashem B, Serag El (2010) Medications (NSAIDs, statins, proton pump inhibitors) and the risk of oesophageal adenocarcinoma in patients with Barrett’s oesophagus. Gastroenterology 138(7):2260–2266
Nguyen T, Tang Z, Younes M, Alsarraj Ramsey D, Fitzgerald S, El-Serag HB (2015) Oesophageal COX-2 expression is increased in Barrett’s oesophagus, obesity, and smoking. Dig Dis Sci 60(1):65–73. doi:10.1007/s10620-014-3333-x
Panarelli NC (2014) Drug-induced injury in the gastrointestinal tract. Semin Diagn Pathol 31(2):165–175
Pandeya N, Webb PM, Sadeghi S, Green AC, Whiteman DC (2010) Gastro-oesophageal reflux symptoms and the risks of oesophageal cancer: are the effects modified by smoking, NSAIDs or acid suppressants? Gut 59(01):31–38
Rainsford KD (2007) Anti-inflammatory drugs in the 21st century, inflammation in the pathogenesis of chronic diseases. Springer, The Netherlands
Sadeghi S, Bain CJ, Pandeya N, Webb PM, Green AC, Whiteman DC (2008) Aspirin, nonsteroidal anti-inflammatory drugs, and the risks of cancers of the oesophagus. Cancer Epidemiol Biomark Prev 17(5):1169–1178
Saunders WB, Anderson LA, Johnston BT, Watson RP, Murphy SJ, Ferguson HR, Comber H, Murray LJ (2006) Nonsteroidal anti-inflammatory drugs and the oesophageal inflammation-metaplasia-adenocarcinoma sequence. Cancer Res 66(9):4975–4982
Schneider JL, Zhao WK, Corley DA (2015) Aspirin and nonsteroidal anti-inflammatory drug use and the risk of Barrett’s oesophagus. Dig Dis Sci 60(2):436–443. doi:10.1007/s10620-014-3349-2
Souza RF (2007) Molecular mechanisms of acid exposure in Barrett’s oesophagus. Inflammopharmacology 15(3):95–100
Takagi K, Kasuya Y, Watanabe K (1964) Studies on the drugs for peptic ulcer. A reliable method for producing stress ulcer in rats. Chem Pharm Bull 12:465–472
Takeuchi K, Nagahama K (2014) Animal model of acid-reflux oesophagitis: pathogenic roles of acid/pepsin, prostaglandins, and amino acids. Biomed Res Int. doi:10.1155/2014/53259
Voltaggio L, Lam-Himlin D, Limketkai BN, Singhi AD, Arnold CA (2014) Message in a bottle: decoding medication injury patterns in the gastrointestinal tract. J Clin Pathol 67(10):903–912
Wallace JL, Blackler RW, Chan MV, da Silva GJ, Elsheikh W, Flannnigan KL et al (2015) Anti-inflammatory and cytoprotective actions of hydrogen sulfide: translation to therapeutics. Antioxid Redox Signal 22(5):398–410. doi:10.1089/ars.2014.5901
Wallace JL, Caliendo G, Santagada V, Cirino G (2010) Markedly reduced toxicity of a hydrogen sulfide-releasing derivative of naproxen (ATB-346). Br J Pharmacol 159:1236–1246
Winstead NS, Bulat R (2004) Pill oesophagitis. Curr Treatment Options Gastroenterol 7(1):71–76
Zanardo RC, Brancaleone V, Distrutti E, Fiorucci S, Cirino G, Wallace JL (2006) Hydrogen sulfide is an endogenous modulator of leukocyte-mediated inflammation. FASEB J 20:2118–2120
Zayachkivska OS (2006) Significance of NO-mediated mechanism in resistance of oesophageal mucosa. Ukr Med Almanac 9(6):48–49
Zayachkivska O, Gzregotsky M, Ferentc M, Yaschenko A, Urbanovych A (2008) Effects of nitrosative stress and reactive oxygen scavenging systems in oesophageal physiopathy under streptozotocin-induced experimental hyperglycemia. J Physiol Pharmacol 59(2):77–87
Zayachkivska O, Hrycevych N, Zvir M (2010) Effect of proinflammatory cytokine-mediated mechanism of quality of gastrointestinal restitutio ad integrum. Ann Univ Mariae Curie-Skłodowska 28(Suppl. 8):211–214
Zayachkivska O, Havryluk O, Hrycevych N, Bula N, Grushka O et al (2014a) Cytoprotective effects of hydrogen sulfide in novel rat models of non-erosive oesophagitis. PLoS One 9(10):e110688. doi:10.1371/journal.pone.0110688
Zayachkivska O, Pshyk-Titko I, Hrycevych N, Savytska M (2014b) New insight into oseophageal injury and protection in physiologically relevant animal models. J Physiol Pharmacol 65(2):295–307
Acknowledgments
This article is based on our presentations (Bula et al. 2014) during the 8th International Symposium on Cell/Tissue Injury and Cytoprotection/Organoprotection, Budapest, September 24–26, 2014, a satellite meeting of the 17th World Congress of Basic and Clinical Pharmacology 2014. We also wish to acknowledge the important contributions of the Symposium Chair, Prof. Klara Gyires (Semmelweis University, Hungary) and her support to the Ukrainian participants.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zayachkivska, O., Bula, N., Khyrivska, D. et al. Exposure to non-steroid anti-inflammatory drugs (NSAIDs) and suppressing hydrogen sulfide synthesis leads to altered structure and impaired function of the oesophagus and oesophagogastric junction. Inflammopharmacol 23, 91–99 (2015). https://doi.org/10.1007/s10787-015-0230-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10787-015-0230-7