Abstract—
Lactate dehydrogenase (LDH) is a terminating enzyme in the metabolic pathway of anaerobic glycolysis with end product of lactate from glucose. The lactate formation is crucial in the metabolism of glucose when oxygen is in inadequate supply. Lactate can also be formed and utilised by different cell types under fully aerobic conditions. Blood LDH is the marker enzyme, which predicts mortality in many conditions such as ARDS, serious COVID-19 and cancer patients. Lactate plays a critical role in normal physiology of humans including an energy source, a signaling molecule and a pH regulator. Depending on the pH, lactate exists as the protonated acidic form (lactic acid) at low pH or as sodium salt (sodium lactate) at basic pH. Lactate can affect the immune system and act as a signaling molecule, which can provide a “danger” signal for life. Several reports provide evidence that the serum lactate represents a chemical marker of severity of disease similar to LDH under inflammatory conditions. Since the mortality rate is much higher among COVID-19 patients, associated with high serum LDH, this article is aimed to review the LDH as a therapeutic target and lactate as potential marker for monitoring treatment response of inflammatory diseases. Finally, the review summarises various LDH inhibitors, which offer potential applications as therapeutic agents for inflammatory diseases, associated with high blood LDH. Both blood LDH and blood lactate are suggested as risk factors for the mortality of patients in serious inflammatory diseases.
Similar content being viewed by others
INTRODUCTION
Coronavirus disease 2019 (COVID-19) is a new coronavirus pandemic disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2); CoV-2 is highly pathogenic in the human population. The immune-pathological event for SARS-CoV-2 is acute respiratory distress syndrome (ARDS). In the majority of individuals, COVID-19 infection is asymptomatic or causes only minor symptoms. Bilateral lung involvement is a common feature on CT images of the patients’ chests [1]. In about 15–20% of patients, COVID-19 infects the respiratory tract that results in ARDS. In COVID-19 patients, the presence of “cytokine storm” has been linked to mortality. “Cytokine storm syndrome (CSS)” is a life-threatening illness caused by a cascade of cytokine activation. To minimise the implications of cytokine storm, it is critical to diagnose it early in the course of the disease. Despite the implementation of strong global outbreak in 2020, the prevalence of COVID-19 continues to rise with different evolving variants of CoV-2, posing a grave threat to human life and health. Reason for high mortality among COVID-19 patients has been linked to metabolic and endocrine systems. Approximately, 50% of the people who lost their life due to COVID-19 suffered with metabolic and vascular diseases such as hypertension and diabetes in addition to non-alcoholic fatty liver disease and obesity [2, 3].
Several reviews and meta-analyses have reported the prognostic value of lactate dehydrogenase (LDH) for severity of COVID-19 and other inflammatory diseases. Serum LDH is a metabolic as well as a prognostic biomarker for immune surveillance. A high level of LDH has been related to respiratory function and a predictor of respiratory failure in CoVID-19 patients. Its rise in serum is associated with poor outcomes in immunocompromised patients [4] and appears to be linked to serum lactate, the end product of glycolysis. According to studies, LDH is the only best measure that may predict ICU admission or serum LDH levels in diabetic COVID-19 patients aged 70 or above predicted fatality. This article is aimed to review the LDH as a therapeutic target and lactate and LDH as potential markers for monitoring treatment response of inflammatory diseases.
CORONAVIRUSES
Coronaviruses (CoVs) belong to the Coronaviridae family of viruses. CoVs are the most common pathogens in developing respiratory illness outbreaks, and they are members of a wide family of single-stranded RNA viruses [5] that can be found in a variety of animals. CoVs can cross species barriers and can cause illness in humans ranging from common cold to more severe diseases. The enveloped viruses have incredibly large single-stranded RNA genomes, having sizes between 26 and 32 kb.
CoV-2 is continually evolving, and new versions are predicted to emerge around the world. Some versions have mutations in the surface spike protein, which is a target for natural and vaccine-induced immunity and promotes viral attachment to human cells. At least seven CoV variants have been linked to human disease. SARS-CoV, which caused the SARS outbreak in 2002–2003, is one of three viruses that can cause severe sickness. Camels are still infected with the Middle East respiratory illness, which first appeared in 2012. SARS-CoV-2, surfaced in Wuhan, China, in December 2019, causes COVID-19 pathogenesis in humans [5]. The origin of SARS-Cov-2 is currently unknown, but it is speculated that it has an animal origin [5]. SARS-CoV-2 variation is highly contagious and spread swiftly across the world. The new virus was initially termed 2019-nCoV due to its resemblance to SARS-CoVs.
Several labs have reported that one of the three target genes is not found in one widely used PCR test. These variations seem to be more contagious, cause more severe disease, and/or avoid natural or vaccine-induced immune responses. The following are some of the more common circulating variants [6]:
-
Alpha (B.1.1.7 lineage), also known as 20I/501Y.V1, was originally discovered in late 2020 in the UK. According to certain research, this type may cause more serious sickness.
-
Delta (B.1.617.2 lineage), also known as 20A/S:478 K, was discovered in India In late 2020. This variant is more contagious than B.1.1.7 and is linked to a more serious sickness.
-
Omicron (B.1.1.529 lineage) variant was initially discovered in southern Africa in November 2021, later in several other nations. The variant has more than 30 mutations in the spike protein, including changes that have been linked to greater transmissibility and decreased sensitivity to neutralising antibodies in other variants of concern. The Omicron variant carries a higher chance of serious illness [6].
SARS-CoV-2
Li et al. [7] displayed the phylogentic analysis of full genome of SARS-like coronavirus. Coronavirus virions have a spherical shape under cryo-electron microscopy, with diameters of 65–125 nm [8] with club-shaped spikes on their surface. The name “coronavirus” comes from the appearance of these spikes, which resemble a solar corona. The virion’s envelope packs the nucleo-capsids, which are helically symmetrical. S (protuberances), E (envelope), M (membrane), and N (nodes) are the letters that indicate the position where the proteins are found in coronaviruses (nucleocapsid). Some virions in the subgroup A of the genus Betacoronavirus contain hemagglutinin esterase activity. CoV-2 proteins are subjected to post-translational modifications (PTMs), such as glycosylation and palmitoylation of the spike and envelope protein, N- or O-linked glycosylation of the membrane protein, phosphorylation and ADP-ribosylation of the nucleocapsid protein, and other PTMs on nonstructural and accessory proteins [9].
ACE2: the Coronavirus Receptor
The cell surface receptor angiotensin-converting enzyme 2 (ACE2) is essential for viral entry into the host cell through a binding site on SARS-Cov-2 protein S. The cell membrane serine protease 2 (TMPRSS2) is also required for viral S protein priming. Although their presence is not essential, virus entrance may be influenced by the activity of the endosomal/lysosomal cysteine proteases cathepsin B and L (CTSB, CTSL) [10, 11]. The receptor-binding domains of ACE2 receptor on host cells on CoV2 have molecular similarities with other CoVs. Though, ACE2 is the primary receptor for CoV-2, despite the fact that numerous lectin receptors and dipeptidyl peptidase 4 (DPP4) can bind CoVs [12,13,14]. The viral RNA is released into the cytoplasm after the virus reaches the host cells, and the viral genome begins to reproduce.
The SARS-CoV-2 S protein interacts to ACE2 on target cells before being processed by membrane proteases, including TMPRSS2, resulting in viral internalisation or fusion with the plasma membrane. Other receptors, besides ACE2, have also been suggested to be involved in viral binding [10, 11]. The S (spike) protein has a short intracellular tail and is linked to the envelope via a transmembrane domain. The S protein’s vast ectodomain extends outward, giving the virus a crown-like look. The S protein’s ectodomain, which consists of three S1 subunit heads for receptor binding and a trimeric S2 subunit stalk for membrane fusion, mediates viral entry. The subunits S1 and S2 of spike protein of CoV2 are responsible for cell receptor recognition and membrane fusion. The N-terminal domain (NTD) and C-terminal domain (CTD) of Coronavirus S1 can both operate as receptor-binding domains (RBD) for ACE2 [8] (Fig. 1a).
a). The metabolic pathway showing two axes of RAS system: (1) “Classical RAS ACE–Ang II–AT1 regulatory axis” and (2) “ACE2–Ang–(1–7)–Mas counter-regulatory axis.” Abbreviations: (P) RR, (pro) renin receptor; Ang, angiotensin; ACE, angiotensin-converting enzyme; ACE2, angiotensin-converting enzyme 2; NEP, neutral endopeptidase; PEP, prolyl endopeptidase; PCP, prolyl carboxypeptidase. Courtesy Gupta and Gupta [13]. b). Structure of S CTD—human ACE2 Complex: The core subdomain and external subdomain in SARS-CoV-2- CTD are colored cyan and orange, respectively. hACE2 subdomains I and II are colored violet and green, respectively. The right panel (B) was obtained by anticlockwise rotation of the left panel (A) along a longitudinal axis [PDB:6LZG]. Courtesy Wang et al. [8]
ACE2 is a class I transmembrane protein and has an enzymatically active domain on the surface of lung cells and cells of other tissues. The most abundant expression of ACE2 and TMPRSS2 among the many cell types in respiratory tissues is found in bronchial transient secretory cells [14]. After host cells are infected with CoV-2, ACE2 is internalised and its expression is reduced [15, 16]. RAS’s uncontrolled action results in the production of a slew of cytokines and chemokines that lead to a cytokine storm syndrome and severe ARDS.
The virus protein can also be discovered in the cells of the stomach, duodenum, and rectal mucosa. Lactate dehydrogenase and other liver enzymes are high in more than half of COVID-19 patients, indicating liver or bile duct impairment. Wang et al. investigated the interaction of gut ACE2 with SARS-CoV-2. The incidence of intestinal symptoms was modest despite the presence of ACE2 on intestinal epithelial cells, showing that the innate immune system is involved [17]. Paneth cells, on the other hand, secrete a human defensin 5 that binds to ACE2 and inhibits SARS-CoV-2 spike protein S1 recruitment [17].
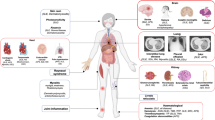
Presence of ACE2 on Different Organs
Human tissues express the ACE2, TMPRSS2, and CTSB/L genes and proteins, and the ACE2 and TMPRSS2 genes appear to be co-regulated [18]. ACE2 is found in a variety of tissues, including the gastrointestinal tract, blood-forming organs, liver, kidney, brain, and endothelial cells, with the bulk of ACE2 being found in enterocytes, tongue, and esophageal epithelial cells. ACE2 mRNA, on the other hand, is detected in practically all tissues [12, 19].
Because adipose tissue acts as a reservoir for microbial pathogens, obese people are more likely to get SARS-CoV-2 infection since they contain more adipose tissues. Diabetics have a stronger inflammatory response due to ACE2’s sustained glucose detection [11, 12, 14]. Patients with hypertension who are on treatment of ACE2-inhibitors have higher levels of ACE2 expression and are more susceptible to SARS-CoV-2 infection. TNF suppresses ACE2 and TMPRSS gene expression, which is stimulated by pro-inflammatory circumstances such as obesity, diabetes, and autoimmune disorders, as well as exercise, cigarette smoke, interferons, and androgens (reviewed in [13]).
Renin–Angiotensin System (RAS) and ACE2
The ACE2 is a major component of “renin–angiotensin system (RAS)”, also known as the “renin–angiotensin–aldosterone system (RAAS)”. RAS controls blood pressure and electrolyte homeostasis, as well as the functions of a variety of critical organs such as the heart, blood arteries, and kidneys [13]. The loss of RAS function has been linked to lung damage and ARDS, which can result in a poor prognosis and even death. RAS plays a vital role in a variety of diseases.
ACE2 is an active homologue of ACE found in a variety of tissues. The entry of viruses into host cells is the first stage in viral infection. ACE2 is the functioning SARS-CoV receptor, through which SARS-CoV can enter ACE2-expressing cells (Fig. 1b).
RAS is important in a range of clinical diseases, and ACE2 is a key component of the anti-RAS mechanism in both disease progression and defence. ACE2’s main role is to metabolise Ang II and produce the heptapeptide angiotensin-(1–7), which binds to the Mas receptor (Mas-R). In the pulmonary system, Mas-R has vasodilatory, antiproliferative, and antifibrotic actions.
When ACE2 removes the carboxyterminal phenylalanine from Ang II, it forms the heptapeptide angiotensin-(1–7). When the actions of ACE2 and ACE alternate, angiotensin (1–7) is also produced without Ang II. Throughout this process, ACE2 hydrolyzes Ang I to produce angiotensin-(1–9). RAS dysfunction has been associated with the development of acute lung injury (ALI) and ARDS, both of which have a bad prognosis and can even result in mortality [14].
RAS is important in a range of clinical illnesses, and ACE2 is a key component of the disease’s progression and defence. ACE2’s principal function is to metabolise angiotensin II and generate the heptapeptide angiotensin-(1–7), which binds to the Mas receptor (Mas-R). In the pulmonary system, Mas-R has vasodilatory, antiproliferative, and antifibrotic actions. ACE2 can remove the carboxyterminal phenylalanine from Ang II, resulting in the heptapeptide angiotensin-(1–7). Furthermore, angiotensin-(1–7) is generated without Ang II when the effects of ACE2 and ACE alternate. Ang I is first digested by ACE2 to generate angiotensin-1–9, which is then degraded by ACE to form angiotensin-1–7. Angiotensin-(1–7) binds as a ligand to the G protein-coupled receptor Mas, causing the opposite reaction to that of Ang II, and performs a variety of roles in many organs/systems [12]. Due to unbalanced ACE/Ang II/AT1R and ACE2/angiotensin-(1–7)/Mas-R axis signaling, COVID-19 causes hypercytokinemia, severe inflammation, collateral tissue damage, and systemic failure.
INFLAMMATION AND ASSOCIATED DISEASES
Inflammation is a local or systemic immune cell response that involves the activation, recruitment, and action of innate and adaptive immune cells. Inflammation is critical for tissue repair, regeneration, and remodeling. Mild types of inflammation are required for tissue homeostasis. There are several types of inflammation, according to evidence, and cells from other sections of the body are also implicated. Inflammatory responses are seen in the cells that line our blood vessels and the cells that line our skin, for example. As a result, it is a broader reaction that can affect cells all over the body. The inflammatory process starts, when chemicals are released by injured tissue. White blood cells respond by producing chemicals that assist cells in dividing and growing in order to heal tissue. The inflammatory process can start even if there is no injury in chronic inflammation, and it does not stop when it should. However, there is debate over whether inflammation is beneficial or harmful due to misinformation. As evident from several reports, we need to know details about the biology of inflammation and its relationship to cancer in order to discover the next breakthrough in cancer therapy [20,21,22,23,24].
Cancer as an Inflammatory Disease
Cancer has two hallmarks: immune evasion and dysregulation of energy metabolism, which may be functionally related. Immunosuppressive metabolites and by-products, such as lactate, are released by malignant cells in metabolically demanding conditions and developing a metabolic symbiosis with immune cells. This acidic tumor microenvironment (TME) has a significant impact on the immune cell profile of tumor-infiltrating immune cells, and is important for immunosuppression. The study of immune system and inflammation in cancer formation and its treatment has resurfaced as a major topic of research in recent decades. Inflammation is critical for tissue repair and regeneration. It is necessary for tissue homeostasis and maintenance. However, research reports have shown that there are different types of inflammation which involve cells from different parts of the body. Inflammatory responses are also seen in the cells that line our blood vessels and those that coat our skin. The inflammatory process in chronic inflammation can start even if there is no injury, and it does not stop when it should. However, there is still uncertainty over whether inflammation is beneficial or harmful due to misinformation.
Inflammation plays a vital part in carcinogenesis and is a critical component of tumor growth, but it was not until the late 1990s that conclusive proof was discovered. Infection, persistent irritation, and inflammation are all factors that contribute to the development of cancer. Inflammation increases all phases of carcinogenesis and prepares for the formation of cancer. To generate an inflammatory tumor microenvironment (TME), cancer cells, as well as adjacent stromal and inflammatory cells, engage in well-orchestrated reciprocal interactions. The phenotypic and functional properties of cells within the TME are constantly changing. References [23,24,25] discovered the origins of inflammation in tumors and proposed mechanisms by which inflammation gives rise to tumor formation, its development and spread. Greten and Grivennikov suggested that tumor-promoting inflammation is similar to inflammatory processes found during growth, immunity and tissue homeostasis, or tissue repair; and how inflammation can aid in the development of anti-cancer therapy [25]. The TME, which is predominantly regulated by inflammatory cells, is now recognised as critical.
At every stage of carcinogenesis, the immune system plays a substantial pro- and anti-tumorigenic role. The immune system’s anti-tumorigenic function is endogenous, meaning that it occurs naturally in response to altered and malignant cells [25]. According to S.S.Watowich, “we need to know details about the biology of inflammation and its relationship to cancer in order to develop the next breakthrough in cancer therapy”. Watowich’s study focuses on how inflammation triggers T cell responses – the cells that clean out pathogens and even tumors that make us sick – and how these events are impacted in cancer.
Chronic inflammation has been related to pro-inflammatory cytokines, chemokines and inflammatory enzymes and linked to a number of disorders, including cardiovascular disease, cancer, diabetes, arthritis, Alzheimer’s disease, pulmonary disease, and autoimmune disease [20]. Various infections have been related to the development of cancers such as gastric cancer, mucosal lymphoma, and cervical and liver carcinomas. Autoimmune diseases and inflammatory conditions of unknown origin are all known to increase cancer risk or progression (e.g. prostatitis for prostate cancer). Inflammation linked to cancer can cause genomic instability [20]. Chronic inflammation can damage DNA and lead to cancer if left untreated. Colon cancer is more common among persons who have chronic inflammatory bowel illnesses such as ulcerative colitis and Crohn’s disease. As a result, inflammation is crucial in the development of tumors.
SARS-CoV-2 Infection and Its Pathogenesis
The pathogenesis of SARS-CoV-2 infection and inflammatory responses is linked to the damage of the airways. As a result, the severity of sickness in SARS-CoV-2 patients is dependent not just on viral infection but also on the host response. ARDS is characterised by low blood oxygen levels and difficulty in breathing in severe cases. This could lead to respiratory failure, resulting in death in 70% of COVID-19 cases. Some patients may not survive due to subsequent bacterial and fungal infections. Furthermore, the massive production of cytokines by immune cells in response to viral and/or secondary infections can cause sepsis symptoms in 28% of fatal COVID-19 patients. Multi-organ failure, mostly of the cardiac, hepatic, and renal systems, is caused by uncontrolled inflammation in such instances [26, 27].
In COVID-19 patients, acidity levels in the blood and other regions of the body have been found to be higher. Hypoxia and acidosis, when combined, cause the patient’s state to rapidly deteriorate and lactate (lactic acid) levels in the blood show poor clinical outcomes. It is recommended that more attention be paid to prevent acidosis, particularly in the early stages of the disease, when it is less dangerous. During inflammatory activation, innate immune cells release a lot of lactate. Human studies demonstrate that expression of genes involved in lactate metabolism and transport is altered in human immune cells during infection and in vitro inflammatory activation with TLR ligands, implying that lactate metabolism plays a significant role in inflammation. Lactate appears to be a regulator of immune cell metabolism, resulting in reduced inflammation and possibly serving as a negative feedback signal to prevent excessive inflammatory reactions [28].
Inflammation and thrombosis, as well as trouble with gas exchange in the lungs, all contribute to the establishment of acidosis in the early stages of the disease. According to this theory, a drop in blood pH causes a drop in oxygen saturation, which contributes to the exacerbation of acidosis and a worsening of the patient’s state. Low extracellular pH in patients can also cause conformational changes in proteins, which can lead to function loss. This suggests that maintaining a normal blood pH is a treatment strategy for COVID-19 and other inflammatory diseases [29].
SARS-CoV-2 syndrome is linked, in part, to immune system dysregulation involving three primary components: (1) increased innate immune activity; decreased production of type 1 interferon (IFN) by SARS-CoV-2-infected cells, and lowered levels of CD4+ and, in particular, CD8+ T cells. (2) When triggered, innate immune cells change their metabolism and increase glucose uptake in order to secrete pro-inflammatory cytokines. (3) Changes in glucose metabolism are also seen in pulmonary epithelial cells, resulting in cytokine dysregulation and pulmonary epithelial inflammation. (4) In severely ill patients, controlling hyperglycolysis may help to limit the overproduction of pro-inflammatory cytokines and optimise the adaptive immune system’s functions. (5) According to reports, non-toxic quantities of 2-DG, the use of GLUT 1 inhibitors, large doses of antioxidants such as vitamin C, and high doses of N-acetylcysteine may be beneficial additional therapy options for these patients. Overall, knowing alterations in the glycolytic pathway linked to COVID-19 infection can aid in the development of new therapeutic options for this disease [30].
Metabolic Pathways in Inflammation
Inflammation is a defensive response that serves to protect and rebuild our tissues against infection, tissue damage, or stress. Various cells are activated during the inflammatory response to combat injuries induced by a range of substances and to maintain tissue homoeostasis. Acute or persistent inflammation is possible. Inflammatory processes are widespread in many diseases and can lead to the development of inflammatory disorders like autoimmune diseases, cancer, neurological diseases, and cardiovascular diseases [21, 22]. The key controllers of inflammation are now known to be immune cells and their metabolism [23]. An increasing amount of research suggests that glycolysis and tricarboxylic acid (TCA) cycle produced metabolites can have immunomodulatory effects during inflammation. The most critical chemicals like succinate, citrate, and lactate, as well as epigenetic modulators are signaling molecules which control the inflammatory response and immune cells that reprogramme their metabolism to regulate or change their inflammatory phenotype. As a result, present research [24] looks for a metabolic shift as a source of inflammation.
Among inflammatory cells, Th1 and Th17 cells, reactive microglia, endothelial cells, and M1 macrophages depend on glycolysis and glutaminolysis for their high biosynthetic and bioenergetic demand, with a dysregulated TCA cycle and higher rate of lipid synthesis, as well as the pentose phosphate pathway (PPP) (Fig. 2). However, once the inflammatory reaction is over, regulatory and memory T cells, resting microglia, and M2-type macrophages rely on OXPHOS and fatty acid oxidation, and maintain tissue homoeostasis and dampen the response. Increased knowledge of inflammatory cells’ metabolic processes could be used therapeutically to lessen the intensity of inflammatory responses [23]. In the present report, we review the role of lactate and its regulatory enzyme, LDH, in the regulation of metabolic environment of inflammatory diseases with major emphasis on COVID-19 patients.
According to Krishnan et al. [31], increased plasma glucose and mannose levels were associated with the severity of Covid-19 illness. Blocking the metabolic pathways generated a considerable reduction in virus production. Glycolysis and glutaminolysis are important for virus replication. Severe SARS-CoV2 is thought to use and rewire mechanisms mediating central carbon metabolism, resulting in hazardous metabolite efflux and being linked to illness severity. As a result, perturbing the host metabolic system could be an appealing technique.
Denson et al. [2] suggested that metabolic syndrome was associated with increased risks of ARDS and death in patients hospitalised with COVID-19. The association with ARDS was cumulative for each metabolic syndrome criteria present [2]. The link between ARDS and each metabolic syndrome criterion was cumulative. Thus, we find similarity in metabolic pathways in carcinogenesis and viral diseases as COVID-19 (Fig. 2).
Reprogramming of Metabolism in Covid-19
Aerobic Glycolysis or Warburg Effect
Metabolism is the heart of all biological processes that provides energy and building blocks for macromolecules. Tumor cells generate a high amount of ATP and biosynthetic metabolites, which can aid in cancer cell survival and multiplication. Otto Warburg observed that even in the presence of oxygen, cancer cells consume a lot of glucose and produce a lot of lactate. This process of aerobic glycolysis was called “Warburg effect” [32].
Monocytes and macrophages in the lungs of COVID-19 patients in response to infection [33] respond to infection by releasing more inflammatory cytokines [31, 34]. SARS-CoV-2 replication in monocytes requires a metabolic base, in which glycolytic flux is significant and necessary for SARS-CoV-2 replication. Several studies have suggested that metabolic processes such glycolysis, the TCA cycle, the pentose phosphate pathway (PPP), oxidative phosphorylation, amino acids, fatty acid (FA) synthesis, and nucleic acids synthesis (NA), among others, comprise various pathways that serve to maintain homeostasis. The disturbances in these pathways are responsible for the development of infectious and non-infectious disorders [31, 35] (Fig. 2). However, Silva et al. showed that glycolysis can interfere with antiviral signaling [35].
Under normal physiology and in presence of oxygen, pyruvate enters the TCA cycle and completely metabolises TCA metabolites to CO2, creating NADH and decreased FADH2 via the electron transport chain oxidative phosphorylation (OXPHOS). Through aerobic glycolysis, pyruvate can be converted to lactate in the presence of oxygen in cancer cells, without creating ATP but regenerating NAD+. Because glycolysis is inefficient compared to OXPHOS, growing cells, such as cancer cells, prefer aerobic glycolysis [32]. This is known as metabolic reprogramming, and it occurs when cancer cells change their metabolism to meet their increased energy needs as a result of their rapid growth and multiplication (Fig. 2).
Glycolysis is a metabolic pathway that produces energy for biological functions. Glycolysis involves a set of enzymes that convert glucose to pyruvate. The LDH isoenzymes catalyse the interconversion of pyruvate and lactate, which is a crucial step in the anaerobic metabolism of glucose when oxygen is unavailable or limited. The LDHA or LDH5 isoform catalyses the conversion of pyruvate to lactate preferentially, preventing pyruvate from entering the TCA cycle. The LDHB (or LDH1), on the other hand, is predisposed to convert lactate to pyruvate while also producing NADH [36].
When immune cells are triggered to create an inflammatory response, they also undergo metabolic reprogramming, like cancer cells, and preferentially employ glycolytic pathway as a source of energy during peak of inflammation, whereas they favour OXPHOS metabolism during the resolution phase, developing a pro-resolving character (Fig. 2). As a result, it has been known in recent years that distinct metabolic pathways influence immune cell fate and the inflammatory response [23]. In addition to metabolic reprogramming, epigenetic alterations in internal organs caused by SARS-CoV-2 also contribute to systemic toxicity and death in COVID-19 [37].
Reprogramming of Glucose Metabolism in COVID-19
The molecular basis of COVID-19’s dysregulated glucose metabolism is poorly understood. The discovery of the molecular processes used by viruses and cancers in their host metabolism expands the therapeutic toolbox available to fight viral disease [38, 39]. Although viral infection is known to alter host cell metabolism for more than half a century, the processes and effects of virus-induced metabolic reprogramming have been examined in depth only recently. Since viruses depend on the machinery of the host cell to replicate–they choose anabolic metabolic pathways to generate the macromolecules required for virion replication and their synthesis.
Infection with RNA-containing viruses results in three types of anabolic reprogramming in host cell metabolism: (1) by increasing glucose uptake and switching to aerobic glycolysis, which involves upregulating rate of glycolysis and glucose transporters in the membrane; (2) resulting in an increase in the concomitant production of lactate, as well as upregulating both glycolysis and glycogenolysis, which provide TCA cycle intermediates needed for enhanced lipogenesis; and (3) by activating the PPP that results in enhanced production of nucleotides required for viral replication [38].
Viruses and cancer cells take up resources like glucose at a faster rate to sustain metabolic signaling, i.e. aerobic glycolysis. For example, human monocytes grown in the presence of high glucose levels, after SARS-CoV-2 infection, undergo metabolic reprogramming, which results in greatly increased viral multiplication and cytokine production such as TNF, IL-1, and IL-6 [40]. Lung epithelial cells die as a result of this. It explains why diabetics are more prone to CoV-2 and develop severe COVID-19. As a result, in diabetes, impaired glucose metabolism and metabolic derangement are an innate cellular mechanism that favours SARS-CoV-2 pathogenesis.
Codo et al. demonstrated that SARS-CoV-2-infected blood monocytes can cause a cytokine storm (excessive synthesis and release of inflammatory cytokines), as seen in severe COVID-19. Surprisingly, increased glucose levels boosted SARS-CoV-2 multiplication, ACE2 transcription, and cytokine secretion in monocytes, implying that elevated glucose is a major inducer of virus replication and inflammatory response. As a result, in diabetics, impaired glucose metabolism and metabolic derangement are the innate cellular mechanism that favours SARS-CoV-2 pathogenesis [38]. Since 2-deoxy-d-glucose (2-DG) also inhibits glycolytic enzymes and LDHA as well as abolished viral replication and cytokine generation, it appears that glycolysis is a crucial event in SARS-CoV-2 pathogenesis [40, 41]. In SARS-CoV-2-infected monocytes, there was also an increase in mitochondrial ROS and impaired oxidative metabolism [38,39,40, 42]. According to the observations, higher glucose metabolism in COVID-19 patients could worsen adjacent cells by aerobic glycolysis and subsequent cytokine production in monocytes (Fig. 2).
During CoV-2 infection, the cell energetics is a critical aspect for inflammatory responses of the host metabolism during CoV-2 infection. Higher levels of the proinflammatory cytokine IL-1, linked to the production of 3-phosphoglycerate, a glycolysis intermediate product, further imply a direct link between COVID-19 and glucose metabolism. In another approach, glycolysis inhibition in mice with 2-DG reduced IL-1 production [34], proving this hypothesis. These findings suggest that metabolic rewiring with a shift toward aerobic glycolysis increases SARS-CoV-2 propagation and cellular host response, similar to the cytokine storm caused by influenza A virus (IAV) [41, 43]. Thus, glucose metabolism and glycolysis can act as antiviral targets for COVID-19 treatment, particularly in individuals with metabolic disorders [36].
Lipid Metabolism and CoV-2 Infection
In viral infection, lipids perform a range of roles, including influencing lipid signaling, host cell metabolism, and undermining the protective immune response. Studies have suggested that disrupting lipid synthesis affects virus replication, implying that lipid pathways are important target in viral disease research. Lipid levels are altered in SARS-CoV-2 patients, with larger quantities in individuals with a higher fatality rate [44,45,46], suggesting that changes in lipid metabolism may be a crucial event in COVID-19 development. Thomas et al. discovered an increase in “free fatty acids” in the blood, and their association with high levels of inflammatory cytokines during CoV-2 infection [46]. Another study highlighted the role of loss of blood malic acid and glycerol 3-phosphate in the mortality of patients suffering with either severe or mild COVID-19, suggesting a change in energy metabolism in CoV-2 infection [45] (Fig. 2).
LACTATE–A KEY PLAYER IN THE INFLAMMATORY RESPONSE
Lactate Metabolism
For cellular integrity and function, an appropriate quantity of oxygen is required. Tissue hypoxia can lead to multi-organ failure and death if it is not treated. As a result, monitoring tissue oxygenation is a vital component of critical care, allowing for prompt intervention aimed at restoring a sufficient supply of oxygen. Tissue oxygenation has been monitored using blood lactate concentration measurements. Only the introduction of electrode-based lactate sensors made it possible to monitor blood lactate levels in real time in a critical care scenario. The concentration of lactate in the blood has been used to evaluate tissue oxygenation. Only the introduction of electrode-based lactate monitoring made it possible to monitor blood lactate levels in real time in a critical care scenario. It is observed that patients with a high blood lactate level (hyperlactatemia) have a low blood pH (acidosis). Lactic acidosis is the result of a combination of hyperlactatemia and acidosis, the common cause of metabolic acidosis. The content of blood lactate in healthy people is kept between 0.5 and 1.5 mmol/L. This represents a balance between the pace at which erythrocytes and other tissue cells produce lactate into the blood stream and the rate at which lactate is cleared from the bloodstream, primarily by the liver and kidney.
Lactate is primarily consumed and produced by skeletal muscles, the heart, and the brain [47]. Lactic acid levels are increased when the flow of blood and oxygen in the body is reduced by vigorous physical exercise or pathological conditions–such as heart failure and sepsis. Lactate has long been thought of as a “waste” product of cell metabolism that builds up at sites of inflammation [48,49,50].
Inside cells, LDHA catalyses the forward and backward conversion of pyruvate to lactate. LDHB, on the other hand, converts lactate to pyruvate. Lactate levels in the blood appear to be a chemical predictor of sickness severity in all circumstances. Lactate is a key molecule involved in COVID-19 mortality, similar to cancer, according to the findings discussed in this review. The possible targeting of LDH and lactate production in serious COVID-19 patients is discussed [51] (Fig. 3).
Lactate: the Prime Causative Factor of Inflammation
The serum lactate level has been included in the recent consensus definitions for septic shock. Lactate is a foremost component of the inflammatory microenvironment. On the one hand, proinflammatory cells such as inflammatory M1 macrophages, Th1 and Th17 lymphocytes, and activated microglia may quickly give energy to fuel inflammation, regulatory T cells or M2 macrophages, on the other hand, which are engaged in inflammation resolution, preferentially employ fatty acid oxidation via the TCA cycle for production of energy.
Lactate buildup is a feature of inflammatory areas, including rheumatoid arthritis (RA) synovitis, and is partly responsible for the creation of an acidic environment. Lactate can be sensed by T cells via the production of particular transporters, which inhibits their mobility. Lactate’s interference with intracellular metabolic pathways, particularly glycolysis, causes this “ inhibitory signal”. Lactate also increases the conversion of CD4+ T cells to an IL-17+ fraction while lowering the cytolytic activity of CD8+ T cells. Autoantibody generation at inflammatory locations, such as in RA synovitis, multiple sclerosis, and other autoimmune disorders, could be caused by these processes [52].
To fulfil their high energy and biosynthetic requirements, inflammatory cells switch their metabolism to glycolysis [23]. Interestingly, metabolites that accumulate under glycolytic settings have been shown to enhance the inflammatory response by modifying intracellular signaling pathways, remodeling the epigenetic landscape, and controlling posttranscriptional and post-translational alterations, among other things. In terms of its impact on inflammation, immunological and vascular cells’ glycolytic metabolism can be used to target inflammation-related diseases [23] as COVID-19 (Fig. 4).
Lactate shutle ststem: In aerobic glycolytic pathway, glucose from the bloodstream enters the cell cytosol via the glucose transporter (GLUT) (1). In the cytosol glucose is broken down into pyruvate via the glycolytic process (2). While pyruvate enters the mitochondrion, allowing respiration and energy production (3) to continue in the TCA cycle, the cytosolic lactate, produced by the cytosolic LDH (4), is exported to the extracellular compartment via monocarboxylate transporter (MCT) (5), where it is redistributed to other functional sites. The cytosolic lactate also enters the mitochondria (6) and is converted to pyruvate in the presence of mitochondrial mLDH (7), forming the basis of the intracellular lactate shuttle system [44].
Genetic Modifications by Lactate
The role of glycolysis deregulation has been linked to epigenetic gene regulation mechanisms in cancer cells. Pyruvate, in particular, affects histone acetylases (HAT) and deacetylases (HDAC), resulting in an increase in glycolytic enzymes and transporter transcription. As a result, glycolysis metabolites may be involved in epigenetic feedback loops, necessitating further investigation. Furthermore, exposure of muscle cells to lactate has been shown to cause a significant change in gene expression [53].
Zhang et al. reported lactate-derived histone lysine lactylation as epigenetic modification, claiming that histone lactylation increases gene transcription from chromatin directly [54]. In human and mouse cells, Zhang and colleagues discovered 28 lactylation sites on core histones. Lactylation of histones occurs at a different time than acetylation. Increased histone lactylation promotes homeostatic genes involved in wound healing in the late stages of M1 macrophage polarisation. Histone lactylation is a novel approach in understanding lactate’s functions and its role in a variety of pathophysiological conditions, such as infection and cancer [54].
Lactate-Induced Lactic Acidosis
Lactate is important for a variety of biological and clinical processes. In critically ill patients, blood lactate concentration is frequently tested. Lactate is produced as a by-product of glycolysis and is thought to be the outcome of cellular oxygen deficiency caused by tissue hypoperfusion. Blood lactate levels that are decreasing are stronger indications of seriousness of a disease. Lactate production is aided by hypoxia, inflammation, viral infection, and malignancies. To carry out its complex functions, lactate activates G protein-coupled receptor 81 (GPR81) or shuttles across membranes via monocarboxylate transporters (MCTs). Lactate is now recognised as a functional chemical capable of influencing immunological responses.
Lactate is a product of glucose metabolism and the end product of anaerobic glycolysis. It is formed when lactic acid is dissociated into an anion. In the cytoplasm of all cells, the glycolytic process can run anaerobically. The enzyme lactate dehydrogenase converts pyruvate to lactate in the final phase of anaerobic glycolysis. This final step produces NAD+, which is required for anaerobic glycolysis to proceed. Pyruvate is not preferentially converted to lactate in well-oxygenated tissue cells which contain mitochondrion, rather converted to carbon dioxide and water in mitochondria via lactate shuttle associated with the citric acid cycle and electron transport chain. During hyperlactatemia, lactate concentration in the resting blood is unusually high (> 1.5 mmol/L) and linked to an abnormal accumulation of hydrogen ions (H+) and a predisposition to acidosis [55].
Elevated blood lactate levels have been associated with vigorous exercise and pathological conditions including shock, sepsis, cardiac arrest, trauma, seizure, ischemia, cancer, rheumatoid arthritis synovitis and others [56,57,58,59]. Although clearance declines in some clinical situations, such as septic conditions in humans and animals, hyperlactemia is linked to lower clearance rather than increased production [60]. Although lactate clearance as a resuscitation endpoint for revival has potential, additional research is needed in this field, because of limited sensitivity and specificity of the lactate assay [61] (Fig. 5).
Role of lactate as a key player in inflammatory cells such as cancer cells: Abbreviations used: DC, dendritic cell; EC, endothelial cell; GLUT, glucose transporter; IL, interleukin; MCT, monocarboxylate transporter; PPP, pentose phosphate pathway; ROS, reactive oxygen species; TAF, tumor-associated fibroblast.
Lactate is linked to treatment for a variety of illnesses [62]. Lactate levels in the blood should be between 0.5 and 1 mmol/L in order to be considered normal. A persistent, mild to moderately increased lactate level (2–4 mmol/L) without metabolic acidosis is referred to as hyperlactatemia. When tissue perfusion and oxygenation are adequate, this can happen. Arterial blood lactate is equivalent to or lower than in central venous blood under healthy conditions. Lung damage in COVID-19 patients is paralleled by arterial lactatemia that is higher than central venous lactatemia, which is then followed by the administration of an immune suppressant drug (as canakinumab). One of the outcomes of the COVID-19-related cytokine storm is a reversed Delta a-cv lactate, which could represent a disruption in the lung cell’s mitochondrial metabolism caused by inflammation or other uncoupling mediators. Delta a-cv lactate decrease may suggest canakinumab’s anti-inflammatory activity, according to a small study [62] (Fig. 5). One of the outcomes of the COVID-19-related cytokine storm is a reversed Delta a-cv lactate, which represents a disruption in the lung’s mitochondrial metabolism caused by inflammation or other uncoupling mediators. According to a small study [62], a decrease in delta a-cv lactate may indicate canakinumab’s anti-inflammatory activity (Fig. 5).
Under physiological pH 7.4, most lactate is deprotonated and present as lactate anion, a negatively charged, physiologically active form [50]. The generation of significant amounts of lactate in cancer causes an acidification of extracellular microenvironment at pH 6.0 to 6.5. Angiogenesis and immunosuppression are aided by acidosis, which has been associated with a worse clinical outcome. Lactate is an essential oncometabolite that acts as a switch in cancer’s metabolic reprogramming. Lactate levels above a certain threshold are linked to a poor prognosis for cancer. H+-monocarboxylate transporters (MCTs) transport lactate and a hydrogen ion out of the cell together, causing the immediate environment to become acidic. The resulting drop in pH may aid cancer cell invasion and metastasis by destroying normal host cells, freeing up space for the tumor and maybe releasing nutrients that the tumor can ingest. Furthermore, secreted lactate has been suggested as a source of nutrients for nearby cells. Lactate, which is secreted by cancer cells, has also been proposed as a source of nutrition for non-tumor stromal cells. In terms of lactate recycling, cancer can be viewed as a micro-ecosystem in which the various tumor components participate in complimentary metabolic pathways that allow for the recycling of waste product molecules from aerobic glycolysis to support tumor growth. Glutaminolysis, in addition to glycolysis, is another source of energy that contributes to increased lactate buildup in tumor cells [58, 63,64,65,66] (Fig. 5).
Above discussion suggests that lactate levels can be followed in the pathogenesis of COVID-19 and lactate blockers can be used to treat the patients. The lactate-induced acidosis hypothesis states that lactic acid is dissociated into lactate ions and hydrogen (H+) while entering skeletal myocytes under hypoxic conditions, such as during anaerobic exercise [50]. Acidosis is produced as a result of this process, which disrupts the cross-bridge cycle and reduces the ability of such cells to contract. Overall, studies imply that lactate accumulation during exercise disrupts the acid–base balance within skeletal muscle, resulting in decreased physical performance.
Despite the fact that the physiology and pathology of acidosis are substantially more complicated than the generation of protons in any metabolic route, it is established that acidosis happens during exercise and other conditions. Blood pH (H+) is hypothesised to be influenced by the partial pressure of CO2 (pCO2), the concentration of weak acids in plasma (mostly amino acids and proteins), and the strong ion difference (SID meq/L) (the sum of the strong cations’ concentrations minus the sum of the strong anions) [47].
Metabolic Shift from OXPHOS to Aerobic Glycolysis in Sepsis
Sepsis is an infection-related clinical condition defined by a systemic inflammatory reaction. Patients with sepsis-induced cytokine storm have a significant mortality rate due to elevated blood lactate and poor lactate elimination. There is frequently a metabolic shift from mitochondrial OXPHOS to aerobic glycolysis during critical illness. Nalos et al. employed transcriptome analysis to look at the cellular metabolism of nonhypoxic critically ill individuals’ circulating blood cells and discovered that metabolic pathways are reprogrammed significantly during critical illness. These researchers concluded that during critical sickness, aerobic glycolysis occurs in nonhypoxic cells [64]. Lactate production, multiple organ dysfunction, and poor outcomes are all linked to this transition. Lactic acid reduced LPS-induced cytokine production and NF-B-mediated transcription of cytokine production in mouse mast cells. In addition, lactic acid dramatically reduced cytokine production in mice after LPS-induced endotoxemia. This suggests that increasing glycolysis and ATP generation could boost immune function by counteracting the immunosuppressive effects of lactic acid in sepsis [65] (Fig. 2).
Lactic acid levels began to rise dramatically on the 18th day of the patient’s sickness with normal pCO2 levels in a fatal case of metabolic acidosis following cytokine storm in a COVID-19 patient. It was thought that the cause of the cytokine storm was metabolic acidosis, which is akin to severe bacterial sepsis. Another possibility is that COVID-19 individuals have significant microvascular thrombosis, which causes tissue hypoxia. High lactic acid levels appeared to be linked to a high WBC count, while there is also the possibility of mitochondrial damage from lopinavir and ritonavir treatment [66].
Lactate as Activator of HIF1 and Glycolysis
The tumor stromal extracellular lactate is one of the HIF1 activators. The discovery of a link between metabolic and genetic differences in cancer cells has rekindled interest in cellular metabolism [67, 68]. One of the HIF1 activators is tumor stromal extracellular lactate. Akt (Akt, a serine/threonine kinase earlier known as protein kinase B (PKB)) is known to activate HIF-1 in hypoxic setting, which upregulates enzymes involved in anaerobic glycolysis and glucose influx. Akt also speeds up the creation of lipids, which is a crucial mechanism for cell growth-related membrane synthesis. Lactate preconditioning appears to prime fibroblasts to switch from OXPHOS to glycolysis, in part via stabilising HIF-1 through ROS. Lactate preconditioning increases the quantity of MYC and SNAI1 transcripts, which are important facilitators of early somatic cell reprogramming [69, 70]. Thus, all genes of glycolytic enzymes of glucose metabolism are transcriptionally stimulated by HIF-1 (Fig. 5).
Effect of Lactate on Immune Metabolism
Lactate regulates monocytes, NK Cells, mast cells, T cells, tumor cells, fibroblasts, dendritic cells, the polarisation of macrophages, and the differentiation of Th1, Th17, myeloid-derived suppressed cells (MDSCs) , and Tregs, all of which contribute to the host’s immune homeostasis and their effects on viral infection, acute inflammation, chronic inflammation, sepsis, and tumor immunosuppression [71]. Lactate has a double-edged influence on host immunity and associated inflammatory reactions, making it a promising target for treating tumors and infectious illnesses [71]. Lactic acid suppresses the cytotoxic activity of human CTLs by suppressing their proliferation and cytokine generation by up to 95%. Because lactic acid buildup in cells impairs cellular metabolism, activated T cells that use glycolysis rely on effective lactic acid generation (Fig. 5).
T Cells
The importance of aerobic glycolysis in innate immune cell metabolism during immune activation has been highlighted in recent years. The magnitude of T cell-mediated immune responses in unfractionated lymphocytes is regulated by l-lactate. External lactate prevents mitogenically activated T cells from using glucose. On immune cells, tumor-derived lactate is immunosuppressive, similar to the immunosuppressive phase of sepsis [72, 73].
TCR (T cell receptor) interaction triggers cellular immune responses, tightly controlled by cytokines, which then influence differentiation, proliferation, and survival. Altering metabolic pathways can affect the actions of immune cells and their different cellular subtypes, and how they produce and expend energy [74, 75]. For example, naïve T cells are quiescent, with a low energy demand that is met primarily via oxidative phosphorylation, but after TCR activation, T cells markedly increase their metabolic activity via aerobic glycolysis and later upregulating oxidative ATP production [75], with production of a range of cytokines, during growth, by signaling events generated by TCR and the co-stimulatory molecule CD28 [76, 77]. Lactate’s role in modifying proi-nflammatory T cell motility and effector activity has been verified in numerous studies, providing a possible molecular basis for T cell entrapment and functional alterations at the sites of chronic inflammation [49, 63] (Fig. 5).
Cytotoxic T Cell Responses
-
(a)
Proliferation of resident T cells
Residents T cells proliferate in the lungs in severe COVID-19 patients, accounting for the bulk of T cells, in contrast to CD8+ effector cells which proliferated in moderate instances, because of symbiotic connection between alveolar macrophages and resident CD-8 cells [78]. Beiter and colleagues suggested that exercise may play a role in reducing harmful local T cell growth [79, 80]. On the other hand, glycolysis and lactic acid had no effect on CD8+ T cell motility. Mueller et al. [81] postulated a molecular basis for functional alterations in T cells at inflammatory sites as well as targeted therapeutics for chronic inflammatory diseases (Fig. 5).
-
(b)
Effect of lactate on T cell effector function
Lactate has been shown to affect pro-inflammatory T cell motility and effector functions [53, 55, 63]. Lactate increase has been reported to produce a stop-migration signal in T cell effectors in inflammatory conditions. Lactate stimulates CD4+ T cell for IL17 production and inhibits CD4+ T cell motility by increasing fatty acid synthesis and downregulate glycolysis [53]. Lactic acid, on the other hand, suppresses the death of CD8+ T cells.
Interleukin (IL)-2, a cytokine with pleiotropic actions and therapeutic effects, is used to expand cells for adoptive cell therapy [82]. IL-2 boosts stem cell memory T cells and antitumor responses. However, besides its beneficial effects, IL-2 can induce T cell differentiation and diminish antitumor efficacy [83], while IL-21 promotes terminal differentiation, resulting in lymphocytes that are ineffective against malignancies. During investigation of the role of metabolic reprogramming induced by IL-2 and IL-21, supported by Hermans et al. [84] who suggested that LDH plays a major role in modulating cytokine-mediated T cell differentiation.
Lactic acid, being a pro-inflammatory mediator, can stimulate the IL-23/IL-17 pro-inflammatory pathway, which is viewed as a key detrimental route in the setting of COVID-19 infection [56, 57, 79]. Inflammatory and autoimmune illnesses, as well as cancer, are caused by IL-17A, which is produced by Th17 cells. Toll-like receptor (TLR) ligand-mediated expression of IL-23 is enhanced by tumor-derived lactic acid, resulting in an increase in pro-inflammatory IL-17A production. The key cell types involved in lactic acid’s potential to increase IL-17A production are macrophages and effector/memory CD4+ T cells. Th17 cells released significant levels of IL-17A despite lactic acid suppressing their growth. Lactate causes T cells to release more IL-17, and causes cytolytic activity to be lost [85, 86] (Fig. 5).
-
(c)
Lactate stimulates lactate transporters on T cells
Lactate buildup in inflamed tissue causes human CD4+ T lymphocytes to upregulate the lactate transporter Slc5a12. Lactate absorption by Slc5A12 causes a change in the effector phenotype of CD4+ T cells, culminating in enhanced IL-17 production via nuclear PKM2/STAT3 and increased fatty acid synthesis. The expression of particular lactate transporters by distinct subsets of T cells, such as sodium lactate transporter Slc5a12 in CD4+ T cells and lactic acid transporter Slc16a1 in CD8+ T cells, determines the functional alterations of these critical properties of T cells. Lactate transporters on T cells can, therefore, be viewed as new therapeutic targets for chronic inflammatory diseases [63].
Antibodies that block Slc5a12 in a murine model of arthritis lessen the severity of the disease. Lactate/Slc5a12-induced metabolic reprogramming has been postulated as a differentiating feature of lymphoid synovitis in individuals with rheumatoid arthritis, as well as a potential therapeutic target in chronic inflammatory disorders [57]. Lactate, in turn, causes Slc5a12 expression on human CD4+ T lymphocytes in inflamed tissue.
Macrophages: Polarisation and Phenotype Switching
Macrophages’ phenotype depends on anatomic region where they are present. They can switch their character according to environment. Reports suggest that tumor-derived lactate directs cancer-associated macrophages to become M2-like polarised cell, which suppresses tumor growth in the microenvironment [70]. Lactate also inhibits the synthesis of TNFα, a pro-inflammatory cytokine, and delays LPS-induced signaling [87, 88]. However, genetic deletion of GPR81, the lactate receptor or its suppression by its antagonist, can limit the effect of lactate on immunological activities [73, 89] (Figs. 2 and 5). Lactate from macrophages can also act as a regulatory signal, allowing macrophage-like accessory cells to improve helper T cell function [57].
M1 macrophages produce a lot of pro-inflammatory cytokines, have a lot of microbic and tumoricidal activity, and have a lot of reactive nitrogen and oxygen species, and they promote the Th1 response. M2 macrophages, on the other hand, support tumor formation and suppress effector T cells while also clearing parasites, remodeling tissue, resolving inflammation, and tolerating self-antigens [90]. Macrophages switch from M1 to M2 during aerobic exercise, resulting in an improvement in inflammatory condition due to a decrease in LPS produced by exercise [91, 92]. Lactate regulates YAP and NF-B activation, which affects the lactate-suppressed macrophage pro-inflammatory response, such as reduced pro-inflammatory cytokine production in macrophages [72, 73] (Figs. 2 and 5).
Lactate influences the immunological response in prostatic adenocarcinoma at the stromal level, including the activation of tumor-associated macrophages (TAM) and the inhibition of cytotoxic T cells [93,94,95]. Tumor-associated macrophages have the ability to speed up the course of cancer. The lactate-ERK/STAT3 signaling pathway, which stimulates macrophage M2-like polarisation and is a possible novel therapeutic target for breast cancer, is the driver of breast cancer progression [95].
NK Cells
Natural killer cell (NK cell), the prototypic member of the innate lymphoid cell family, is the founder member of innate immune system. These effector lymphocytes control microbial infections and their expression, as well as a variety of malignancies. NK cells are found in almost all human tissues and have activating and inhibitory receptors, characterised in humans by phenotypic marker CD56 [96]. While killing virus-infected target cells, the balance of force between activating and inhibiting receptors serves to shield normal cells from the harmful effects of NK cells. IL-12 has the ability to activate NK cells.
NK cell levels are significantly reduced but strongly activated in COVID19 patients with severe disease relative to controls [13, 97, 98] with a preference for dim CD56dim phenotype cells over bright phenotype CD56bright cells. The pro-inflammatory and cytotoxic roles of CD56dim cells are counter-balanced by CD56bright cells. According to research, a cytokine storm that occurs during COVID-19 development may cause NK cell malfunction. Incubation of NK cells with COVID-19 plasma, particularly plasma from individuals with severe illness, causes NK cell effector capabilities to be decreased in response to K562 cell stimulation. Researchers also found indications that cytokines (like IFN and IL-6) and inhibitory checkpoint receptors (like NKG2A and TIGIT) may play a role in NK cell dysfunction in COVID-19 patients, suggesting that these molecules could be used as targets to improve NK cell activity. According to reports, at low lactate levels, distinct NK cell subsets mobilise differentially in response to aerobic exercise. During the post-exercise recovery phase, the ratio of CD56bright to CD56dim cells favours the CD56bright subgroup [99]. Acidosis caused by lactic acid inhibited the generation of IFN-γ by NK cells in many cancers, and reversing tumor acidosis increased NK cell activity and tumor cell regression [100, 101] (Fig. 5).
Dendritic Cells (DCs)
DCs are antigen-presenting cells (APCs), which have their ability to activate immune naive T cells and elicit immune response in first instance. DCs outperform macrophages and B cells when it comes to activating naive T cells. They stimulate T cells to a wide range of antigens and are found in almost all organs, excluding the brain, where they act as tissue-resident APCs. There are three types of DCs: conventional DCs (cDCs), plasmacytoid DCs (pDCs), and monocyte-derived DCs (mDCs). pDCs are an uncommon form of immune cell that secretes significant amounts of type 1 interferon in response to a viral infection and have regulatory functions, whereas cDCs control immunogenicity. In severe COVID-19 patients, CD1c+ conventional DCs transfer from the blood to the lungs, whereas CD123hi pDCs are missing in the blood and almost non-existent in the lungs [102]. However, aerobic exercise causes the opposite changes in DC differential counts in severe COVID-19 patients [90, 91]. Lactate buildup was associated with decreased DC movement into the bloodstream [103]. Tumor-derived lactic acid is also critical for modifying DC phenotype in the tumor microenvironment, and it may help with tumor-escape mechanisms [85].
Since high amounts of lactate production during high-intensity anaerobic exercise can influence NK cells, macrophages, DCs, and cytotoxic T cells, as well as immunological indicators including serum IL-6, it is recommended that other lactate-blocking strategies should be employed in inflammatory therapies, in addition to beta-blockers, for treatment of COVID-19 patients [104].
Metabolic Acidosis and Complement Activation
The Complement System
Complement is the heat labile proteinaceous component of the innate immune system, present in the blood plasma. Complement provides protection against invading microrbial pathogens through both antibody-dependent and antibody-independent mechanisms. It kills microbial pathogens by opsonisation, chemotaxis and direct cytolysis through C5b-9 membrane complex.
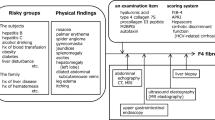
Complement also functions as a link between the immune and coagulation systems. Around 40 inactive proteins, including circulating zymogens (proteases which are activated by themselves), a fluid phase and membrane-bound regulators, and cell-bound receptors, form the complete complement system. Complement is activated through three pathways which involve these proteins: classical pathway (CP), alternate pathway (AP), and lectin pathway (LP) [105] (Fig. 6). The initial chemical complexes and triggering signals are the only differences between the CP and LP pathways [106].
Complement activation pathways: (1) Classical pathway (CP) is initiated by binding of C1 complex (C1qC1rC1s) to an Ag–Ab complex. (2) The lectin pathway (LP), similar to classical pathway, is initiated by binding of mannose-binding lectins (MBLs) to specific carbohydrate structures, present on pathogens. Both of these pathways initiate the hydrolysis of C2 and C4 and result in the formation of C2a and C4b, which form the C3 convertase (C4bC2a). C3 is further cleaved into C3b (an opsnin) and C3a (an anaphylatoxin). (3) The alternate pathway (AP) is activated when C3, a zymogen found in high concentrations in serum, undergoes spontaneous hydrolysis. C3(H2O) binds a factor B (FB), and the resulting pro-convertase complex is activated by factor D (FD), resulting in the C3 convertase C3bBb or C3(H2O)Bb. These early C3 convertases further activate AP, resulting in AP amplification. After that, the final route is triggered, resulting in C5 cleavage and the production of MAC. C3b, generated in all three pathways, opsonises the target, attaches to a C3 convertase to make [C4b2a3b or (C3b)2Bb] trimolecular C5 convertases, and generates additional C3b via AP. C5 breaks into C5a, a potent anaphylatoxin, and C5b, which starts the final lytic cascade, resulting in the formation of the complex membrane assault complex (C5b-9, MAC). Inflammation (through the AP and terminal pathways), pathogen and cell lysis (by MACs), and opsonisation (pathogen clearance and by-products of different pathways) are the end outcomes of complement activation.
The CP’s initiator complex consists of one complement C1q, one serine protease C1r, and one serine protease C1s forming C1qrs. The C1qrs complex is activated by binding to molecules such as lipopolysaccharide (LPS), viral proteins, C-reactive protein (CRP), and myelin, although it can also be activated without binding to an antigen–antibody combination. Carbohydrate recognition molecules as mannose-binding lectin (MBL), ficolins, or collectin-11 are linked with serine proteases, notably MASP-1, MASP-2, and MASP-3, to form LP-initiating complexes with pathogen [107]. The lectin pathway (LP) is activated when the carbohydrate recognition molecules of the LP recognise certain sugar patterns on the surfaces of invading microbial pathogens. Unlike CP and LP, however, AP activation is caused by an imbalance between activating and inactivating signals operating on a steady-state tick-over process [108]. AP also serves as a loop for signal amplification from the other two routes [109]. AP activation, unlike CP and LP, is triggered by an imbalance between activating and inactivating signals in a “steady-state tick-over process” [108]. AP also serves as a loop for signal amplification from the other two routes [109].
Finally, the three complement pathways come together at a C3 convertase (an enzyme) site, where C3 is cleaved into a big product, C3b, and a tiny fragment, C3a. C3a is an anaphylatoxin that causes inflammation, whereas C3b is an opsonin. When many molecules of the C3b bind to C3-convertases (either from CP/LP or AP), C5-convertase is assembled, which cleaves C5 into the strong anaphylatoxin C5a and the opsonin C5b. Target cell opsonisation with C5b permits the membrane attack complex (MAC) to be assembled from terminal complement components C6, 7, 8, and 9, which insert into target membranes and form channels that impair membrane function and induce target cell lysis [98, 110] (Fig. 6).
Effect of pH on Complement
In COVID-19 patients, the complement system has been found to cause immunological damage. The complement has received little attention in the search for effective anti-inflammatory treatment options. Complement activation is highly sensitive to metabolic pH [111, 112], and is substantially triggered at pH below 7.1. Because arterial blood pH is fixed at 7.4, complement plasma proteins in blood arteries are unlikely to be exposed to very low pH even in sick conditions. However, at the sites of inflammation, the pH drops significantly, to 6 or below [113]. This physiological reality has just recently been recognised and addressed by Kenawy et al. [114]. Chronic kidney disease (CKD) with metabolic acidosis is of special relevance, as therapeutic alkalinisation of urine after sodium bicarbonate (NaHCO3) has been found to lower tubular complement activation impact, which has substantial implications for slowing CKD progression [115, 116]. Direct pH measurements, on the other hand, have failed to support direct complement activation by acidosis. As a result, more likely explanations include AP activation and pH-sensitive cross-talk between the coagulation (contact) and complement systems [117].
LDHA: THE TARGET PROTEIN FOR COVID-19 THERAPY
LDH Isozymes
According to reports, lactate levels in the blood are a chemical indication of sickness severity in all circumstances. The final crucial stage in the anaerobic metabolism of glucose is as follows when oxygen is in inadequate quantity:
The LDHA4 isoform of lactate dehydrogenase (also called LDHA or LDH5) catalyses the formation of lactate from pyruvate (Eq. (1)), preventing pyruvate from entering the TCA cycle. The NADH oxidation process enables for the regeneration of NAD+ molecules, which are essential for glycolysis to continue producing ATP. On the other hand, the LDHB4 (LDH1) enzyme is predisposed to convert lactate to pyruvate while simultaneously creating NADH. It regenerates NAD+ during this process, which is required for glycolysis to continue [38, 48]. The oxidative phosphorylation process, which produces ATP, is disturbed in anaerobic or hypoxic environments. As a result, LDH is increased in order to meet the increased demand for energy.
Somatic LDH
The LDH family of proteins is a terminal enzyme of glycolytic pathway that is found in tissue and cell-specific patterns throughout the body. The LDHA version of the enzyme, which is translated into a 332 amino acid protein, is encoded by a gene on chromosome 11p15.4. The LDHB gene on chromosome 12p12.1 produces a 334-amino acid protein [118].
In a single cell, LDH exists in multi-molecular tetrameric forms. LDH monomers A or M (muscle type) and B or H (heart type) and their related genes (LDHA and LDHB) are found in mammalian somatic cells [118, 119]. The A and B subunits form tetramers to produce five distinct isoenzymes (LDH-1 to LDH-5), which contains either of LDHB4 (LDH-1); LDHB3:A1 (LDH-2); LDHB2:A2 (LDH-3), LDHB1:A3 (LDH-4) or LDHA4 (LDH-5) subunits. LDH isoenzyme’s 3D structure depends on the origin of tissue. LDH1 is found mostly in heart tissue, red blood cells, and kidney cells, whereas LDH5 is found primarily in hepatocytes and skeletal muscles [120]. Tissues with a stable oxygen supply (heart, brain) have a high B content, whereas tissues that create huge amounts of lactic acid, such as muscle, have a high A monomer concentration. It has been observed that the ratio of B and A monomers is regulated by the state of hypoxia in tissues [121].
The LDHA4 isoenzyme (or LDH-5) converts pyruvate to lactate with unrivalled efficiency, particularly under anaerobic conditions [119]. However, as the amount of LDHB subunits compared to LDHA subunits increases, LDH’s function steadily declines. As a result, the LDH-1 isoenzyme (LDHB4), which is made up entirely of four B subunits, efficiently promotes the backward conversion of lactate to pyruvate [38, 119].
Besides LDHA and LDHB genes, LDHC gene is expressed in testis germ cells and the LDHD gene is expressed in variety of tissues [122]. The LDHA and LDHB isoforms are present in mitochondria, plasma membrane and cytosol [122].
LDHC4 in Spermatogenic Cells
Unlike somatic LDHA and LDHB, the C subunit of LDH designated as LDHC and a product of the LDHC (Ldh-3 in murine) gene is mostly found in spermatogenic cells of the testis. LDHC is synthesised in the testis throughout sexual maturation, and it makes up the majority of mature spermatozoa [118, 123, 124]. While LDHA and LDHB are found in most somatic tissues, LDHC was detected in the testes’ germinal epithelium. The human gene loci for LDHA and LDHC have been assigned to chromosome 11, whereas LDHB has been attributed to chromosome 12. This demonstrates that LDHC and LDHA are syntenic on human chromosome 11. Phylogenetic investigations and sequence analysis revealed that the LDHA, LDHB, and LDH6B genes are found in all mammalian genomes, so far studied; however, the LDHC gene appears to have emerged more recently in marsupial mammals [118, 123].
The five isoforms of LDH in somatic cells and LDHC in the male and female reproductive tract differ in their enzyme kinetics, isoelectric point, and electrophoretic mobility, despite following the same general process. With the exception of helices αD, αE, and α2G in the area of the active centre and carboxy terminal helix H, secondary structural elements in dogfish apoLDHA and other species are essentially in the same position relative to the molecular twofold axis. As a result, the overall folding of the apo-LDHC polypeptide chain resembles that of somatic LDH, with the same α-helices and β-pleated sheets in LDHC as in other LDH isozymes [118, 123] (Fig. 7).
Three-dimensional structure of LDHA and LDHC subunits of LDH: A LDHA from tropical damselfish, mouse testis, adapted from Johns and Somero [125] (PDB code: 1LDM). B LDHC from mouse testis, adapted from Hogrefe et al. [126] (PDB code: 2LDX), showing secondary structure elements. The ThrfiAla (temperatefitropical) mutation in LDHA is indicated at position 219.
Mitochondrial LDH
Despite the fact that LDH is primarily a cytoplasmic enzyme, many studies have shown its presence in mitochondria (mLDH of yeast, plants, and mammals) [48, 118, 127, 128]. The transport of l-lactate to the mitochondria is carried out by the l-lactate/H symporter, as well as by the l-lactate/pyruvate and l-lactate/oxaloacetate antiporters. As a result, mL-LDH assists in the conversion of l-lactate to pyruvate in the mitochondrial matrix. Many cancer cells reprogramme mitochondrial activities to satisfy their increased energy demands. Glycolysis is enhanced in cancer cells, and mL-LDH may have a role in accelerating oxidative phosphorylation.
Outside the nucleus, LDHA is involved in glycolysis, but it also functions in the nucleus as a single-stranded DNA binding protein (SSB), where it is likely involved in DNA duplication and transcription. The cellular level of LDH is influenced by the metabolic needs of each tissue, such as development, biological circumstances, and pathological traits [129]. While the LDHA and LDHB genes arose from a single LDHA gene duplication, the LDHC gene is an LDHA gene duplication. The sequences of the human A and C subunits are 84–89% identical, with 69–75% amino acid identity. In mitochondria, plasma membrane, and cytosol, the LDHA and LDHB isoforms are found [122].
Clinical Relevance of Serum LDH Measurements
LDH: a Non-specific Indicator of Cellular Death
Human cells, particularly myocardial and hepatic cells, contain LDH. According to various publications, serum LDH levels are a non-specific marker of cellular death in a variety of illnesses. However, research on alterations in LDH in COVID-19 patients has not been thoroughly performed. Because serum LDH rises as a result of tissue breakdown, high serum LDH is seen in a variety of clinical disorders, including hematological disorders, cancers, tissue infarction, liver disease, congestive heart failure, and several respiratory illnesses. LDH is a multi-organ damage marker that affects more than only liver and heart function [130]. Serum LDH is a prognostic marker in patients with non-Hodgkin’s lymphoma, myeloma, and acute and chronic problems [48, 131, 132]. Drug poisoning can also cause elevated serum LDH levels. A high glycolytic activity has been linked to the development of cancer [133, 134]. LDH is released in the bloodstream by damaged tumors, where it plays a role in cancer pathogenesis. When a cell’s cytoplasmic membrane is damaged, LDH is released in many diseases.
LDH as a Predictive Marker for Immune Surveillance
Serum LDH is a metabolic as well as a prognostic biomarker for immune surveillance. Its rise in serum is associated with poor outcomes in immunocompromised patients [3] and appears to be linked to serum lactate. As already described [135], LDH promotes lactate synthesis, which enhances immune-suppressive cells like macrophages and DCs, while inhibiting cytolytic cells like NK cells and cytotoxic T lymphocytes (CTLs). When T cells are activated and proliferate, LDH is frequently induced [136]. An increase in LDH level was suggestive of a poor outcome in the investigation of a CTL that showed improved T cell activity and proliferation, indicative of inhibitory impact of LDH on CTLs. Furthermore, in the absence of LDH, CD4+ T cells released low level of IFN-γ, suggesting that LDH plays an important role in boosting T cell responses [136] (Fig. 4). Significant relationships have also been discovered between LDH and cytokines/chemokines. Low LDH activity provides anti-inflammatory effects due to downregulation of various inflammatory mediators, including cytokines and NO [137], as well as lactate fluctuation, which modulates macrophage inflammatory response [137]. Lower numbers of T cells, notably CD3+, CD4+, and CD8+ T cells, but not B or NK cells, were connected to the development of lymphocytopenia in severe patients, and an increase in LDH was substantially correlated with illness severity [138, 139]. LDH elevation, on the other hand, could be considered a predictive characteristic in severe COVID-19 individuals [139, 140].
LDH in Respiratory Disorders and SARS-CoV-2
Higher serum LDH levels have been linked to obstructive lung disease, such as bronchial asthma and chronic obstructive pulmonary disease (COPD), among other respiratory disorders [141]. Infections like pulmonary tuberculosis and the corona virus-related SARS and others have all been linked to elevated serum LDH [142]. Lung diseases such as “Idiopathic fibrosing alveolitis (Idiopathic pulmonary fibrosis, IPF), hypersensitivity pneumonitis, desquamative interstitial pneumonitis, and cryptogenic organising pneumonia (COP), previously known as bronchiolitis obliterans with organizing pneumonia (BOOP), are all associated with elevated levels of LDH” [143]. As a pathological mechanism, these diseases are linked to inflammation. A significant proportion of individuals with chronic cough, as asthma and persistent cough, which are owing to airway inflammation [144, 145], have higher serum LDH levels. When a cell’s cytoplasmic membrane is damaged, LDH is released.
Among the risk variables, LDH exhibits the strongest direct relationship with both the P/F ratio and the CT score in the lungs, indicating a clear link between lung damage and disease severity. Researchers discovered that Epstein-Barr virus (EBV)-infected B cells had more LDH transcripts than uninfected B cells in EBV-infected B cells [135, 146]. In a Zika-infected animal study, an increase in serum LDH was associated with 70% mortality [130].
LDH and Other Prognostic Markers of SARS-CoV-2 Infection
Several systemic reviews and meta-analyses have reported the prognostic value of laboratory data for severity of COVID-19. LDH and CRP have been related to respiratory function (PaO2/FiO2) and a predictor of respiratory failure in CoVID-19 patients by Poggiali et al. [147], where (PaO2/FiO2) is the ratio of arterial partial pressure of oxygen (PaO2) to fraction of inspired oxygen (FiO2). Lymphocytopenia in severe patients is produced primarily by a decrease in T lymphocyte subsets, notably CD3+, CD4+, and CD8+ T lymphocytes, in COVID-19 patients’ blood, which is found to be connected with illness severity. Lymphocytopenia, on the other hand, is not a strong predictor of ICU admission, ARDS, or mortality, despite having a high leukocyte count and a high level of LDH. According to studies, LDH is the only best measure that may predict ICU admission or fatality situations. LDH increase up to sixfold in COVID-19 patients with severe disease related up to 16-fold increase in fatality [148,149,150,151,152]. Serum LDH levels in diabetic COVID-19 patients aged 70 or older also predicted fatality.
Other Prognostic Markers of SARS-CoV-2 Infection
Both, severe and fatal COVID-19 patients show high levels of IL-6 and IL-10, as well as serum ferritin [148]. Increased leukocyte count, increased transaminases, elevated LDH, and increased procalcitonin all predicted ICU admission in the meta-regression [148,149,150]. Low lymphocyte counts, as well as blood levels of CRP, D-dimers, ferritin, cardiac troponin, as well as LDH, can be utilised to predict severity and death in COVID-19 patients admitted to the ICU [148, 151]. In some studies, patients with severe CoV-2 infection showed increased symptoms of liver impairment [152], which could be linked to cytokine storm, as well as pneumonia-related hypoxia in critically ill COVID-19 patients [149, 153]. In non-survivors, aberrant coagulation parameters have been linked to a poor prognosis (Table 1). In comparison to survivors, non-survivors have considerably greater amounts of plasma D-dimers and fibrin breakdown products, as well as longer prothrombin times and activated partial thromboplastin times [154]. The best independent predictor of mortality was D-dimer elevation > 1 µg/L [155, 156]. In severely ill patients, elevated cardiac troponin I levels, which indicate heart injury, were also predictive of mortality [155, 157].
LDH in Cancer
Cancer being inflammatory metabolic disease, many cancers rely on LDH for their progression and survival. LDHA is engaged in the metabolism of key nutrients like glucose and glutamine, as well as determining tumor pH and TCA cycle activity, as it is implicated at a vital stage in metabolism [169, 170]. Cancer is now thought to be a metabolic illness in which rapidly multiplying cancer cells reprogram metabolic pathways across tumor microenvironments (TME). The TME, which is a complex dynamic biological environment, is made up of tumor cells, stromal cells, blood vessels, ECM, growth factors, and cellular metabolites [171]. The TME is reprogrammed by cross-talk between ECM components and cancer cells, allowing cancer cells to meet their high metabolic demands while also impacting tumor growth. Cancer cells can benefit from molecular reprogramming because it helps them meet their greater metabolic needs for bioenergetics and cellular production. LDH is critical in controlling food exchange between tumor and stromal cells in such a TME [172,173,174] (Fig. 2).
The LDHA isoenzyme has been found to be increased in different types of tumors [129, 149, 155]. Isoenzymes B and C are only expressed in particular cancers [168, 175,176,177,178]. The c-myc and HIF1- α, both of which are typically overexpressed in many malignancies, boost LDHA expression. AKT, MYC, and HIF-1 are all carcinogenic molecules that can contribute to the metabolic shift that happens during carcinogenesis. Haas et al. [63] explored the mechanisms that cause metabolic shift as well as different explanations for its occurrence [63, 70].
ENZYMES AS A SPECIAL CLASS OF THERAPEUTIC TARGETS
Multistep chemical reactions are catalysed by enzymes, which attain extraordinary rates of acceleration. Drugs that operate on enzymes can either inhibit or activate them, with inhibition being the more typical mode of action. By inhibiting the enzyme–substrate interaction competitively, non-competitively, or uncompetitively, drugs that inhibit enzymes impede the production of the product. Enzyme catalysis is crucial for designing effective inhibitors, making them a unique therapeutic target. Enzymes as mitogen-activated protein kinase, renin and dipeptidyl peptidase IV are important drug targets. Drugs that target these enzymes (enzyme inhibitors or activators) target functional groups of enzymes [179,180,181,182,183]. The most researched pharmacological targets are transmembrane receptors connected to enzymes, commonly employed in oncology and immunology [180]. Lipogenic enzyme inhibitors have also been investigated as a possible cancer treatment [181].
Proteolytic Enzymes and Their Inhibitors
Several proteolytic enzymes help to control and coordinate virus entry in the virus machinery in host cells, which could be useful in COVID-19. Serratiopeptidase (SEPD), also known as Serratia E-15 protease and serrapeptase, has recently gained popularity. SEPD, a serine protease super, is produced in the silkworm’s intestine. Because of its wide spectrum of therapeutic actions, including anti-inflammatory, antibacterial, atheroprotective, antithrombotic, and fibrinolytic qualities, SEPD has an edge over other COVID-19 treatments. SEPD has long been utilised to treat joint pain and inflammation, as well as sports-related sprains. Inhibition of elastase by SEPD may be helpful in controlling the cytokine storm that causes acute lung damage in COVID-19. SEPD-mediated elastase inhibition in the airways may also reduce airway inflammation [182].
TMPRSS2
CoV-2 cell entrance is dependent on the viral spike (S) protein binding to the host cell proteases TMPRRS2 and ACE2. CoV-2 viral study has revealed that the virus interacts with the transmembrane protease TMPRSS2, allowing it to enter the cell more easily. As a result, blocking this interaction could be a feasible treatment option for COVID-19 infection. The quest for inhibitors makes this a suitable target for respiratory viral infection treatment.
Camostat mesylate, a clinically established serine protease inhibitor, is being tested in a number of trials against SARS-CoV-2. Camostat mesylate partially prevents S protein-driven entry into TMPRSS2-expressing human lung cells, but has no effect on TMPRSS2-knockout cells [183]. Other TMPRSS2 inhibitors being studied include nafamostat, which can prevent SARS-CoV-2 membrane fusion, and bromhexine, a mucolytic cough suppressant, combined with hydroxychloroquine, a competitive inhibitor of viral-ACE2 binding.
SARS-CoV-2 entry and activation can be mediated by both endosomal (such as cathepsin L) and non-endosomal pathways, depending on the accessibility of the cellular proteases required for SARS-S activation. The viral S protein is broken by the furin enzyme in infected host cells in the non-endosomal pathway as per evidence. Host protease inhibition has been employed as a treatment method for viral infection, according to [184].
A different approach is to breakdown the host cell machinery that allows the virus to infect the host cell and prevent its reproduction. Host cell proteases, which have been implicated in viral pathogenesis in a number of coronaviruses, are examples of such machinery.
Importance of LDH in Covid-19
LDH is a cytosolic enzyme that aids in the synthesis of energy in the human body. However, the major goal of analysing LDH in blood is to see if there is any tissue damage in the body. Injury and inflammation in the heart, lungs, liver, muscle, or kidneys are few of the tissue damage disorders that can develop. In such instances, LDH test is recommended in patients. In patients who have been infected with SARS-COV-2, it can aid in the prediction of acute respiratory distress syndrome.
LDH INHIBITORS AS ANTI-INFLAMMATORY AGENTS: REGULATION OF GLYCOLYSIS AND METABOLIC ACIDOSIS
LDH is a promising biomarker, especially as elevated LDH levels have previously been linked to poor outcomes in patients with various viral illnesses including COVID-19, hence a potential therapeutic target for a variety of tumors [185] as well as a target for infectious diseases. Importantly, lymphocytes and LDH levels in COVID-19 patients’ blood have been linked to disease severity. The greater the leukocyte count and the LDH, the greater the chance of death. In COVID-19 patients with severe illness, LDH levels increased up to sixfold, with a 16-fold increase in mortality [148]. In relation to COVID-19, we emphasise the importance of small molecule inhibitors or their combination in targeting LDH activity and developing safe therapy as studied in cancer [186]. A vast number of these compounds have been discovered. The findings clarified ambiguities in two well-known LDHA inhibitors’ modes. MIA PaCa-2 and HT29, two glycolytic cancer models, were proven in vivo by Oshima et al. Within 30 min of LDH inhibition, HP-MRSI demonstrated a metabolic rewiring in vivo, in which pyruvate in a tumor is diverted toward mitochondrial metabolism [187].
Oxamate
Oxamate, a pyruvate analogue and a competitive LDH inhibitor, affects cell glycolysis by directly inhibiting LDH’s conversion of pyruvate to lactate. Because glycolysis and mitochondrial oxidative phosphorylation are linked processes [185], and LDHA regulates glycolysis and growth in breast cancer cells, it was assumed that increased LDHA expression and activity in Taxol-resistant cells would result in increased glycolysis and decreased mitochondrial oxidative phosphorylation. This supports the hypothesis that oxamate increases Taxol sensitivity by reducing cellular glycolysis [188].
In lymphoma cells, Hoffmann et al. found that inhibiting LDHA with oxamate inhibited tumor development via increased apoptosis and the formation of reactive oxygen species (ROS) [183]. Oxamate decreased ATP levels while increasing cancer radiation sensitivity [189,190,191]. By blocking the CDK1/cyclin B1 pathway, oxamate suppression of LDH produced G2/M cell cycle arrest and encouraged death by increasing mitochondrial ROS generation. For the therapy of nasopharyngeal cancer cells, LDHA is an appropriate therapeutic target [189]. Miskimins et al. discovered that oxamate and phenformin have a synergistic anti-cancer effect by inhibiting complex I in mitochondria and LDH in the cytosol at the same time [192].
Gossypol
“((2,2′-Binaphthalene)-8,8′-dicarboxaldehyde, 1,1′,6,6′,7,7′-hexahydroxy-5,5′-diisopropyl-3,3′-dimethyl)” is a lipid-soluble polyphenol isolated from cotton plant (genus Gossypium) and the tropical tree Thespesia populnea (L.). Gossypol is present in cotton seed oil. With respect to both NADH and pyruvate, gossypol acts as a competitive inhibitor of all LDH isozymes [127, 193]. Gossypol can reduce temozolomide-resistant glioblastoma by inhibiting numerous dehydrogenases in metabolic pathways [194].
Gossypol has a comparable affinity for the Bcl2 (B-cell lymphoma 2) family of proteins, and it can trigger apoptosis in tumor cells that display high levels of Bcl-XL and/or Bcl-2, whereas normal cells are unaffected [195]. The racemic mixture of two enantiomers is formed by (+)-gossypol and (-)-gossypol. (-)-Gossypol, also known as AT-101, has a higher affinity for Bcl-XL, Bcl-2, and Mcl-1 than (+)-gossypol, making it a more potent apoptosis inducer [195, 196].
“3-Dihydroxy-6-methyl-7-(phenylmethyl)-4 propylnaphthalene-1-carboxylic acid” (FX11, a chemical derived from gossypol) is a recognised malarial LDH inhibitor and a competitive inhibitor of LDHA in terms of NADH binding, causing ATP depletion and severe oxidative stress [184, 197]. Lactate levels were lowered, which inhibited the inflammatory response generated by macrophage LPS. Due to decreased tissue lactate, the production of cytokines, inducible nitric oxide synthase (iNOS), and cyclooxygenase 2 (COX 2) was downregulated in murine macrophages treated with FX11. Clinical trials for gossypol/AT-101 are now underway; however, clinical trials for FX11 have yet to commence.
Galloflavin
Galloflavin (GF), a synthetic chemical, inhibits LDHA by binding preferentially to free enzymes without competing with substrates or cofactors [198] and without altering mitochondrial respiration. By limiting aerobic glycolysis and ATP synthesis, GF reduced cancer cell proliferation [198, 199]. In vitro, GF disrupted LDHA/ssDNA connections and inhibited RNA synthesis, pointing to a complex mechanism underpinning its toxicity to cancer cells [199]. GF has the potential to be a two-edged therapy for Covid-19, reducing glycolysis and iRNA synthesis as well as CoV-2 replication.
Other Small Molecules as LDH Inhibitors
Hydroxychloroquine (HCQ) is a medication that is commonly used to treat autoimmune illnesses such arthritis and SLE, has been attempted to treat COVID-19. LDH activity is suppressed by HCQ. Having its low toxicity relative to its closely related molecule chloroquine, it is also prescribed for the treatment of malaria. P. falciparum LDH (PfLDH) and human LDH have highly comparable biological functions. Any medication aimed at inhibiting PfLDH has the potential to influence human LDH activity [200, 201].
Kim et al. discovered that selenobenzene compounds have LDHA inhibitory characteristics [202] and the most effective inhibitor was 1-(phenylseleno)-4-(trifluoromethyl) benzene (PSTMB). It slowed the growth of a number of cancer cell lines and efficiently suppressed LDHA activity and lactate [202]. EWS-FLI1 inhibits LDHA expression and results in genetic depletion of LDHA and decreased EWS cell growth, and death [203]. Phthalimide and dibenzofuran compounds are new LDH inhibitors, which selectively inhibit LDHA isoenzyme [186, 204]. Quinoline-3-sulfonamides compete with NADH and have a higher selectivity for LDHA than LDHB [205].
Suppression of LDH by Small Interfering RNAs
Small interfering RNAs (siRNAs) are double-stranded non-coding RNA molecules having 20–25 nucleotides and can target sequence complementarity to suppress gene expression. Inhibition of gene expression by siRNA is predicted to be an important technique in medication development in the future [206]. The use of siRNAs to target LDHA has been examined as a means to prevent cancer formation [207,208,209,210]. The expression of IL 6 and nitrites were reduced when LDHA was genetically suppressed by siRNAs. The phosphorylation of p38 mitogen-activated protein kinase was decreased by genetic suppression of LDHA. The findings suggested that LDH is a key target in the control of the inflammatory response by siRNAs. Inhibition of LDHA by siRNA causes oxidative stress and cell death, suggesting that it could be a useful therapy for LDHA-dependent malignancies [64]. Small chemical inhibitors or non-coding RNA approaches to inhibit LDHA and LDHB expression are of major attention, as they may interfere with cancer and COVID-19 progression. LDHA knockdown in glioblastoma cells reduced cell growth, decreased glycolysis, and enhanced apoptosis [209]. The loss of LDHA overexpression inhibited colorectal cancer growth and decreased lactate levels [207].
Besides siRNA, short hairpin RNA (shRNA) also decreased tumorigenicity and lowered LDHA expression in neuroblastoma cells without affecting aerobic glycolysis. ShRNA-mediated LDHA attenuation has been shown to result in a decrease in mitochondrial membrane potential and a reduced ability to proliferate under hypoxia, in addition to increasing mitochondrial respiration.
Compounds with Unknown Mechanisms
In pancreatic tumors, where LDHA is acetylated at lysine 5, post-translational modification increases its expression. This acetylation lowers the catalytic activity of LDHA. Endogenous acetylated LDHA replacement reduces cancer cell proliferation and migration, implying that LDHA acetylation is important for cell growth control [210]. LDHA inhibitors GNE140, a piperidine derivative, and gall, a natural extract, have been reported to be beneficial in cancer treatment [211]. N-hydroxyindoles (NHI) are more selective for LDHA than LDHB and can reduce cancer cell proliferation [185], while genetic or drug suppression of LDHA can reverse osteosarcoma development in children [212]. Through docking-based virtual screening, Fang et al. discovered LDHA inhibitors. In MG-63 cancer cells, compound 11 caused apoptosis, increased oxygen consumption, and lowered lactate production and extracellular acidification rates. Compound 11 appears to be a viable candidate for developing powerful LDHA inhibitors [213]. In a pilot study, pentoxifylline increased lymphocyte counts and a decreased serum LDH. Maldonado rebranded pentoxifylline as a COVID-19 therapy medication. This evidence, however, must be validated in a subsequent trial [214].
CONCLUSIONS
With aberrant bioenergetic metabolism, infectious and other inflammatory illnesses are always changing. Inflammatory illnesses have the ability to reprogram metabolic pathways to meet increased nutritional needs in order to promote cell proliferation at a high pace. The glycolytic pathway is frequently disrupted in several types of inflammatory illnesses to satisfy the increased bioenergetic and metabolic demand. Lactate, the product of anaerobic metabolism, is continuously produced and used by numerous types of cells in fully reprogrammed aerobic inflammatory diseases. Lactate is primarily produced in the human body from glucose. LDH, the final enzyme in the glycolytic pathway and a generator of lactate, is a promising biomarker, especially since elevated LDH intensity has been related to poorer outcomes in cancer patients and viral infections like SARS-CoV-2.
Availability of Data and Material
Permissions attached where required.
Code Availability
Not applicable.
References
Lai, C.C., T.P. Shih, W.C. Ko, H.J. Tang, and P.R. Hsueh. 2020. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and Coronavirus disease-2019 (COVID-19): The epidemic and the challenges. International journal of antimicrobial agents 55: 105924.
Denson, J.L., A.S. Gillet, Y. Zu, M. Brown, T. Pham, Y. Yoshida, et al. 2021. Metabolic Syndrome and Acute Respiratory Distress Syndrome in Hospitalized Patients With COVID-19. JAMA Network Open 2021 (4): e2140568. https://doi.org/10.1001/jamanetworkopen.2021.40568.
Lim, S., J.H. Bae, and H.S. Kwon. 2021. Nauck MA COVID-19 and diabetes mellitus: From pathophysiology to clinical management. Nature Reviews Endocrinology 17: 11–30.
Zhong, K., Y. Yi, and W. Wei. 2020. Clinical characteristics and prognosis of community acquired pneumonia in autoimmune disease induced immunocompromised host: A retrospective observational study. World Journal of Emergency Medicine 11: 136–140.
Li, H., S.-M. Liu, X.-H. Yu, S.-L. Tang, and C.-K. Tang. 2020. Coronavirus disease 2019 (COVID-19): Current status and future perspectives. International Journal of Antimicrobial Agents 55: 105951.
Choi, J.Y., and D.M. Smith. 2021. SARS-CoV-2 Variants of Concern. Yonsei medical journal 62: 961–968. https://doi.org/10.3349/ymj.2021.62.11.961.
Li, M.Y., L. Li, Y. Zhang, and X.S. Wang. 2020. Expression of the SARS-CoV-2 cell receptor gene ACE2 in a wide variety of human tissues. Infectious Diseases of Poverty 9: 45. https://doi.org/10.1186/s40249-020-00662-x.
Wang, Q., Y. Zhang, L. Wu, S. Niu, C. Song, Z. Zhang, et al. 2020. Structural and functional basis of SARS-CoV-2 entry by using human ACE2. Cell 181: 894–904.
Mishra, S., G. Bassi, and B.L.G. Nyomba. 2021. Inter-proteomic posttranslational modifications of the SARS-CoV-2 and the host proteins - A new frontier. Experimental Biology and Medicine 246: 749–757.
Lu, G., Q. Wang, and G.F. Gao. 2015. Bat-to-human: Spike features determining ‘host jump’ of coronaviruses SARS-CoV, MERS-CoV, and beyond. Trends in Microbiology 23: 468–478.
Partridge, L.J., L. Urwin, M.J.H. Nicklin, D.C. James, L.R. Green, and P.N. Monk. 2021. ACE2-Independent interaction of sars-cov-2 spike protein with human epithelial cells is inhibited by unfractionated heparin. Cells 10: 1419.
Trougakos, I.P., K. Stamatelopoulos, E. Terpos, O.E. Tsitsilonis, E. Aivalioti, D. Paraskevis, et al. 2021. Insights to SARS-CoV-2 life cycle, pathophysiology, and rationalized treatments that target COVID-19 clinical complications. Journal of Biomedical Science 28: 9.
Gupta, A., and G.S. Gupta. 2021. Status of mannose-binding lectin (MBL) and complement system in COVID-19 patients and therapeutic applications of antiviral plant MBLs. Molecular and Cellular Biochemistry 476: 2917–2942.
Gao, Y.-L., Y. Du, C. Zhang, C. Cheng, H.-Y. Yang, Y.-F. Jin, et al. 2020. Role of renin-angiotensin system in acute lung injury caused by viral infection. Infection and Drug Resistance 13: 3715–3725.
Chen, Y., K. Shan, and W. Qian. 2020. Asians and other races express similar levels of and share the same genetic polymorphisms of the SARS-CoV-2 cell-entry receptor. Preprints. https://doi.org/10.20944/preprints202002.0258.v1.
Zhuang, M.-W., Y. Cheng, J. Zhang, X.-M. Jiang, L. Wang, J., Deng, and P.H. Wang. 2020. Increasing host cellular receptor-angiotensin-converting enzyme 2 (ACE2) expression by coronavirus may facilitate 2019-nCoV infection. Journal of medical virology. https://doi.org/10.1002/jmv.26139.
Wang, C., S. Wang, D. Li, X. Zhao, S. Han, and T. Wang. 2020. Lectin-like intestinal defensin inhibits 2019-nCoV spike binding to ACE2. biorxiv. https://doi.org/10.1101/2020.03.29.013490v1.
Gkogkou, E., G. Barnasas, K. Vougas, and I.P. Trougakos. 2020. Expression profiling meta-analysis of ACE2 and TMPRSS2, the putative anti-inflammatory receptor and priming protease of SARS-CoV-2 in human cells, and identification of putative modulators. Redox Biology 36: 101615. https://doi.org/10.1016/j.redox.2020.101615.
Donoghue, M., F. Hsieh, E. Baronas, K. Godbout, M. Gosselin, et al. 2000. A novel angiotensin-converting enzyme–related carboxypeptidase (ACE2) converts angiotensin I to angiotensin 1–9. Circulation Research 87: e1–e9. https://doi.org/10.1161/01.RES.87.5.e1.
Pahwa, R., A. Goyal, and I. Jialal. 2021. Chronic Inflammation. NCBI.
da Silva, D.M., H. Langer, and T. Graf. 2019. Inflammatory and Molecular Pathways in Heart Failure-Ischemia, HFpEF and Transthyretin Cardiac Amyloidosis. International Journal of Molecular Sciences 20: 2322.
Zhang, X., X. Wu, Q. Hu, J. Wu, G. Wang, Z. Hong, and J. Ren. 2019. Lab for Trauma and Surgical Infections. Mitochondrial DNA in liver inflammation and oxidative stress. Life Sciences 236: 116464.
Soto-Heredero, G., M.M. Gómez de las Heras, E. Gabandé-Rodríguez, J. Oller, and M. Mittelbrunn. 2020. Glycolysis – a key player in the inflammatory response. FEBS Journal 287: 3350–3369.
Palmieri, E.M., M. Gonzalez-Cotto, W.A. Baseler, L.C. Davies, B. Ghesquière, et al. 2020. Nitric oxide orchestrates metabolic rewiring in M1 macrophages by targeting aconitase 2 and pyruvate dehydrogenase. Nature Communications 11: 698. https://doi.org/10.1038/s41467-020-14433-78.
Greten, F.R., and S.I. Grivennikov. 2019. Inflammation and Cancer: Triggers, Mechanisms, and Consequences. Immunity 51: 27–41. https://doi.org/10.1016/j.immuni.2019.06.025.
Lim, S., J.H. Bae, H.-S. Kwon, and M.A. Nauck. 2021. COVID-19 and diabetes mellitus: From pathophysiology to clinical management. Nature Reviews Endocrinology 17: 11–30.
Tay, M.Z., C.M. Poh, L. Rénia, P.A. MacAry, and L.F.P. Ng. 2020. The trinity of COVID-19: Immunity, inflammation and intervention. Nature Reviews Immunology 20: 363–374.
Ratter, J.M., H.M.M. Rooijackers, G.J. Hooiveld, A.G.M. Hijmans, de Galan, et al. 2018. In vitro and in vivo Effects of lactate on metabolism and production of human primary PBMCs and monocytes. Frontiers in Immunology 12 (9): 2564. https://doi.org/10.3389/fimmu.2018.02564.
Nechipurenko, Y.D., D.A. Semyonov, I.A. Lavrinenko, D.A. Lagutkin, E.A. Generalov, et al. 2021. The Role of acidosis in the pathogenesis of severe forms of COVID-19. Biology 10: 852. https://doi.org/10.3390/biology10090852.
Santos, A.F., P. Póvoa, P. Paixão, A. Mendonça, and L. Taborda-Barata. 2021. Changes in glycolytic pathway in SARS-COV 2 infection and their importance in understanding the severity of COVID-19. Frontiers in Chemistry 10. https://doi.org/10.3389/fchem.2021.685196.
Krishnan, S., H. Nordqvist, A.T. Ambikan, .S Gupta, M. Sperk, S. Svensson-Akusjärvi, et al. 2021. Metabolic perturbation associated wth COVID-19 disease severity and SARS-CoV-2 replication. Molecular & Cellular Proteomics 20: 100159. https://doi.org/10.1016/j.mcpro.2021.100159.
Warburg, O. 1956. On the origin of cancer cells. Science 123 (3191): 309–314.
Bost, P., F. De Sanctis, S. Canè, S. Ugel, K. Donadello, M. Castellucci, et al. 2021. Deciphering the state of immune silence in fatal COVID-19 patients. Nature Communications 12: 1428.
Blanco-Melo, D., B.E. Nilsson-Payant, W.-C. Liu, S. Uhl, D. Hoagland, et al. 2020. Imbalanced host response to SARS-CoV-2 drives development of COVID-19. Cell 181: 1036-1045.e9.
Silva, M.A., A.R.P. Alves da Silva, M.A. do Amaral, M.G. Fragas, and N.O.S. Câmara. 2021. Metabolic alterations in SARS-CoV-2 infection and its implication in kidney dysfunction. Frontiers in Physiology 12: 624698. https://doi.org/10.3389/fphys.2021.624698.
Ardestani, A., and Z. Azizi. 2021. Targeting glucose metabolism for treatment of COVID-19. Signal Transduction and Targeted Therapy 6: 112. https://doi.org/10.1038/s41392-021-00532-4.
Li, S., F. Ma, T. Yokota, G. Garcia, A. Palermo Jr., Y. Wang, et al. 2021. Metabolic reprogramming and epigenetic changes of vital organs in SARS-CoV-2–induced systemic toxicity. JCI Insight 2021 (6): e145027. https://doi.org/10.1172/jci.insight.145027.
Mansour, K., M. Rastegari-Pouyani, M. Ghanbri-Movahed, M. Safarzadeh, S. Sara Kiani, and Z. Ghanbari-Movahed. 2020. Can a metabolism-targeted therapeutic intervention successfully subjugate SARS-COV-2? A scientific rational. Biomedicine & Pharmacotherapy 131: 110694. https://doi.org/10.1016/j.biopha.2020.110694.
Ganesh, G.V., and R.K. Mohanram. 2021. Metabolic reprogramming and immune regulation in viral diseases. Reviews in medical virology. https://doi.org/10.1002/rmv.2268.
Codo, A.C., G. Gasta, L.-D. Davanzo, B. Monteiro L-d, G.E. de Souza, et al. 2020. Eevated glucose levels favor sars-cov-2 infection and monocyte response through a HIF-1a/glycolysis-dependent axis. Cell Metabolism 32: 437–446.
Wang, Z., L. Zhang, D. Zhang, R. Sun, Q. Wang, and X. Liu. 2015. Glycolysis inhibitor 2-deoxy-D-glucose suppresses carcinogen-induced rat hepatocarcinogenesis by restricting cancer cell metabolism. Molecular medicine reports 11: 1917–1924.
Steenblock, C., P.E.H. Schwarz, B. Ludwig, A. Linkermann, P. Zimmet, and K. Kulebyakin. 2021. COVID-19 and metabolic disease: mechanisms and clinical management. The lancet Diabetes & endocrinology 9: 786–798. https://doi.org/10.1016/S2213-8587(21)00244-8.
Wang, Q., P. Fang, R. He, M. Li, H. Yu, et al. 2020. O-GlcNAc transferase promotes influenza A virus-induced cytokine storm by targeting interferon regulatory factor-5. Science Advances 6 (16): eaaz7086. https://doi.org/10.1126/sciadv.aaz7086.
Nardacci, R., F. Colavita, C. Castilletti, D. Lapa, G. Matusali, et al. 2021. Evidences for lipid involvement in SARS-CoV-2 cytopathogenesis. Cell Death & Disease 12: 263. https://doi.org/10.1038/s41419-021-03527-9.
Wu, D., T. Shu, X. Yang, J.-X. Song, M. Zhang, et al. 2020. Plasma metabolomic and lipidomic alterations associated with COVID-19. National Science Review 7: 1157–1168. https://doi.org/10.1093/nsr/nwaa086.
Thomas, T., D. Stefanoni, J.A. Reisz, T. Nemkov, L. Bertolone, et al. 2020. COVID-19 infection alters kynurenine and fatty acid metabolism, correlating with IL-6 levels and renal status. JCI Insight 5 (14): e140327.
Brooks, G.A. 2018. The Science and translation of lactate shuttle theory. Cell Metabolism 27: 757–785.
Gupta, G.S. 2017. Lactate: Metabolic hallmark of cancer in 21st century. Clinics in Oncology 2: 1375–1377.
Mauro, C., and F.M. Marelli-Berg. 2012. T cell immunity and cardiovascular metabolic disorders: Does metabolism fuel inflammation? Frontiers in Immunology 3: 173. https://doi.org/10.3389/fimmu.2012.00173.
Robergs, R.A., F. Ghiasvand, and D. Parker. 2004. Biochemistry of exercise-induced metabolic acidosis. American Journal of Physiology: Regulatory, Integrative and Comparative Physiology 287: R502-516.
de la Cruz-López, K.G., L.J. Castro-Muñoz, D.O. Reyes-Hernández, A. García-Carrancá, and J. Manzo-Merino. 2019. Lactate in the regulation of tumor microenvironment and therapeutic approaches. Frontiers in Oncology 9: 1143. https://doi.org/10.3389/fonc.2019.01143.
Pucino, V., M. Certo, V. Bulusu, D. Cucchi, K. Goldmann, E. Pontarini, et al. 2019. Lactate buildup at the site of chronic inflammation promotes disease by inducing CD4+ T Cell Metabolic Rewiring. Cell Metabolism 30: 1055–1074.
Hashimoto, T., R. Hussien, S. Oommen, K. Gohil, and G.A. Brooks. 2007. Lactate sensitive transcription factor network in L6 cells: Activation of MCT1 and mitochondrial biogenesis. The FASEB Journal 21: 2602–2612.
Zhang, D., Z. Tang, H. Huang, G. Zhou, C. Cui, et al. 2019. Metabolic regulation of gene expression by histone lactylation. Nature 574 (7779): 575–580.
Kraut, J.A., and N. E. Madias. 2014. Lactic Acidosis. New England Journal of Medicine 371: 2309–2319.
Kamel, K.S., M.S. Oh, and M.L. Halperin. 2020. L-lactic acidosis: Pathophysiology, classification, and causes; emphasis on biochemical and metabolic basis. Kidney International 97: 75–88.
De Saedeleer, C.J., T. Copetti, P.E. Porporato, J. Verrax, O. Feron, and P. Sonveaux. 2012. Lactate activates HIF-1 in oxidative but not in Warburg-phenotype human tumor cells. PLoS ONE 7: e46571.https://doi.org/10.1371/journal.pone.0046571.
Hirschhaeuser, F., U.G. Sattler, and W. Mueller-Klieser. 2011. Lactate: A metabolic key player in cancer. Cancer Research 71: 6921–6925.
Gotmaker, R., S.L. Peake, A. Forbes, R.A.R.I.S.E. Bellomo, and Investigators. 2017. Mortality is greater in septic patients with hyperlactatemia than with refractory hypotension. Shock 48: 294–300.
Tapia, P., D. Soto, A. Bruhn, L. Alegría, N. Jarufe, et al. 2015. Impairment of exogenous lactate clearance in experimental hyperdynamic septic shock is not related to total liver hypoperfusion. Critical Care 19: 188.
Andersen, L.W., J. Mackenhauer, J.C. Roberts, K.M. Berg, M.N. Cocchi, and M.W. Donnino. 2013. Etiology and therapeutic approach to elevated lactate. Mayo Clinic Proceedings 88: 1127–1140.
NardI, G., G. Sanson, L. Tassinari, G. Guiotto, A. Potalivo, J. Montomoli, and F. Schiraldi. 2020. Lactate arterial-central venous gradient among COVID-19 patients in ICU: a potential tool in the clinical practice. Critical Care Research and Practice 2020: 4743904. https://doi.org/10.1155/2020/4743904.
Haas, R., J. Smith, V. Rocher-Ros, S. Nadkarni, T. Montero-Melendez, F. D’Acquisto, et al. 2015. Lactate regulates metabolic and proinflammatory circuits in control of T cell migration and effector functions. PLoS biology 13 (7): e1002202. https://doi.org/10.1371/journal.pbio.1002202.
Nalos, M., G. Parnell, R. Robergs, D. Booth, A.S. McLean, and B.M. Tang. 2016. Transcriptional reprogramming of metabolic pathways in critically ill patients. Intensive Care Medicine Experimental 4: 21.
Ryan, J.J., L.A. Hoeferlin, C.E. Chalfant, and H. Caslin. 2019. Lactic acid suppresses LPS-induced mast cell cytokine production by limiting glycolysis and ATP availability. The Journal of Immunology 202 (1 Supplement): 64.9.
Chhetri, S., F. Khamis, N. Pandak, H.A.I. Khalili, E. Said, and E. Petersen. 2020. A fatal case of COVID-19 due to metabolic acidosis following dysregulate inflammatory response (cytokine storm). IDCases 21: e00829.
Gatenby, R.A., and R.J. Gillies. 2008. A microenvironmental model of carcinogenesis. Nature Reviews Cancer 8: 56–61.
Elstrom, R.L., D.E. Bauer, M. Buzzai, et al. 2004. Akt stimulates aerobic glycolysis in cancer cells. Cancer Research 64: 3892–3929.
Kozlov, A.M., A. Lone, D.H. Betts, et al. 2020. Lactate preconditioning promotes a HIF-1α-mediated metabolic shift from OXPHOS to glycolysis in normal human diploid fibroblasts. Science and Reports 10: 8388.
Colegio, O.R., N.Q. Chu, A.L. Szabo, T. Chu, A.M. Rhebergen, et al. 2014. Functional polarization of tumor associated macrophages by tumor-derived lactic acid. Nature 513: 559–563.
Luo, Y., L. Li, X. Chen, H. Gou, K. Yan, et al. 2021. Effects of lactate in immunosuppression and inflammation: Progress and prospects. International Reviews of Immunology 41: 19–29. https://doi.org/10.1080/08830185.2021.1974856.
Yang, K., J. Xu, M. Fan, F. Tu, X. Wang, T. Ha, D.L. Williams, and C. Li. 2020. Lactate suppresses Pro-Inflammatory Response to LPS Stimulation by Inhibition of YAP and NF-κB Activation via GPR81-Mediated Signaling. Frontiers in Immunology.https://doi.org/10.3389/fimmu.2020.587913.
Stone, S.C., R.A.M. Rossetti, K.L.F. Alvarez, I.P. Carvalho, P.F.R. Margarido, et al. 2019. Lactate secreted by cervical cancer cells modulates macrophage phenotype. Journal of Leukocyte Biology 105: 1041–1054.
O’Neill, A.J., R.J. Kishton, and J. Rathmell. 2016. A guide to immunometabolism for immunologists. Nature Reviews Immunology 16: 553–565.
Lee, Y.S., J. Wollam, and J.M. Olefsky. 2018. An integrated view of immunometabolism. Cell 172: 22–40.
Gerriets, V.A., and J.C. Rathmell. 2012. Metabolic pathways in T cell fate and function. Trends in Immunology 33: 168–173.
Finlay, D.K. 2012. Regulation of glucose metabolism in T cells: New insight into the role of Phosphoinositide 3-kinases. Frontiers in Immunology 3: 247.
McGill, J., and K.L. Legge. 2009. Cutting edge: Contribution of lung-resident T cell proliferation to the overall magnitude of the antigen-specific CD8 T cell response in the lungs following murine influenza virus infection. The Journal of Immunology 183: 4177–4181.
Beiter, T., A. Fragasso, D. Hartl, and A.M. Nieß. 2015. Neutrophil extracellular traps: A walk on the wild side of exercise immunology. Sports Medicine 11 (45): 625–640.
Jordan, R.E., P. Adab, and K.K. Cheng. 2020. Covid-19: Risk factors for severe disease and death. BMJ 368: m1198.
Mueller, S.N., K.A. Hosiawa-Meagher, B.T. Konieczny, B.M. Sullivan, M.F. Bachmann, et al. 2007. Regulation of homeostatic chemokine expression and cell trafficking during immune responses. Science 317: 670–674.
Tran, E., P.F. Robbins, and S.A. Rosenberg. 2017. “Final common pathway” of human cancer immunotherapy: Targeting random somatic mutations. Nature Immunology 18: 255–262.
Hinrichs, C.S., R. Spolski, C.M. Paulos, L. Gattinoni, K.W. Kerstann, et al. 2008. IL-2 and IL-21 confer opposing differentiation programs to CD8+ T cells for adoptive immunotherapy. Blood 111: 5326–5333.
Hermans, D., S. Gautam, J.C. García-Cañaveras, D. Gromer, S. Mitra, R. Spolski, et al. 2020. Lactate dehydrogenase inhibition synergizes with IL-21 to promote CD8+ T cell stemness and antitumor immunity. PNAS 117: 6047–6055.
Gottfried, E., Leoni A. Kunz-Schughart, S. Ebner, W. Mueller-Klieser, et al. 2006. Tumor-derived lactic acid modulates dendritic cell activation and antigen expression. Blood 107: 2013–2021.
Yabu, M., H. Shime, H. Hara, T. Saito, M. Matsumoto, T. Seya, T. Akazawa, and N. Inoue. 2011. IL-23-dependent and -independent enhancement pathways of IL-17A production by lactic acid. International Immunology 23: 29–41.
Peter, K., M. Rehli, K. Singer, K. Renner-Sattler, and M. Kreutz. 2015. Lactic acid delays the inflammatory response of human monocytes. Biochemical and Biophysical Research Communications 457: 412–418.
Dietl, K., K. Renner, K. Dettmer, B. Timischl, K. Eberhart, C. Dorn, et al. 2010. Lactic acid and acidification inhibit TNF secretion and glycolysis of human monocytes. The Journal of Immunology 184: 1200–1209.
Ranganathan, P., A. Shanmugam, D. Swafford, A. Suryawanshi, P. Bhattacharjee, et al. 2018. GPR81, a Cell-Surface Receptor for Lactate, Regulates Intestinal Homeostasis and Protects Mice from Experimental Colitis. The Journal of Immunology 200: 1781–1789.
Brown, F.F., J.P. Campbell, A.J. Wadley, J.P. Fisher, S. Aldred, and J.E. Turner. 2018. Acute aerobic exercise induces a preferential mobilisation of plasmacytoid dendritic cells into the peripheral blood in man. Physiology & Behavior 194: 191–198.
Oliveira, A.G., T.G. Araujo, B.M. Carvalho, D. Guadagnini, G.Z. Rocha, et al. 2013. Acute exercise induces a phenotypic switch in adipose tissue macrophage polarization in diet-induced obese rats. Obesity 21: 2545–2556.
Silveira, L.S., B. de Moura Mello Antunes, A.L.A. Minari, R.V.T. dos Santos, J.C.R. Neto, and F.S. Lira. 2016. Macrophage polarization: Implications on metabolic diseases and the role of exercise. Critical Reviews in Eukaryotic Gene Expression 26: 115–132.
Gupta, G.S., and G. Chaturvedi. 2000. Regulation of immune functions by sperm-specific LDH and its differences with somatic isozyme in primary and secondary lymphocyte cultures. American Journal of Reproductive Immunology 44: 160–169.
Gupta, G.S., G. Chaturvedi, and A. Joshi. 1996. Sex-dependent immunological suppression by LDH isozymes. Molecular and Cellular Biochemistry 158: 115–119.
Nenu, J., G.A. Gafencu, T. Popescu, and G. Kacso. 2017. Lactate - A new frontier in the immunology and therapy of prostate cancer. Journal of Cancer Research and Therapeutics 13: 406–411.
Actor, J.K. 2012. Mononuclear Cells and Macrophages. In: Elsevier’s Integrated Review Immunology and Microbiology (e book).
Maucourant, C., I. Filipovic, A. Ponzetta, S. Aleman, M. Cornillet, et al. 2020. Natural killer cell immunotypes related to COVID-19 disease severity. Science immunology 5: eabd6832.
Bi, J. 2022. NK cell dysfunction in patients with COVID-19. Cellular & molecular immunology 19: 127–129. https://doi.org/10.1038/s41423-021-00825-2.
Timmons, B.W., and T. Cieslak. 2008. Human natural killer cell subsets and acute exercise: A brief review. Exercise Immunology Review 14 (905): 8–23.
Pötzl, J., D. Roser, L. Bankel, N. Hömberg, A. Geishauser, et al. 2017. Reversal of tumor acidosis by systemic buffering reactivates NK cells to express IFN-γ and induces NK cell-dependent lymphoma control without other immunotherapies. International Journal of Cancer 140: 2125–2133.
Terrén, I., A. Orrantia, J. Vitallé, O. Zenarruzabeitia, and F. Borrego. 2019. NK Cell Metabolism and tumor microenvironment. Frontiers in Immunology 10: 2278.
Sanchez-Cerrillo, I., P. Landete, B. Aldave, S. Sanchez-Alonso, A. Sanchez-Azofra, et al. 2020. Differential Redistribution of Activated Monocyte and Dendritic Cell Subsets to the Lung Associates with Severity of COVID-19. medRxiv.
Wculek, S.K., S.C. Khouili, E. Priego, I. Heras-Murillo, and D. Sancho. 2019. Metabolic Control of dendritic cell functions: Digesting information. Frontiers in Immunology 2019: 10. https://doi.org/10.3389/fimmu.2019.00775.
AbdelMassih, A.F., R. Menshawey, R. Hozaien, A. Kamel, F. Mishriky, R.J. Husseiny, et al. 2021. The potential use of lactate blockers for the prevention of COVID-19 worst outcome, insights from exercise immunology. Medical Hypotheses 148: 110520.
Fujita, T. 2002. Evolution of the lectin-complement pathway and its role in innate immunity. Nature Reviews Immunology 2: 346–353.
Wallis, R., D.A. Mitchell, R. Schmid, W.J. Schwaeble, and A.H. Keeble. 2010. Paths reunited: Initiation of the classical and lectin pathways of complement activation. Immunobiology 215: 1–11.
Ali, Y.M., N.J. Lynch, K.S. Haleem, T. Fujita, Y. Endo, S. Hansen, et al. 2012. The lectin pathway of complement activation is a critical component of the innate immune response to pneumococcal infection. PLoS Pathogens 2012 (8): e1002793.
Nilsson, B., and Ekdahl K. Nilsson. 2012. The tick-over theory revisited: Is C3 a contact-activated protein? Immunobiology 217: 1106–1110.
Walport, M.J. 2001. Complement. First of two parts. New England Journal of Medicine 344: 1058–1066.
Wang, Y., E.S. Bjes, and A.F. Esser. 2000. Molecular aspects of complement-mediated bacterial killing. Periplasmic conversion of C9 from a protoxin to a toxin. Journal of Biological Chemistry 275: 4687–4692.
Miyazawa, K., and K. Inoue. 1990. Complement activation induced by human C-reactive protein in mildly acidic conditions. The Journal of Immunology 145: 650–654.
Sonntag, J., M. Emeis, E. Strauss, and M. Obladen. 1998. In vitro activation of complement and contact system by lactic acidosis. Mediators of Inflammation 7: 49–51.
Grinstein, S., C.J. Swallow, and O.D. Rotstein. 1991. Regulation of cytoplasmic pH in phagocytic cell function and dysfunction. Clinical Biochemistry 24: 241–247.
Kenawy, H.I., I. Boral, and A. Bevington. 2015. Complement-coagulation cross-talk: A potential mediator of the physiological activation of complement by low pH. Frontiers in Immunology 6 (6): 215.
Sheerin, N.S., P. Risley, K. Abe, Z. Tang, W. Wong, T. Lin, et al. 2008. Synthesis of complement protein C3 in the kidney is an important mediator of local tissue injury. The FASEB Journal 22: 1065–1072.
de Brito-Ashurst, I., M. Varagunam, M.J. Raftery, and M.M. Yaqoob. 2009. Bicarbonate supplementation slows progression of CKD and improves nutritional status. Journal of the American Society of Nephrology 20: 2075–2084.
Gaarkeuken, H., M.A. Siezenga, K. Zuidwijk, C. van Kooten, T.J. Rabelink, M.R. Daha, et al. 2008. Complement activation by tubular cells is mediated by properdin binding. American Journal of Physiology Renal Physiology 295: F1397–F1403.
Gupta, G.S. 1999. LDHC4: A Unique target of mammalian spermatozoa. Critical Reviews in Biochemistry and Molecular Biology 34: 361–368.
Seth, P., A. Grant, J. Tang, E. Vinogradov, X. Wang, R. Lenkinski, et al. 2011. On target inhibition of tumor fermentative glycolysis as visualized by hyperpolarized pyruvate. Neoplasia 13: 60–71.
Jialal, I., and L.J. Sokoll. 2015. Clinical Utility of Lactate Dehydrogenase: A Historical Perspective. American Journal of Clinical Pathology 143: 158–159.
Firth, J.D., B.L. Ebert, and P.J. Ratcliffe. 1995. Hypoxic regulation of lactate dehydrogenase A: Interaction between hypoxia-inducible factor 1 and cAMP response elements. Journal of Biological Chemistry 270: 21021–21027.
Urbańska, K., and A. Orzechowski. 2019. Unappreciated Role of LDHA and LDHB to Control Apoptosis and Autophagy in Tumor Cells. International Journal of Molecular Sciences 20: 2085.
Gupta, G.S. 2005. Proteomics of Spermatogenesis. New York: Springer.
Gupta, G.S., and N. Syal. 2000. Newly Exposed Immunochemically Cross-Reactive Epitopes in Sperm-Specific LDH after glucosylation and gossypo interaction. American Journal of Reproductive Immunology 44: 303–309.
Johns, G.C., and G.N. Somero. 2004. Evolutionary convergence in adaptation of proteins to temperature: A4-lactate dehydrogenases of Pacific Damselfishes (Chromis spp.). Molecular Biology and Evolution 21: 314–320.
Hogrefe, H.H., J.P. Griffitht, M.G. Rossmanns, and E. Goldberg. 1987. Characterization of the antigenic sites on the refined 3-A resolution structure of mouse testicular lactate dehydrogenase C4. Journal of Biological Chemistry 262: 13155–13162. https://doi.org/10.1016/S0021-9258(18)45181-2.
Young, A., C. Oldford, and R.J. Mailloux. 2020. Lactate dehydrogenase supports lactate oxidation in mitochondria isolated from different mouse tissues. Redox Biology 28: 101339.
Bhowal, B., S.L. Singla-Pareek, S.K. Sopory, and C. Kaur. 2020. From methylglyoxal to pyruvate: A genome-wide study for the identification of glyoxalases and D-lactate dehydrogenases in Sorghum bicolor. BMC Genomics 21: 145.
Feng, Y., Y. Xiong, T. Qiao, X. Li, L. Jia, and Y. Han. 2018. Lactate dehydrogenase A: A key player in carcinogenesis and potential target in cancer therapy. Cancer Medicine 7: 6124–6136.
Wu, Y., X. Cui, N. Wu, R. Song, W. Yang, W. Zhang, D. Fan, Z. Chen, and J. An. 2017. A unique case of human zika virus infection in association with severe liver injury and coagulation disorders. Science and Reports 7: 11393.
Brown, N.J., S.E. Higham, B. Perunovic, M. Arafa, S. Balasubramanian, et al. 2013. Lactate Dehydrogenase-B Is Silenced by Promoter Methylation in a High Frequency of Human Breast Cancers. PLoS ONE 8: e57697.
Stojanovic, K.S., and F. Lionnet. 2016. Lactate dehydrogenase in sickle cell disease. Clinica Chimica Acta 458: 99–102.
Lokesh, K., J. Kannabiran, and M.D. Rao. 2016. Salivary lactate dehydrogenase (LDH) – A novel technique in oral cancer detection and diagnosis. Journal of Clinical and Diagnostic Research 10: 34–37.
Coller, H.A. 2014. Is Cancer a Metabolic Disease? American Journal of Pathology 184: 4–17.
Ding, J., J.E. Karp, and A. Emadi. 2017. Elevated lactate dehydrogenase (LDH) can be a marker of immune suppression in cancer: Interplay between hematologic and solid neoplastic clones and their microenvironments. Cancer Biomarkers 19: 353–363.
Peng, M., N. Yin, S. Chhangawala, K. Xu, C.S. Leslie, and M.O. Li. 2016. Aerobic glycolysis promotes T helper 1 cell differentiation through an epigenetic mechanism. Science 354: 481–484.
Song, Y.J., A. Kim, G.T. Kim, H.Y. Yu, E.S. Lee, M.J. Park, et al. 2019. Inhibition of lactate dehydrogenase A suppresses inflammatory response in RAW 264.7 macrophages. Molecular Medicine Reports 19: 629–637.
Liu, J., X. Zheng, Q. Tong, W. Li, B. Wang, K. Sutter, et al. 2020. Overlapping and discrete aspects of the pathology and pathogenesis of the emerging human pathogenic coronaviruses SARS-CoV, MERS-CoV, and 2019-nCoV. Journal of Medical Virology 92: 491–494.
Liu, J., S. Li, J. Liu, B. Liang, X. Wang, H. Wang, W. Li, Q. Tong, J. Yi, L. Zhao, L. Xiong, C. Guo, J. Tian, et al. 2020. Longitudinal characteristics of lymphocyte responses and cytokine profiles in the peripheral blood of SARS-CoV-2 infected patients. eBioMedicine 55: 102763. https://doi.org/10.1016/j.ebiom.2020.
Chen, N., M. Zhou, X. Dong, J. Qu, F. Gong, et al. 2020. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in wuhan, China: A descriptive study. Lancet 395: 507–513.
Cepelak, I., S. Dodig, D. Romic, et al. 2006. Enzyme catalytic activities in chronic obstructive pulmonary disease. Archives of Medical Research 37: 624–629.
Hui, D.S. 2008. Review of clinical symptoms and spectrum in humans with influenza A/H5N1 infection. Respirology 13 (Suppl. 1): S10-13.
Morell, F., A. Roger, L. Reyes, M.J. Cruz, C. Murio, and X. Muñoz. 2008. Bird fancier’s lung: A series of 86 patients. Medicine (Baltimore) 87: 110–130.
Faruqi, S., R. Wilmot, C. Wright, and A.H. Morice. 2012. Serum LDH in chronic cough: A potential marker of airway inflammation. The Clinical Respiratory Journal 6: 81–87.
Inomata, M., R. Hayashi, K. Tokui, C. Taka, S. Okazawa, et al. 2016. Lactate dehydrogenase and body mass index are prognostic factors in patients with recurrent small cell lung cancer receiving amrubicin. Tumori 102: 606–609.
Mo, X., F. Wei, Y. Tong, L. Ding, Q. Zhu, et al. 2018. Lactic acid downregulates viral MicroRNA to promote epstein-barr virus-immortalized B lymphoblastic cell adhesion and growth. Journal of Virology 2018 (92): e00033-e118. https://doi.org/10.1128/JVI.00033-18.
Poggiali, E., D. Zaino, P. Immovilli, L. Rovero, G. Losi, A. Dacrema, et al. 2020. Lactate dehydrogenase and C-reactive protein as predictors of respiratory failure in CoVID-19 patients. Clinica Chimica Acta 509: 135–138.
Henry, B.M., G. Aggarwal, J. Wong, S. Benoit, J. Vikse, M. Plebani, and G. Lippi. 2020. Lactate dehydrogenase levels predict coronavirus disease 2019 (COVID-19) severity and mortality: A pooled analysis. American Journal of Emergency Medicine 38: 1722–1726.
Zhang, J., Y.-H. Yao, B.-G. Li, Q. Yang, P.-Y. Zhang, and H.-T. Wang. 2020. Prognostic value of pretreatment serum lactate dehydrogenase level in patients with solid tumors: a systematic review and meta-analysis. Frontiers in Oncology. https://doi.org/10.3389/fonc.2020.00677.
Gao, Y., T. Li, M. Han, M. Han, X. Li, D. Wu, et al. 2020. Diagnostic Utility of Clinical Laboratory Data Determinations for Patients with the Severe COVID-19. Journal of medical virology 92 (7): 791–796. https://doi.org/10.1002/jmv.25770.
Yan, H., X. Liang, J. Du, Z. He, Y. Wang, et al. 2021. Proteomic and Metabolomic Investigation of COVID-19 Patients with Elevated Serum Lactate Dehydrogenase. medRxiv. https://doi.org/10.1101/2021.01.10.21249333.
Vidal-Cevallos, P., F. Higuera-De-La-Tijera, N.C. Chávez-Tapia, F. Sanchez-Giron, E. Cerda-Reyes, et al. 2021. Lactate-dehydrogenase associated with mortality in hospitalized patients with COVID-19 in Mexico: A multi-centre retrospective cohort study. Annals of Hepatology 24: 100338. https://doi.org/10.1016/j.aohep.2021.100338.
Mehta, P., D.F. McAuley, M. Brown, E. Sanchez, R.S. Tattersall, and J.J. Manson. 2020. COVID-19: Consider cytokine storm syndromes and immunosuppression. Lancet 395 (10229): 1033–1034.
Tang, N., D. Li, X. Wang, and Z. Sun. 2020. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. Journal of Thrombosis and Haemostasis 18: 844–847. https://doi.org/10.1111/jth.14768.
Shekhanawar, M., H.T. Sarala, and R.A. Shaik. 2021. Role of D-Dimer and LDH in Assessment of Severity of Covid-19. Asian Journal of Medical Research 10: 1–8.
Zhou, F., T. Yu, R. Du, G. Fan, Y. Liu, et al. 2020. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 395 (10229): 1054–1062.
Velavana, T.P., and C.G. Meyer. 2020. Mild versus severe COVID-19: Laboratory markers. International Journal of Infectious Diseases 95: 304–307.
Huang, C., Y. Wang, X. Li, et al. 2020. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395: 497–506.
Wu, C., X. Chen, Y. Cai, et al. 2020. Risk Factors Associated With Acute Respiratory Distress Syndrome and Death in Patients With Coronavirus Disease 2019 Pneumonia in Wuhan, China. JAMA internal medicine 180: 934–943.
Li, L.-Q., T. Huang, Y.Q. Wang, Z.-P. Wang, Y. Liang, et al. 2020. 2019 novel coronavirus patients’ clinical characteristics, discharge rate and fatality rate of meta-analysis. Journal of Medical Virology 92: 577–583.
Chen, L., H.G. Liu, W. Liu, et al. 2020. Analysis of clinical features of 29 patients with 2019 novel coronavirus pneumonia. Zhonghua Jie He He Hu Xi Za Zhi 43: 203–208.
Li, Y.Y., W.N. Wang, Y. Lei, B. Zhang, J. Yang, et al. 2020. Comparison of the clinical characteristics between RNA positive and negative patients clinically diagnosed with 2019 novel coronavirus pneumonia. Zhonghua Jie He He Hu Xi Za Zhi 12 (43): 427–430.
Liu, M., P. He, H.G. Liu, X.J. Wang, F.J. Li, et al. 2020. Clinical characteristics of 30 medical workers infected with new coronavirus pneumonia. Zhonghua Jie He He Hu Xi Za Zhi 43: E016 Chinese.
Mo, P., Y. Xing, Y. Xiao, L. Deng, Q. Zhao, et al. 2020. Clinical characteristics of refractory COVID-19 pneumonia in Wuhan, China. Clinical Infectious Diseases 73 (11): e4208–e4213. https://doi.org/10.1093/cid/ciaa270.
Chan, J.F., S. Yuan, and K.H. Kok. 2020. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: A study of a family cluster. Lancet 395: 514–523.
Wang, Z., B. Yang, Q. Li, L. Wen, and R. Zhang. 2020. Clinical Features of 69 Cases with Coronavirus Disease 2019 in Wuhan, China. Clinical infectious diseases 71: 769–777.
Chen, C., C. Chen, J.T. Yan, N. Zhou, J.P. Zhao, and D.W. Wang. 2020. Analysis of myocardial injury in patients with COVID-19 and association between concomitant cardiovascular diseases and severity of COVID-19. Zhonghua Xin Xue Guan Bing Za Zhi 48: 567–657.
Urbanska, K., and A. Orzechowski. 2019. Unappreciated Role of LDHA and LDHB to Control Apoptosis and Autophagy in Tumor Cells. International journal of molecular sciences 20: 2085.
Ryberg, M., D. Nielsen, K. Osterlind, P.K. Andersen, T. Skovsgaard, and P. Dombernowsky. 2005. Predictors of central nervous system metastasis in patients with metastatic breast cancer. A competing risk analysis of 579 patients treated with epirubicin-based chemotherapy. Breast Cancer Research and Treatment 91: 217–225.
Gupta, G.P., and J. Massague. 2006. Cancer metastasis: Building a framework. Cell 127: 679–695.
Egeblad, M., E.S. Nakasone, and Z. Werb. 2010. Tumors as organs: Complex tissues that interface with the entire organism. Developmental Cell 6: 884–901.
Lyssiotis, C.A., and A.C. Kimmelman. 2017. Metabolic Interactions in the Tumor Microenvironment. Trends in Cell Biology 11: 863–875.
Pavlova, N.N., and C.B. Thompson. 2016. The Emerging Hallmarks of Cancer Metabolism. Cell Metabolism 1: 27–47.
Swierczynski, J., A. Hebanowska, and T. Sledzinski. 2014. Role of abnormal lipid metabolism in development, progression, diagnosis and therapy of pancreatic cancer. World Journal of Gastroenterology 20: 2279–3035.
Doherty, J.R., and J.L. Cleveland. 2013. Targeting lactate metabolism for cancer therapeutics. The Journal of Clinical Investigation 123: 3685–3692.
Gupta, G.S. 2012. LDHC4: A target with therapeutic potential for cancer and contraception. Molecular and cellular biochemistry 371: 115–127.
Wilpe, S.V., R. Koornstra, M.D. Brok, J.W. De Groot, C. Blank, J.D. Vries, et al. 2020. Lactate dehydrogenase: a marker of diminished antitumor immunity. OncoImmunology 9: 1. https://doi.org/10.1080/2162402X.2020.1731942.
Chen, J., M.X. Sun, Y.Q. Hua, et al. 2014. Prognostic significance of serum lactate dehydrogenase level in osteosarcoma: A meta-analysis. Journal of Cancer Research and Clinical Oncology 140: 1205–1210.
Robertson, J.G. 2007. Enzymes as a special class of therapeutic target: Clinical drugs and modes of action. Current Opinion in Structural Biology 17: 674–679. https://doi.org/10.1016/j.sbi.2007.08.008.
Seetharaman, R., M. Advani, S. Mali, and S. Pawar. 2020. Enzymes as targets of Drug Action: an Overview. International Journal of Medical Science and Current Research (IJMSCR) 3: 114–125. www.ijmscr.com.
Montesdeoca, N., M. López, X. Ariza, L. Herrero, and K. Makowski. 2020. Inhibitors of lipogenic enzymes as a potential therapy against cancer. The FASEB Journal 34: 11355–11381. https://doi.org/10.1096/fj.202000705R.
Sharma, C., N.K. Jha, M.F.N. Meeran, C.R. Patil, S.N., Goyal, and S. Ojha. 2021. Serratiopeptidase, A Serine Protease Anti-Inflammatory, Fibrinolytic, and Mucolytic Drug, Can Be a Useful Adjuvant for Management in COVID-19. Frontiers in Pharmacology 12: 1188. https://doi.org/10.3389/fphar.2021.603997.
Hoffmann, M., H. Hofmann-Winkler, J.C. Smith, N. Krüger, P. Arora, et al. 2021. Camostat mesylate inhibits SARS-CoV-2 activation by TMPRSS2-related proteases and its metabolite GBPA exerts antiviral activity. eBioMedicine 65: 103255. https://doi.org/10.1016/j.ebiom.2021.103255.
Saadat, Y.R., S.M.H. Khatibi, S.Z. Vahed, and M. Ardalan. 2021. Host Serine Proteases: A Potential Targeted Therapy for COVID-19 and Influenza. Frontiers in Molecular Biosciences. https://doi.org/10.3389/fmolb.2021.725528.
Granchi, C., I. Paterni, R. Rani, and F. Minutolo. 2013. Small-molecule inhibitors of human LDH5. Future Medicinal Chemistry 5: 1967–1991.
Friberg, A., H. Rehwinkel, D. Nguyen, V. Pütter, M. Quanz, J. Weiske, et al. 2020. Structural Evidence for Isoform-Selective Allosteric Inhibition of Lactate Dehydrogenase A. ACS Omega 22: 13034–13041.
Oshima, N., R. Ishida, S. Kishimoto, V.M. Darley-Usmar, M.C. Krishna, and L.M. Neckers. 2020. Dynamic Imaging of LDH Inhibition in Tumors Reveals Rapid In Vivo Metabolic Rewiring and Vulnerability to Combination Therapy. Cell Reports 30: 1798–1810.
Zhou, M., Y. Zhao, Y. Ding, H. Liu, Z. Liu, O. Fodstad, et al. 2010. Warburg effect in chemosensitivity: Targeting lactate dehydrogenase-A re-sensitizes taxol-resistant cancer cells to taxol. Molecular cancer 9: 33.
Zhai, X., Y. Yang, J. Wan, R. Zhu, and Y. Wu. 2013. Inhibition of LDHA by oxamate induces G2/M arrest, apoptosis and increases radiosensitivity in nasopharyngeal carcinoma cells. Oncology Reports 30: 2983–2991.
Dhup, S., R.K. Dadhich, P.E. Porporato, and P. Sonveaux. 2012. Multiple biological activities of lactic acid in cancer: Influences on tumor growth, angiogenesis and metastasis. Current Pharmaceutical Design 18: 1319–1330.
Armstrong, A.J., D.J. George, and S. Halabi. 2012. Serum lactate dehydrogenase predicts for overall survival benefit in patients with metastatic renal cell carcinoma treated with inhibition of mammalian target of rapamycin. Journal of Clinical Oncology 30: 3402–3407.
Miskimins, W.K., H.J. Ahn, J.Y. Kim, S. Ryu, Y.S. Jung, and J.Y. Choi. 2014. Synergistic anti-cancer effect of phenformin and oxamate. PLoS ONE 2014 (9): e8557665.
Gupta, G.S., S. Kapur, and R.G. Kinsky. 1988. Inhibition kinetics of lactate dehydrogenase by gossypol acetic acid. Biochemistry International 17: 25–34.
Kim, H.Y., B.I. Lee, J.H. Jeon, D.K. Kim, S.-G. Kang, J.-K. Shim, et al. 2019. Gossypol Suppresses Growth of Temozolomide-Resistant Glioblastoma Tumor Spheres. Biomolecules 9: 595. https://doi.org/10.3390/biom9100595.
Oliver, C.L., J.A. Bauer, K.G. Wolter, M.L. Ubell, A. Narayan, et al. 2004. In vitro effects of the BH3 mimetic, (-)-gossypol, on head and neck squamous cell carcinoma cells. Clinical Cancer Research 10: 7757–7763.
Kitada, S., M. Leone, S. Sareth, D. Zhai, J.C. Reed, and M. Pellecchia. 2003. Discovery, characterization, and structure-activity relationships studies of proapoptotic polyphenols targeting B-cell lymphocyte/leukemia-2 proteins. Journal of Medicinal Chemistry 46: 4259–4264.
Allison, S.J., J.R. Knight, C. Granchi, et al. 2014. Identification of LDH-A as a therapeutic target for cancer cell killing via (i) p53/NAD(H)-dependent and (ii) p53-independent pathways. Oncogenesis 2014 (3): e102.
Manerba, M., M. Vettraino, L. Fiume, et al. 2012. Galloflavin (CAS 568–80-9): A novel inhibitor of lactate dehydrogenase. ChemMedChem 7: 311–317.
Farabegoli, F., M. Vettraino, M. Manerba, L. Fiume, M. Roberti, and G. Di Stefano. 2012. Galloflavin, a new lactate dehydrogenase inhibitor, induces the death of human breast cancer cells with different glycolytic attitude by affecting distinct signaling pathways. European Journal of Pharmaceutical Sciences 47: 729–738.
Singh, R., V. Bhardwaj, and R. Purohit. 2020. Identification of a novel binding mechanism of Quinoline based molecules with lactate dehydrogenase of Plasmodium falciparum. Journal of Biomolecular Structure and Dynamics 3: 348–356.
Penna-Coutinho, J., W.A. Cortopassi, A.A. Oliveira, T.C.C. França, and A.U. Krettli. 2011. Antimalarial Activity of Potential Inhibitors of Plasmodium falciparum Lactate Dehydrogenase Enzyme Selected by Docking Studies. PLoS ONE 2011 (6): e21237.
Kim, E.-Y., T.-W. Chung, C.W. Han, S.Y. Park, K.H. Park, et al. 2019. A Novel Lactate Dehydrogenase Inhibitor, 1-(Phenylseleno)-4-(Trifluoromethyl) Benzene Suppresses Tumor Growth through Apoptotic Cell Death. Science and Reports 9: 3969.
Yeung, C., A.E. Gibson, S.H. Issaq, N. Oshima, J.T. Baumgart, L.D. Edessa, et al. 2019. Targeting Glycolysis through Inhibition of Lactate Dehydrogenase Impairs Tumor Growth in Preclinical Models of Ewing Sarcoma. Cancer Research 79: 5060–5073.
Nilov, D.K., E.A. Prokhorova, and V.K. Švedas. 2015. Search for Human Lactate Dehydrogenase A Inhibitors Using Structure-Based Modeling. Acta Nature 7: 57–63.
Billiard, J., J.B. Dennison, J. Briand, R.S. Annan, D. Chai, M. Colón, et al. 2013. Quinoline 3-sulfonamides inhibit lactate dehydrogenase A and reverse aerobic glycolysis in cancer cells. Cancer & metabolism 1: 19.
Wittrup, A., and J. Lieberman. 2015. Knocking down disease: A progress report on siRNA therapeutics. Nature Reviews Genetics 16: 543–552.
Wang, X., L. Xu, Q. Wu, M. Liu, F. Tang, Y. Cai, et al. 2017. Inhibition of LDHA Deliver Potential Anticancer Performance in Renal Cell Carcinoma. Urologia Internationalis 99: 237–244.
Sheng, S.L., J.J. Liu, Y.H. Dai, X.G. Sun, X.P. Xiong, and G. Huang. 2012. Knockdown of lactate dehydrogenase A suppresses tumor growth and metastasis of human hepatocellular carcinoma. FEBS Journal 279: 3898–3910.
Li, J., S. Zhu, J. Tong, H. Hao, J. Yang, Z. Liu, and Y. Wang. 2016. Suppression of lactate dehydrogenase A compromises tumor progression by downregulation of the Warburg effect in glioblastoma. NeuroReport 27: 110–115.
Zhao, D., S.-W. Zou, Y. Liu, X. Zhou, Y. Mo, et al. 2013. Lysine-5 acetylation negatively regulates lactate dehydrogenase A and is decreased in pancreatic cancer. Cancer Cell 23: 464–476.
Deiab, S., E. Mazzio, S. Messeha, N. Mack, and K.F. Soliman. 2013. High-throughput screening to identify plant derived human LDH-A inhibitors. European journal of medicinal plants 3: 603–615.
Gao, S., D.N. Tu, H. Li, J.X. Jiang, X. Cao, et al. 2016. Pharmacological or genetic inhibition of LDHA reverses tumor progression of pediatric osteosarcoma. Biomedicine & Pharmacotherapy 81: 388–393.
Fang, A., Q. Zhang, H. Fan, Y. Zhou, Y. Yao, Y. Zhang, and X. Huang. 2017. Discovery of human lactate dehydrogenase A (LDHA) inhibitors as anticancer agents to inhibit the proliferation of MG-63 osteosarcoma cells. Medchemcomm 8: 1720–1726. https://doi.org/10.1039/c7md00222j. Published online 2017 Jul 7.
Maldonado, V., C. Hernandez-Ramírez, E.A. Oliva-Pérez, C.O. Sánchez-Martínez, J.F. Pimentel-González, et al. 2021. Pentoxifylline decreases serum LDH levels and increases lymphocyte count in COVID-19 patients: Results from an external pilot study. International Immunopharmacology 90: 107209. https://doi.org/10.1016/j.intimp.2020.107209.
Acknowledgements
Facilities provided by Panjab University, Chandigarh, to GSG as Professor Emeritus are being acknowledged.
Author information
Authors and Affiliations
Contributions
Single authorship, not applicable.
Corresponding author
Ethics declarations
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not required.
Conflict of Interest
The author declares no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gupta, G.S. The Lactate and the Lactate Dehydrogenase in Inflammatory Diseases and Major Risk Factors in COVID-19 Patients. Inflammation 45, 2091–2123 (2022). https://doi.org/10.1007/s10753-022-01680-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-022-01680-7