ABSTRACT
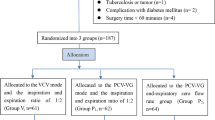
The aim of this present study is to compare the effect of pressure-controlled ventilation and volume-controlled ventilation on pulmonary mechanics and inflammatory markers in prone position. The study included 41 patients undergoing to vertebrae surgery. The patients were randomized into two groups: Group 1 received volume-controlled ventilation, while group 2 received pressure-controlled ventilation. The demographic data, pulmonary mechanics, the inflammatory marker levels just after the induction of anesthetics, at the 6th and 12th hours, and gas analysis from arterial blood samples taken at the beginning and the 30th minute were recorded. The inflammatory marker levels increased in both groups, without any significant difference among groups. Peak inspiratory pressure level was higher in the volume-controlled ventilation group. This study revealed that there is no difference regarding inflammatory marker levels between volume- and pressure-controlled ventilation.

Similar content being viewed by others
REFERENCES
Kim, B.S. 2009. Anesthesia and pain management, 2nd ed, 929–973. Seoul: Elsevier Korea.
Warner, M.A. 2006. Patient positioning. In Clinical anesthesia, 5th ed, ed. P.G. Barash, B.F. Cullen, and R.K. Stoelting, 657–661. Philadelphia: Lippincott-Raven Publishers.
Manna, E.M., O.A. Ibraheim, A.H. Samarkandi, W.M. Alotaibi, and S.M. Elwatidy. 2005. The effect of prone position on respiratory mechanics during spinal surgery. Middle East Journal of Anesthesiology 18: 623–630.
Senturk, M. 2006. New concepts of the management of one-lung ventilation. Current Opinion in Anaesthesiology 19(1): 1–4.
Benumorf, J.L. 2000. Anesthesia for thoracic surgery. In Anesthesia, ed. M. Anesthesia, 1665–2000. Philadephia.
Longnecker, D.E. 1984. Stres free to be or not to be? In Anaesthesiology, ed. D. E. Longnecker, 643–644.
Rozet, I., and M.S. Vavilala. 2007. Risks and benefits of patient positioning during neurosurgical care. Anesthesiology Clinics 25(3):631–653.
Krayer, S., et al. 1989. Position and motion of the human diaphragm during anesthesia-paralysis. Anesthesiology 70(6): 891–898.
Pelosi, P., et al. 1995. The prone positioning during general anesthesia minimally affects respiratory mechanics while improving functional residual capacity and increasing oxygen tension. Anesthesia and Analgesia 80(5): 955–960.
Jiang, J., B. Li, N. Kang, A. Wu, and Y. Yue. 2015. Pressure-controlled versus volume-controlled ventilation for surgical patients: a systematic review and meta-analysis. Journal of Cardiothoracic and Vascular Anesthesia.
Palmon, S.C., et al. 1998. The effect of the prone position on pulmonary mechanics is frame-dependent. Anesthesia and Analgesia 87(5): 1175–1180.
Soro, M., et al. 2007. Effects of prone position on alveolar dead space and gas exchange during general anaesthesia in surgery of long duration. European Journal of Anaesthesiology 24(5): 431–437.
Nam, Y., A.M. Yoon, Y.H. Kim, and S.H. Yoon. 2010. The effect on respiratory mechanics when using a Jackson surgical table in the prone position during spinal surgery. Korean Journal of Anesthesiology 59(5): 323–328.
Wahba, R.W., M.J. Tessler, and K.J. Kardash. 1998. Carbon dioxide tensions during anesthesia in the prone position. Anesthesia and Analgesia 86(3): 668–669.
Manikandan, S. 2002. Effect of surgical position on pulmonary gas exchange in neurosurgical patients. In Effect of surgical position on pulmonary gas exchange in neurosurgical patients, ed. S. Manikandan, Vol. 46. India: Indian J Anaesth.
Franke, A., et al. 2002. Proinflammatory and antiinflammatory cytokines after cardiac operation: different cellular sources at different times. Annals of Thoracic Surgery 74(2): 363–370. discussion 370–1.
Fishman, A.P. 1992. Update, pulmonary diseases and disorders. In Update, pulmonary diseases and disorders, ed. A.P. Fishman.
Finn, A., et al. 1993. Interleukin-8 release and neutrophil degranulation after pediatric cardiopulmonary bypass. Journal of Thoracic and Cardiovascular Surgery 105(2): 234–241.
Feldmann, M., and R.N. Maini. 2001. Anti-TNF alpha therapy of rheumatoid arthritis: what have we learned? Annual Review of Immunology 19: 163–196.
Memtsoudis, S.G., A.M. Bombardieri, Y. Ma, and F.P. Girardi. 2012. The effect of low versus high tidal volume ventilation on inflammatory markers in healthy individuals undergoing posterior spine fusion in the prone position: a randomized controlled trial. Journal of Clinical Anesthesia 24(4): 263–269.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Approval was obtained from the local Ethics Board of Afyon Kocatepe University Facullty of Medicine.
Rights and permissions
About this article
Cite this article
Şenay, H., Sıvacı, R., Kokulu, S. et al. The Effect of Pressure-Controlled Ventilation and Volume-Controlled Ventilation in Prone Position on Pulmonary Mechanics and Inflammatory Markers. Inflammation 39, 1469–1474 (2016). https://doi.org/10.1007/s10753-016-0379-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-016-0379-2