Abstract
This review provides a comprehensive overview of heart failure with mildly reduced and preserved ejection fraction (HFmrEF/HFpEF), including its definition, diagnosis, and epidemiology; clinical, humanistic, and economic burdens; current pharmacologic landscape in key pharmaceutical markets; and unmet needs to identify key knowledge gaps. We conducted a targeted literature review in electronic databases and prioritized articles with valuable insights into HFmrEF/HFpEF. Overall, 27 randomized controlled trials (RCTs), 66 real-world evidence studies, 18 clinical practice guidelines, and 25 additional publications were included. Although recent heart failure (HF) guidelines set left ventricular ejection fraction thresholds to differentiate categories, characterization and diagnosis criteria vary because of the incomplete disease understanding. Recent epidemiological data are limited and diverse. Approximately 50% of symptomatic HF patients have HFpEF, more common than HFmrEF. Prevalence varies with country because of differing definitions and study characteristics, making prevalence interpretation challenging. HFmrEF/HFpEF has considerable mortality risk, and the mortality rate varies with study and patient characteristics and treatments. HFmrEF/HFpEF is associated with considerable morbidity, poor patient outcomes, and common comorbidities. Patients require frequent hospitalizations; therefore, early intervention is crucial to prevent disease burden. Recent RCTs show promising results like risk reduction of composite cardiovascular death or HF hospitalization. Costs data are scarce, but the economic burden is increasing. Despite new drugs, unmet medical needs requiring new treatments remain. Thus, HFmrEF/HFpEF is a growing global healthcare concern. With improving yet incomplete understanding of this disease and its promising treatments, further research is required for better patient outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background and objectives
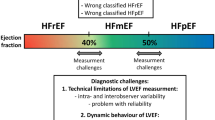
Chronic heart failure (HF) is a multisystemic disorder and a leading cause of cardiovascular (CV) morbidity and mortality globally [1,2,3]. Its severity and impact on patients’ physical activity are typically categorized using the widely employed New York Heart Association (NYHA) functional classification system, which categorizes the severity of HF symptoms into classes I to IV. Class I refers to asymptomatic patients; class II, class III, and class IV correspond to mildly, moderately, and severely symptomatic patients, respectively [1, 2]. Furthermore, HF is classified into 3 groups based on patients’ left ventricular ejection fraction (LVEF): heart failure with reduced ejection fraction (HFrEF) (LVEF ≤ 40%); mildly reduced ejection fraction (HFmrEF) (LVEF 41%-49%); and preserved ejection fraction (HFpEF) (LVEF ≥ 50%) [1,2,3]. The prevalence of HF is increasing worldwide, largely because of aging populations and lifestyle factors contributing to a higher prevalence of risk factors [4, 5]. Data suggest that HFmrEF and HFpEF are projected to become the dominant HF subtypes in the future, given their substantial and growing prevalence among patients with HF worldwide, leading to substantial patient burden and unmet needs because of limited treatment options [4, 5]. Currently, only a few drugs have been specifically approved to treat HFmrEF/HFpEF. In recent years, initial approvals have been granted for sodium-glucose cotransporter-2 inhibitors (SGLT-2is)—including empagliflozin [6, 7] and dapagliflozin [8, 9]—and angiotensin receptor/neprilysin inhibitor (ARNI) sacubitril/valsartan [10]. Prior to these recent approvals, there was a lack of conclusive studies showing improvements in the course or prognosis of HFmrEF/HFpEF in the long term [1, 2, 5]. Previous reviews have presented data on the burden of illness and epidemiology of HFpEF and HFmrEF. However, some of these publications have relatively dated time frames or focus on countries out of key pharmaceutical markets like United States, Western Europe and Japan [11,12,13]. Considering the recent changes in the treatment landscape, the objective of this review is to provide the most up-to-date data on the definition and diagnosis, epidemiology, burden of illness, and current pharmacologic landscape in the United States, Europe (with a focus on the United Kingdom, France, Germany, and Sweden), and Japan in relation to HFmrEF/HFpEF. Finally, this review aims to assess the remaining unmet needs and identify key knowledge gaps.
Methods
Study design and search process
To assess the existing research on HFpEF and HFmrEF, a targeted literature review (TLR) was conducted. The search process adhered to the methods recommended by the Cochrane Collaboration Handbook [14] and the Centre for Reviews and Dissemination [15]. The TLR was performed in the Ovid MEDLINE® In-Process & Other Non-Indexed Citations and Ovid MEDLINE® databases, with the search for articles published from January 2012 through September 2022 (except for RCTs, for which no time restriction was applied) focusing on the most recent data. The gray literature search was conducted in January 2023 and included targeted, iterative manual searches of 29 regulatory and/or research organization websites, which are listed in Supplementary Table 1.
Eligibility criteria
Abstracts and full texts were screened by a reviewer who selected relevant articles based on the eligibility criteria (Supplementary Table 2). The eligibility criteria included studies focusing on adult patients diagnosed with HF (NYHA II-IV) and LVEF ≥ 40% (symptomatic HFmrEF/HFpEF). The analysis considered various outcomes, including epidemiologic data, clinical and humanistic burden, treatment overviews, economic burden, and economic evaluations. To ensure the comprehensive coverage of evidence, the study design criteria included real-world evidence (RWE), RCTs, treatment guidelines, systematic literature reviews (SLRs), cost-effectiveness analyses (CEAs), and budget impact analyses (BIAs). There were no restrictions regarding the study design for economic burden studies. Studies eligible for inclusion had to be published in English, except for treatment guidelines, which were considered irrespective of language.
A process of study prioritization was then undertaken to identify those articles most likely to provide valuable insights into the research topics. During the prioritization process, studies conducted in populations of patients with acute HF were excluded. Furthermore, those that used medical devices, diagnostic tests, dietary supplements, and genetic testing with regard to behavioral interventions were excluded. Pilot studies, phase 1 and phase 2 trials, pooled analyses, reviews, and SLRs were also excluded. Additionally, studies were excluded if their sample size was < 50 patients for RCTs or < 100 patients for RWE studies. For RCTs, only studies evaluating the most commonly used and recommended medications according to the guidelines [SGLT-2is, sacubitril/valsartan, mineralocorticoid antagonists (MRAs), angiotensin-converting enzyme inhibitors (ACE-Is), and angiotensin receptor blockers (ARBs)] were included. Moreover, only the latest guidelines were considered. For RWE studies reporting epidemiology, comorbidities, effectiveness, safety, treatment patterns, or economic burden, only studies with data collection end dates in ≥ 2016 were included.
Data extraction
The epidemiologic outcomes of interest included the incidence, prevalence, mortality, and co-morbidities related to HFpEF and/or HFmrEF. Management outcomes of interest included the treatment pattern/practice, percentage of patients receiving each treatment type, adherence/compliance, discontinuation rate and adverse events, predictors, and risk factors for HF. To assess clinical burden, the following outcomes were collected: CV death; HF events; improvement in NYHA class; non-fatal CV events; composite renal events [defined as a sustained decrease in estimated glomerular filtration rate (eGFR) ≥ 50%, a sustained decrease in eGFR ≥ 57%, a sustained eGFR decline to < 15 ml/min/1.73m2, and the initiation of dialysis or renal transplantation]; changes in UACR from baseline; new onset of atrial fibrillation; and hospitalizations (all-cause and CV). The humanistic burden outcome of interest was health-related quality of life (HRQoL). Economic burden outcomes included direct costs, indirect costs, and resource use.
Quality assessment and risk of bias
The quality of the included RCTs was assessed using the Cochrane Risk of Bias Tool checklist [14]. For the included cohort studies, their methodologic quality was assessed using the Newcastle–Ottawa Scale (NOS) or an adapted version of the NOS in the case of cross-sectional studies [16].
Results
Literature search results
The electronic searches yielded 6134 records after the de-duplication process. A total of 580 records met the relevant criteria. An additional 9 records were obtained from cross-reference checking or from other sources, such as clinicaltrials.gov. Following the prioritization process, 105 records were included in the qualitative synthesis. Moreover, 31 records were sourced from manual searches. The study selection process is depicted in Fig. 1. Additionally, the distribution of included studies by study design and type of document is presented in Fig. 2. The characteristics of the RCTs and RWE included in the TLR are presented in Tables 1 and 2. The review found 18 guidelines for HF (including HFmrEF/HFpEF) from 6 countries (the United States, Japan, France, Germany, Sweden, and the United Kingdom) published between 2014 and 2022. Supplementary Table 3 provides an overview of these guidelines and their recommendations for HFmrEF/HFpEF care.
Definition and diagnosis
The general definition of chronic HF was specified in 12 out of 18 clinical guidelines [1,2,3, 17,18,19,20,21,22,23,24,25]. HFpEF was defined in 15 [1,2,3, 17,18,19,20, 23,24,25,26,27,28,29,30] of 18 [1,2,3, 17,18,19,20,21,22,23,24,25,26,27,28,29,30,31] guidelines; HFmrEF was defined in 10 of 18 guidelines [1,2,3, 17, 19, 20, 23, 24, 27, 28]. The HFmrEF/HFpEF population is often grouped together, but they are well defined in the latest heart failure clinical guidelines for the United States, Europe, and Japan based on their LVEF values [1,2,3]. The guidelines set an LVEF cut-off of ≥ 50% for HFpEF and between 40 to 41% and 49% for HFmrEF. Additionally, the guidelines describe more subgroups in the HFmrEF/HFpEF population, including patients transitioning between LVEF categories, which may present different outcomes, such as HF with improved EF (patients whose LVEF improved from < 40% to > 40%) [1,2,3]. However, there were variations in the definition of HFpEF in the included RCT and RWE studies compared with the guidelines, represented by differences in LVEF thresholds (> 40%, ≥ 45%, or ≥ 50%). HFmrEF, usually considered part of HFpEF, was not explicitly defined in these studies, with most of them using an LVEF cut-off of > 40% or ≥ 45%. RCTs usually include subgroup analyses in the population of patients with LVEF < 50% (corresponding to the HFmrEF population, per the guidelines) [13, 32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55]. HFpEF and HFmrEF are 2 groups of HF characterized by a complex pathophysiology and overlapping symptoms, making their diagnoses challenging. Multiple risk factors and causes contribute to these conditions, and their phenotypic manifestations can vary [2, 26]. Despite ongoing HF research, information from the literature on the specific predictors and risk factors for the HFmrEF/HFpEF population is scarce. Only 2 included studies reported limited information on the predictors and risk factors for HFpEF and advanced HF [56, 57]. One study indicated a higher likelihood of HFpEF in participants with diabetes and microvascular complications [56], aligning with calls for further research on the disease’s pathophysiology and natural history made in the literature [58]. Diagnosing HFmrEF/HFpEF is challenging because of its nonspecific signs and symptoms, which can overlap with other conditions [2]. Therefore, cardiac imaging and the measurement of natriuretic peptides (NPs) play a crucial role in diagnosis. Guidelines propose specific diagnostic criteria, with an NT proBNP value threshold > 125 pg/ml commonly used for HFpEF diagnosis. However, challenges remain and different guidelines recommend various diagnostic algorithms, like H2FPEF (heavy, 2 or more hypertensive drugs, atrial fibrillation, pulmonary hypertension, elder age > 60, elevated filling pressures) or HFA-PEFF (Heart Failure Association-pre-test assessment, echocardiography and natriuretic peptide score, functional testing, final aetiology) scores [1,2,3, 17, 26], leading to different patient classifications [1, 2]. Limited access to specialized tests may hinder the practicality of these scores, contributing to ongoing diagnostic uncertainty in HFpEF [1]. To address this, a simplified pragmatic approach was recommended by the European Society of Cardiology (ESC) 2021, German Cardiac Society 2021, and US 2022 guidelines, focusing on widely available variables for diagnosing HFpEF (Table 3) [1, 2, 17]. The generalizability of the scores used for HFpEF diagnosis has been tested in various trials and cohorts, resulting in a varying diagnostic performance [1]. In a few guidelines, the HFmrEF diagnostic criteria align with HFpEF [1, 2, 17, 23, 28]. The diagnosis of HFmrEF requires the presence of symptoms and/or signs of cHF, and a mildly reduced EF (LVEF measurement). The presence of elevated NPs and other evidence of structural heart disease make the diagnosis more likely but are not mandatory for diagnosis if there is certainty regarding the measurement of LVEF [1]. The main criteria used in RCTs is similar to those mentioned in clinical guidelines, relying on symptoms, signs, hospitalization, structural heart disease evidence, echocardiographic data (LVEF criteria varies among studies), and NP levels for HFmrEF/HFpEF diagnosis.
Prevalence
The prevalence of HFmrEF and/or HFpEF among HF patients was reported in 29 studies. The overall prevalence of HF has reportedly increased, with approximately 50% of symptomatic HF patients having HFmrEF/HFpEF [47, 59,60,61,62,63]. However, estimates of HFpEF prevalence varied among countries (Fig. 3) [47, 59,60,61,62,63,64]. A US-based single-center study involving 874 patients revealed the highest prevalence of HFpEF among patients with HF, reaching 61% [62]. In the same study, 15% of HF patients were diagnosed with HFmrEF. A similar trend was observed in the US-based National Cardiovascular Data Registry Practice Innovation and Clinical Excellence (NCDR PINNACLE) registry [65], where 56.5% of patients with HF had HFpEF and 7.5% had HFmrEF [65]. The regional distribution of HF phenotypes across the United States was heterogenous and may have reflected differences in the prevalence of main risk factors (including obesity, hypertension, or diabetes), with HFpEF and HFmrEF being most prevalent in the South [65]. Among the European countries of interest, the highest prevalence of HFpEF and HFmrEF in patients with HF was reported in Germany at 45% and 44%, respectively, as reported by Wenzel et al. [47]. Additionally, Gobel et al. reported a prevalence of 37% for HFpEF in the same country [66]. The lowest prevalence was reported in France (23% and 33%, respectively) and in Sweden (24% for both HFpEF and HFmrEF) [60, 61]. In Japan, HFpEF prevalence was high across patients hospitalized because of HF (43%) [63, 67]. In Japan additional prevalence data were reported in specific sub-populations showing 44.3% in patients on maintenance hemodialysis (44.3%) [63, 67]; 18.6% and 25% across HF adults with comorbid diabetes and HF [56]. Across studies with decompensated HF patients, HFpEF prevalence ranged between 43% [68] and 55.1% [69]. In Japan, similarly, as in other countries, the prevalence of HFmrEF was lower and ranged between 15 and 21% for HF patients overall [62, 70].
Incidence
Recent data on the incidence of HFpEF and/or HFmrEF are scarce, with only 1 identified study conducted in the United States, using data limited to just 1 US district (a cohort of adult residents from Olmsted County, Minnesota). The cumulative incidence at 6 years was 11.7% for advanced HFpEF (defined as refractory HF symptoms despite attempts to optimize guideline-directed medical therapies) and 11.4% for HFmrEF [57].
Mortality
Results for mortality among patients with HFpEF and/or HFmrEF were reported in 22 studies. The US-based studies showed varied mortality results due to differences in study design, patient characteristics, and outcome definitions. For HFpEF patients with similar baseline risks, the 1-year all-cause mortality ranged from 18.5% to 26.4% [71, 72]; patients with a higher baseline risk (admitted to intensive care) had a higher 1-year mortality risk (35.1% for HFpEF and 24.6% for HFmrEF) [73]. Patients with HFmrEF had a lower unadjusted risk of in-hospital death (8% vs 12%) than patients with HFpEF. However, after adjustment, the short-term mortality differences were not significant [73]. In Sweden, HFmrEF was associated with lower all-cause mortality compared with HFpEF (10.3 vs 13.2 events per 100 patient-years) [61]. However, in a study in France, there was no significant difference in mortality among HFmrEF and HFpEF patients hospitalized for congestive HF. In this study over a follow-up period of 2.17 ± 1.38 years, 41.3% of 383 deaths (158 deaths) were in patients with HFpEF, and 39.3% (108 deaths) were in patients with HFmrEF [74]. In a retrospective UK study covering 2 12-month periods, patients admitted with HF showed lower overall mortality in the 2015/2016 cohort compared to 2012/2013, especially in HFpEF cases (13.3% vs 16.3%, P = 0.435). There was no significant difference in in-hospital mortality between the 2 cohorts for HFpEF (P = 0.472). Notably, for HFpEF, 30-day post-discharge mortality decreased from 8.9% (2012/2013) to 3.1% (2015/2016) (P = 0.032) [75]. Improved mortality was prominent among cardiology ward patients, possibly due to optimised fluid status and extended inpatient stays [75]. The Swedish registry data (SwedeHF) [44] revealed that HFpEF patients on beta-blockers had lower mortality rates at 1, 3, and 5 years (16%, 37%, and 53%, respectively) with an incidence rate of 157 per 1000 patient-years (95% CI: 153–162) compared with non-beta-blocker users. The non-beta-blocker users had mortality rates of 22%, 47%, and 62% at 1, 3, and 5 years, respectively, with an incidence rate of 209 per 1000 patient-years (95% CI: 197–221) [44]. A Swedish study revealed that hypertension, atrial fibrillation, and ischemic heart disease were the main factors for mortality in HFpEF. Being of a younger age and having a low comorbidity burden were associated with lower mortality rates [36].
In Japan, for HFpEF, the in-hospital mortality rate was 8%; for HFmrEF, it was 6% [63]. After discharge, the mortality rate ranged from 16% to 24.7% [63, 76].
Comorbidities
The most common comorbidities among patients with HFmrEF/HFpEF are hypertension, atrial fibrillation, coronary artery disease (CAD), diabetes, obesity, chronic kidney disease (CKD), and chronic obstructive pulmonary disease (COPD). In a large US registry (PINNACLE; 2008–2016) with 697,542 patients with HF, including 324,387 patients with HFpEF and 56,527 with HFmrEF [65], the most prevalent comorbidities among HFpEF patients were hypertension (79.1%), CAD (55.5%), atrial fibrillation (AF) or atrial flutter (AFL) (34.4%), and diabetes (25.7%). Patients with HFmrEF had a higher prevalence of CAD, peripheral artery disease, AF or AFL, CKD, diabetes, and prior myocardial infarction compared with those who had HFrEF or HFpEF (P < 0.001) [65]. In a 2013 to 2016 US-based outpatient registry of patients with diabetes and prediabetes who were prescribed ≥ 1 glucose-lowering medication and diagnosed with HF (55.5% with LVEF ≥ 50%), CV comorbidities were common: 87.3% had hypertension, 59.0% had CAD, and 37% had AF/AFL [77]. In a large nationwide Swedish registry (2000–2018), collecting data mainly from secondary care inpatients, outpatient wards and clinics, and primary care settings for clinician-judged HF, the most frequently reported comorbidities among patients with HF at follow-up in specialty care versus primary care were as follows: hypertension (62.2% vs 76.6%), AF (54.8% vs 63.3%), ischemic heart disease (54.3% vs 56.7%), kidney disease (44.3% vs 61.7%), and anemia (33% vs 40.8%) [61]. The prevalence of major comorbidities was slightly higher in patients with HFpEF compared to HFmrEF, in both specialty care and primary care [61]. In the largest Japanese prospective observational study (2010–2018), the most commonly reported comorbidities in patients with HFpEF and HFmrEF were hypertension and dyslipidemia, followed by CKD, anemia, and sleep-disordered breathing [41].
Clinical burden
Efficacy in randomized controlled trials
The efficacy of interventions in patients with HFmrEF/HFpEF has been largely studied in RCTs. The most commonly reported outcome in RCTs was a composite of CV death or HF hospitalization, but definitions varied, affecting interpretation. The main differences were related to the inclusion of first/recurrent hospitalizations and HF with or without urgent visits. Additionally, some studies categorized deaths from undetermined causes as CV deaths (eg, EMPEROR-Preserved) [78], although others excluded them (eg, DELIVER) [79]. Overall, interventions reduced the HF hospitalization risk, but the effect on mortality was not significant (Table 4). In large, long-term, HF-specific RCTs, SGLT-2is—mainly dapagliflozin (DELIVER) [79] and empagliflozin (EMPEROR-Preserved) [78]—significantly reduced the risk of a composite of CV death or hospitalization for HF compared with controls [79, 80]. This effect was mainly driven by the risk reduction for HF hospitalization. Overall, SGLT-2is [dapagliflozin [79] and empagliflozin [81, 82] and spironolactone therapy significantly reduced HF hospitalization compared with controls; sacubitril/valsartan had no effect on HF events [35]. Candesartan moderately reduced HF hospitalizations [unadjusted hazard ratio (HR): 0.85 (95% CI: 0.72–1.01), P = 0.072; adjusted HR: 0.84 (95% CI: 0.70–1.000), P = 0.047] in the HFpEF population, with fewer HF hospitalizations compared with the placebo group (230 vs 279, P = 0.017) [83]. In the perindopril in elderly people with chronic heart failure (PEP-CHF) study, perindopril lowered the HF hospitalization risk in the first year [HR: 0.63 (95% CI: 0.41–0.97), P = 0.033], but it did not have this effect throughout the follow-up period (mean: 26.2 months) [84]. No treatment significantly reduced the CV death risk, regardless of the definition used. Most RCTs analyzed subgroups based on demographics, medical history, or prior treatments for the primary outcome only, which differed among studies. The overall effect was generally consistent across subgroups. In the EMPEROR-Preserved study, conducted in patients with EF > 40%, the empagliflozin group had a significantly lower risk of CV death or worsening HF events (hospitalization for HF or an urgent HF visit requiring intravenous therapy) compared with the placebo group. The benefit increased when only patients with LVEF < 60% were considered [82]. In PARAGON-HF, the sacubitril/valsartan group showed a significantly lower risk of CV death or HF hospitalization compared with patients administered valsartan alone, with greater benefit afforded to patients with an LVEF of 45% to 57% and women [85]. In TOPCAT, spironolactone's effect varied based on the randomization stratum and prior HF hospitalization. This effect was better among patients not hospitalized for HF in the year prior to study enrollment. Post hoc analysis showed significant regional differences in event rates for the primary outcome (CV death, aborted cardiac arrest, or hospitalization for HF), with a significant risk reduction in the Americas (in the United States, Canada, Brazil, and Argentina) but not in Russia or Georgia [86].
Real-world effectiveness
There is a limited availability of RWE regarding patients with HFpEF and/or HFmrEF. The existing data mainly came from subgroup analysis, so caution is advised in their interpretation. There was significant heterogeneity among the included studies, particularly in the definitions of HFmrEF/HFpEF, baseline characteristics, comorbidity burden, and outcome definition and follow-up. Most studies focused on the clinical burden in patients treated with standard HF treatments, without focusing on any specific drugs.
The real-world data indicated high morbidity with increased rates of hospitalization. According to Afzal et al., in the United States, hospitalizations for HF increased from 45,148 in 2004 to 297,125 in 2016. The number of diastolic HF cases (HFpEF) increased between 2007 and 2008 but decreased significantly in 2017 because of changes in HF coding [87]. Additionally, Clark et al., found a significant increase in hospitalizations due to HFpEF from 189,260 in 2008 to 495,095 in 2018 [88]. Over time, hospitalizations due to HFpEF involved younger patients (from a mean age of 78 years in 2008 to 77 years in 2018) and were less common among female patients (from 65.3% to 60.3% in 2018; P < 0.001 for all). The prevalence of comorbidities also rose among HFpEF hospitalizations, including diabetes (43.0% in 2008 to 51.6% in 2018), obesity (14.2% to 32.8%), and obstructive sleep apnea (9.2% to 19.5%) (P < 0.001 for all). Reinhardt et al. studied hospitalization trends in HF and AF patients using the National Inpatient Sample (NIS) between 2008 and 2017. Among HFpEF patients, there were 3,117,059 admissions, with the percentage of HFpEF hospitalizations with comorbid AF rising from 38.0% in 2008 to 49.1% in 2017 [89]. Patients with HFpEF and AF with comorbid hypertension had the highest hospitalization rates. Results from a US cohort study (2010–2019) showed increasing hospitalizations for worsening HF from 0.6 to 1.0 per 100 hospitalizations per year for HFmrEF. For HFpEF, hospitalizations increased from 2.6 to 3.9 per 100 hospitalizations per year [90]. In patients from the SwedeHF registry who had HFpEF, beta-blockers did not impact HF hospitalizations at 5 years [42% with beta-blockers vs 43% without; unadjusted HR: 0.97 (95% CI: 0.90–1.05)]. In the matched cohort, no significant association was found between beta-blockers and HF admissions [HR: 0.95 (95% CI: 0.87–1.05)] [44]. However, beta-blockers were associated with a lower risk of all-cause hospital admissions at 1 year and 5 years (56% and 88% with beta-blockers; 60% and 91% without) [44].
Real-world data for CV deaths in patients with HFpEF and/or HFmrEF have not been widely reported, making comparisons with RCTs difficult because of study design and baseline differences. A cluster analysis identified clinically distinct HFpEF clusters, with the highest CV death incidence and hazard ratio in the cluster including older patients with multiple CV comorbidities and hypertension [36]. A US study comparing classification approaches for elderly patients with HF found similar 1-year CV death rates in HFpEF cases, with slightly different contributions to overall mortality based on the approach used [91]. A Swedish study found that beta-blockers significantly reduced the risk of CV mortality [HR: 0.8 (95% CI: 0.73–0.87), P < 0.001] in patients with HFpEF. At 5 years, CV death was reported in 40% (95% CI: 37–43) of non-beta-blocker users and 35% (95% CI: 33–36) of beta-blocker users (48). In Japan, a study showed lower CV deaths in tolvaptan responders with HFpEF (5.9%) compared with non-responders (18%); the difference was not significant compared with patients with HFrEF (P = 0.288 for responders; P = 0.245 for non-responders) [76].
Safety in randomized controlled trials
Overall, 21 studies reported safety outcomes in populations of patients with HFpEF and/or HFmrEF. The investigated treatments for HFpEF (with or without HFmrEF), including SGLT-2is, MRAs (spironolactone), ARNIs (sacubitril/valsartan), ACE-Is, and ARBs, exhibited a generally good safety profile. Specific side effects included genital and urinary tract infections, hypotension, and fractures for SGLT-2is or hyperkalemia, worsening of renal function, and anemia for spironolactone. The percentage of patients discontinuing treatment was comparable between study arms in all studies except one, in which a numerically higher percentage of patients discontinued ramipril treatment compared with diuretics (13.3% vs 6%) [80]. The overall rates of adverse events (AEs) were similar among the treated patients and the comparator groups, except for 1 trial of sacubitril/valsartan, which reported a significantly higher percentage of total AEs in the sacubitril/valsartan group compared with the background medication-based comparator group [32]. The most frequent AEs during sacubitril/valsartan treatment were hypotension and hyperkalemia.
Real-world safety
Real-world safety data were limited (reported in 3 studies) but indicated higher rates of hyperkalemia hospitalizations among patients with HFpEF who started spironolactone between 2013 and 2018 (crude incidence rate: 9.8 per 1000 patient-years) [92].
Humanistic burden
The impact of HFmrEF/HFpEF on patients' HRQoL is substantial; it is associated with a wide range of symptoms and functional limitations that affect daily activities, physical abilities, and emotional well-being. The Kansas City Cardiomyopathy Questionnaire (KCCQ) was the most commonly used tool across the identified studies, for both RCTs (8 studies) and RWE (7 studies). The KCCQ has been qualified by the US Food and Drug Administration (FDA) as a clinical outcome assessment for HF and is recommended for measuring care quality. Regulatory bodies, including the European Medicines Agency and FDA, have utilized it in drug assessments [93, 94]. The KCCQ scale is considered a reliable and sensitive to clinical change tool, that has been validated for both HFrEF and HFpEF patients, with a 5-point improvement considered a minimal clinically important difference [95, 96]. Therefore, we focused our results on the KCCQ tool. The KCCQ is a 23-item, self-administered questionnaire that quantifies seven domains impacting HF patients' lives, including their physical and social limitations, symptom frequency and severity, quality of life, recent changes in symptom status, and self-efficacy. The symptom frequency and symptom burden are merged into a total symptom score, which combined with the physical limitation domain create an overall clinical score. An overall summary score comprising the total symptom score, physical limitation, quality of life and social limitation domains. Scores for each domain range from 0 to 100, with higher scores indicating a lower symptom burden and better quality of life. The scores are categorized to represent health status as follow: 0 to 24 (very poor to poor), 25 to 49 (poor to fair), 50 to 74 (fair to good), and 75 to 100 (good to excellent) [97].
Health-related quality of life in randomized controlled trials
Overall, 15 trials reported results for HRQoL in the population of patients with HFpEF and or HFmrEF. The change in the KCCQ total symptom score from baseline to month 8 showed that dapagliflozin provided benefits compared with the placebo for symptoms of HF [win ratioFootnote 1: 1.11 (95% CI: 1.03–1.21)], P = 0.009) [79]. Another study revealed that dapagliflozin significantly improved the KCCQ clinical summary score (P = 0.001), the total symptom score (P = 0.003), and the physical limitations score (P = 0.026) compared with placebo; patients treated with dapagliflozin rather than placebo had a ≥ 5-point improvement in overall KCCQ score [adjusted odds ratio (OR): 1.73 (95% CI: 1.05–2.85), P = 0.03] [80]. Similarly, empagliflozin improved HRQoL, including KCCQ clinical summary, total symptom, and overall summary scores compared with the placebo at 12 weeks; this effect was durable up to 52 weeks. This finding was supported by a responder analysis. At 12 weeks, patients on empagliflozin had higher odds of improvement ≥ 5 points [OR: 1.23 (95% CI, 1.10–1.37)], ≥ 10 points [OR: 1.15 (95% CI, 1.03–1.27)], and ≥ 15 points [OR: 1.13 (95% CI, 1.02–1.26)], as well as lower odds of deterioration ≥ 5 points in KCCQ clinical summary score [OR: 0.85 (95% CI, 0.75–0.97)] compared with placebo. A similar pattern was seen at 32 and 52 weeks, and the results were consistent for the total symptom and overall summary scores [78]. In the PARALAX trial, an improvement in KCCQ score was observed; however, no significant differences between sacubitril/valsartan and the control group were reported in the mean change in the KCCQ clinical summary score from the baseline. The proportion of patients experiencing an improvement or decrease by ≥ 5 points was similar in both treatment groups [32]. In PARAGON, a decrease in the KCCQ clinical summary score was observed and the mean change at 8 months was 1.0 point higher in the sacubitril/valsartan group compared with the valsartan group [85]. A higher percentage of patients in the sacubitril/valsartan group than in the valsartan group had an improvement of ≥ 5 points in their KCCQ clinical summary score (33.0% vs 29.6%; OR: 1.30; 95% CI, 1.04–1.61) [85]. The results showed that spironolactone led to better patient-reported outcomes. In the TOPCAT trial, the spironolactone group had a significantly higher mean change in KCCQ compared with the placebo group at months 4 (P = 0.002) and 12 (P = 0.02), but this effect was not seen at the end of the study. At 4 months, spironolactone also improved the KCCQ clinical summary and symptom scores compared with placebo, but these improvements did not persist beyond 4 months. There were no significant differences among the treatment groups in the other KCCQ domains (social interference, physical scores, and quality of life) during the follow-up period [98].
Health-related quality of life in real-world evidence studies
Overall, 11 RWE studies reported HRQoL results in patients with HFmrEF/HFpEF. The real-world data indicated a decline in overall KCCQ scores in patients with HFpEF compared with HFmrEF. In the BIOSTAT-CHF study, patients with HFpEF reported more physical limitations, increased symptom frequency, and greater symptom burden, as well as having more social limitations [99]. Additionally, it was observed that most non-cardiac comorbidities (diabetes mellitus, obesity, thyroid dysfunction, CKD, stroke, COPD, peripheral artery disease, and anemia) were associated with a significant decline in the overall KCCQ score. For patients with HFmrEF or HFpEF, each comorbidity—except for peripheral artery disease in HFpEF—was associated with a decline in the score. For HFmrEF, all comorbidities except for CKD (mean difference of 4.48 points; 4.96 points for stroke) had minimal clinically important differences; for HFpEF, the only comorbidities with a minimal clinically important difference were COPD (mean difference of 10.8 points) and thyroid dysfunction (mean difference of 4.9 points) [99]. One study revealed a correlation between overall KCCQ summary scores and NYHA class. Higher scores were observed for lower NYHA classes and vice versa in HFpEF (r = − 0.62, P < 0.001) patients. Similarly, KCCQ total symptom domain scores showed a significant correlation with NYHA class in HFpEF (r = − 0.61, P < 0.001) patients [96].
Economic burden
Overall, 4 RWE publications reported outcomes for direct costs in patients with HFpEF and 10 reported outcomes for direct resource use for hospitalizations due to HFpEF and/or HFmrEF. Nevertheless, the available data are primarily limited to the United States. A study conducted in the United States from 2012 to 2018 revealed that the average per-patient monthly cost for healthcare was $7482. This cost was primarily driven by high rates of inpatient and outpatient visits, with costs of $4668 for inpatient stays, $2318 for outpatient visits, and $495 for medications [100]. Another US study conducted from 2008 to 2018 indicated that although the number of hospitalizations increased, the median inpatient costs of hospitalization due to HFpEF decreased from $9071 in 2008 to $8306 in 2018. This increase in the number of hospitalizations was related to changes in HF coding practices over time; however, the decrease in the inpatient costs of HF hospitalization may be due to improved management of HF exacerbations, enhanced outpatient management, and new therapeutic agents [88]. A comparison of healthcare resource use among HFmrEF and HFpEF patients in the United States (2007–2018) showed that the length of stay in the cardiac intensive care unit (CICU) and in hospital was longer in patients with HFmrEF than HFpEF (median length: 8.5 vs 6.9 days and 2.8 vs 2 days, respectively) [73]. In the United States, the length of stay was relatively stable over time; the length of hospital stays per patient ranged between 4 and 5 days per year for adult patients with HFpEF [100]. In Japan, the length of stay was longer than in the United States and ranged between 17 and 38 days [63, 101].
Pharmacologic treatment
Guideline-directed pharmacologic therapy
Guideline-directed pharmacologic therapy for HFmrEF and HFpEF focuses on reducing congestion symptoms with diuretics and treating underlying comorbidities (Table 5). Limited evidence exists of specific treatments for HFmrEF, and no prospective RCTs have been conducted exclusively for HFmrEF patients. Commonly considered drugs for HFmrEF treatment include diuretics, ACE-Is, ARBs, beta-blockers, MRA, and ARNIs (Table 5). Recent treatment options for HFmrEF/HFpEF include sacubitril/valsartan (an ARNI), empagliflozin, and dapagliflozin (SGLT-2is). In 2021, the FDA approved sacubitril/valsartan's indication extension, based on the PARAGON‐HF trial, to include certain HFpEF patients with reduced ejection fractions. Now, its use is indicated for patients with chronic HF, and the benefits are most clearly seen in patients with a below normal LVEF, although the exact definition of a normal LVEF has not been provided [10, 102, 103]. In Europe, sacubitril/valsartan is currently approved only for patients with HFrEF [104]. Empagliflozin and dapagliflozin were initially approved for type 2 diabetes [6,7,8,9]; later, they were also approved for HFrEF [104, 105]. Subsequently, in 2022, empagliflozin’s indication was extended in Europe and the United States, making it the first therapy approved for adults with HFmrEF/HFpEF [106]. This was followed by dapagliflozin’s approval in the United Kingdom (2022) [107], Europe (2023) [8], and the United States (2023) for symptomatic chronic HF, including HFmrEF/HFpEF, in adult patients [9, 108]. In Japan, sacubitril/valsartan, dapagliflozin, and empagliflozin were also approved for use in the broad chronic HF population, but whether there are any limitations on HFrEF/HFmrEF/HFpEF patients in their indications has not been clearly stated [109, 110]. Clinical guidelines are beginning to incorporate SGLT-2is and ARNI recommendations for HFmrEF/HFpEF based on new evidence. American Heart Association (AHA), American College of Cardiology (ACC), and Heart Failure Society of America (HFSA) 2022 guidelines in the United States recommended SGLT-2is based on the EMPEROR-Preserved study for HFmrEF/HFpEF [2]. Multiple other guidelines, with similar classes of recommendation and levels of evidence, recommended an ARNI (sacubitril/valsartan) based on PARAGON-HF and combined PARADIGM-HF/PARAGON-HF analyses for HFmrEF/HFpEF (Table 6).
Real-world practice
Studies on HFpEF and/or HFmrEF patients reported real-world treatment patterns as percentages for different therapies [13, 36,37,38,39,40, 43, 44, 46, 47, 49, 50, 60, 62, 63, 65, 68, 69, 76, 77, 90,91,92, 100, 111]. Commonly used medications included beta-blockers, renin-angiotensin system inhibitors (RASIs), diuretics (loop or thiazide), ACE-Is/ARBs (in combination or separately), anti-coagulants, and calcium channel blockers, as well as statins and MRAs. SGLT-2i use in real-life has rarely been reported. No significant differences in treatment patterns were found among patients with HFpEF and HFmrEF [13, 36,37,38,39,40, 43, 44, 46, 47, 49, 50, 60, 62, 63, 65, 68, 69, 76, 77, 90,91,92, 100, 111].
Discussion
This TLR provides up-to-date data on the epidemiology, burden of illness, and current pharmacologic landscape of HFmrEF/HFpEF, alongside identifying unmet needs and knowledge gaps.
The literature indicates a lack of consensus regarding the characterization and diagnosis of HFpEF and HFmrEF, with variation in diagnostic criteria observed across scientific society guidelines and clinical trials. This variation partly arises from an incomplete understanding of disease pathophysiology and the heterogenous nature of the disease which involves a multitude of contributing risk factors, causes, and phenotypic manifestations [26, 112]. Our results reveal a concerning gap in understanding regarding the predictors and risk factors of HFmrEF/HFpEF, which confirms the needs for additional research to better understand such factors and natural history. Given the persisting challenges in HFpEF diagnosis, various scientific societies have proposed specific diagnostic criteria, tools, and algorithms, which are referenced in key guidelines (although not discussed within the context of HFmrEF). However, the additional validation of these scoring tools and their practical applicability in routine clinical practice are still subject to discussion [1,2,3, 17, 26]. To date, RCTs mainly refer to a documented diagnosis of symptomatic HF with typical symptoms/signs of HF combined with LVEF thresholds of ≥ 40%, ≥ 45% or ≥ 50%, evidence of structural heart disease or hospitalization for HF within 12 months, as well as elevated NT-proBNP threshold. The potential impact of evolving diagnostic criteria on the definition of RCT populations in the future remains to be evaluated. In addition, inconsistencies exist in the definition of subgroups of patients whose EF transitioned among guidelines. These variations may contribute to the complexity of patient classification and tailored management strategies. On the other hand, real-world results indicate an increase in HF hospitalizations, especially in cases of HFpEF, possibly because of changes in coding practices, emphasizing the need for an accurate HF classification [87].
Approximately 50% of patients with symptomatic HF are reported to have HFpEF, while HFmrEF is less common. The recent incidence and epidemiology trends data identified for the selected geographical scope were relatively scarce, because most epidemiology data were reported before 2016, cut-off date of our review. Moreover, most epidemiology data refer to HFpEF rather than HFmrEF.
Epidemiology data were found to be heterogeneous, reflecting the heterogeneity of HFmrEF/HFpEF disease. Furthermore, estimates of HFpEF and HFmrEF prevalence varied among countries, and caution is advised when interpreting these estimates because of the variations in definitions and study characteristics across different regions and populations. Another important aspect that may have influenced the prevalence estimates is the changes in the definition of HF provided by the guidelines over time [47]. A study in Germany assessed the impact of these changes between the 2016 ESC HF guidelines and the 2021 ESC guidelines, finding notable differences in prevalence estimates for HFpEF and HFmrEF. This review found that HF prevalence in the middle-aged general population increased by 12% (4.8% with 2021 definition), HFmrEF increased by 54% (2.12% with 2021 definition), and HFpEF decreased by 11% (2.19% with 2021 definition) [47]. Previous reviews by Savarese et al. [113], Groenewegen et al. [11], and Dunlay et al. [12] also observed wide variations in HFmrEF/HFpEF prevalence across countries, and a decline in HFpEF incidence was observed, although the results were relatively old, with the most recent incidence results being from 2015.
HFmrEF/HFpEF is associated with considerable mortality. However, HFmrEF/HFpEF exhibits varying mortality rates because of factors like study design, follow-up duration, patient characteristics, treatment approaches, and HFmrEF/HFpEF definitions, making it hard to derive a range. The mortality risk can differ for various types of HF. HFmrEF tends to have lower all-cause mortality compared to HFpEF, potentially due to its lower risk characteristics, as explained by Jentzer et al. [73]. In another study, patients with HFmrEF share more similar characteristics with HFrEF than with HFpEF, yet HFpEF and HFmrEF still exhibit comparable mortality rates, both of which are lower than the mortality rates seen in HFrEF [1]. This may be due to their higher LVEF; previous studies have indicated that recovery from a reduced LVEF is linked to better outcomes [114,115,116,117]. In a study by Borlaug et al., HFpEF and HFrEF patients showed similarly poor survival rates, but differed in causes of death. HFpEF had fewer cardiovascular and more non-cardiovascular deaths compared to HFrEF. This highlights the significance of effectively managing non-cardiac comorbidities in HFpEF [112]. Mortality rates in RWE studies were higher than RCTs because of differences in patient populations. RCTs typically include younger, healthier individuals with fewer underlying health conditions, who are closely monitored in outpatient settings with shorter follow-up periods.
HFmrEF/HFpEF is associated with considerable morbidity and poor reported patient outcomes. Key co-morbidities are well identified in the HFmrEF/HFpEF setting, with the main common ones being hypertension, atrial fibrillation, stroke, diabetes, obesity, COPD, and CKD. Two studies by Chamberlain et al. highlight an association between HF and a higher prevalence of comorbidities, which vary based on HF type, age, and sex [118, 119]. Notably, comorbidities were more common in men, and patients with HFpEF had an additional condition compared with HFrEF (mean: 4.5 vs 3.7). This underscores the importance of considering HF type when addressing comorbidities and tailoring treatment approaches accordingly [119].
Patients with HFmrEF/HFpEF require frequent hospitalizations. Patients with HFpEF face a higher rate of the first hospitalization for HF than patients with HFmrEF (9.6 vs 8.9 per 100 patient-years), while HF hospital readmission rates are similar between HFpEF and HFmrEF (44.6% vs 40.1% for the first readmission and 23.3% for HFmrEF vs 17.1% for the second readmission, respectively) [13, 120]. The high disease morbidity is impacting the HRQoL of patients with HFmrEF/HFpEF. Patients with HFpEF yield poorer PROs, impacting QoL (overall KCCQ scores), compared to those with HFmrEF or HFrEF. This impact is further heightened by frequently associated non-cardiac comorbidities like T2D, CKD, and obesity. In a study by Joseph (2013), NYHA class correlated with KCCQ scores in both HFpEF and HFmrEF groups, suggesting that HRQoL could be related to factors other than EF, such as symptom severity [96].
As a result, early intervention is crucial to prevent disease burden. Optimizing the prevention and treatment of these conditions could potentially prevent a substantial number of HF cases [118]. RCT results suggest that interventions in HFpEF and HFmrEF, particularly SGLT-2is like dapagliflozin and empagliflozin, reduce the risk of CV death or HF hospitalization [79, 80]. Although the mortality reduction was limited, the significant decrease in HF hospitalization risk shows promise for the improvement of HFmrEF/HFpEF management and outcomes [79, 80]. Treatments for HFpEF and/or HFmrEF demonstrated promising safety profiles overall, with specific side effects observed for some drugs, such as hypotension and hyperkalemia for sacubitril/valsartan [32, 80]. More research in real-world settings is needed to better understand the safety implications, especially in the long term. Some studies have found positive effects on HRQoL with SGLT-2is, particularly dapagliflozin [80] and empagliflozin [78]. However, sacubitril/valsartan did not significantly impact HRQoL [32]. Spironolactone showed short-term improvements in patient-reported outcomes but not in the longer term [98]. Although some KCCQ scores reached statistical significance, the clinical relevance of the differences was uncertain, as indicated in regulatory reports. The mean differences in KCCQ scores for both SGLT-2is and sacubitril/valsartan were not clinically meaningful. For empagliflozin, the change in the KCCQ clinical summary score from the baseline at week 52 was statistically significant but modest, raising doubts regarding its clinical relevance [102, 121, 122]. The proportion of patients achieving a clinically relevant change (5 points) was slightly higher in the empagliflozin group (41.7%) compared with the placebo group (38.7%), but the difference in the percentage was small. Other KCCQ scores also showed treatment differences, although they were, again, considered small and not clinically relevant [123].
Data on costs and resource utilization in patients with HFmrEF/HFpEF are scarce. Nonetheless, this TLR highlights the increasing economic burden. High healthcare costs per patient and rising hospitalizations call for more cost-effective management strategies. On the other hand, the available data are primarily limited to the United States, so future research should explore the global economic impact and assess the long-term effects of different management approaches.
Although treatments for HFrEF are established and effective, until recently, there was an important evidence gap in relation to therapeutic options that provide significant benefits for patients with HFmrEF/HFpEF. Three new drugs have entered the HFpEF space since 2020, with promising data from their clinical trials. Sacubitril/valsartan was approved in patients with HF and a below normal LVEF based on the PARAGON-HF trial [10]. Later, empagliflozin was approved for HFmrEF/HFpEF in 2022 based on data from the EMPEROR-Preserved trial [6, 7, 9], with dapagliflozin arriving on the market in 2022/2023 as a result of data obtained from the DELIVER trial [8, 9]. Real-world studies indicate that the utilization of SGLT-2is has thus far been limited, which may be because of their recent introduction, but this is expected to increase with accumulating evidence. Guidelines are starting to integrate recommendations for SGLT-2is in HFmrEF/HFpEF, driven by emerging evidence. This includes specific recommendations for empagliflozin which are supported by trial outcomes within the HFmrEF/HFpEF population. Notably, organizations such as the American Heart Association (AHA), American College of Cardiology (ACC), and Heart Failure Society of America (HFSA) in 2022 have contributed to these evolving guidelines [2]. According to recent updates, SGLT-2is (empagliflozin and dapagliflozin) were recently recommended by Japanese guidelines for patients with HF regardless of LVEF [124]. More recently, a focused update of the 2021 ESC guidelines was published in August 2023, which also recommends empagliflozin and dapagliflozin for patients with HFmrEF/HFpEF [125].
In addition, there is a growing focus on HFmrEF/HFpEF indication, with four products (tirzepatide [126], semaglutide [127], ziltivekimab [128], and mitiperstat [129]) in phase 3 of development. However, most of these trials are being conducted in restricted populations with specific comorbidities, such as obesity and/or type 2 diabetes [126,127,128,129]. Moreover, in May 2023, the FDA approved the first dual SGLT-1 and SGLT-2 inhibitor, sotagliflozin, for the broad treatment of HF, based on phase 3 results from the SCORED trial and the SOLOIST-WHF trial [105, 130].
Despite the introduction of new drugs, unmet medical needs remain and new therapeutic options for HFmrEF/HFpEF are required, because there has been no demonstrably clear effect on mortality in dedicated HFmrEF/HFpEF trials (CV death or all-cause mortality), the change in KCCQ total symptom score is not deemed clinically meaningful, and there are specific safety warnings for gliflozins.
This review’s inclusion of a wide range of publications, including RCTs, RWE publications, and guidelines from various locations, ensures a comprehensive and up-to-date summary of the published literature in this field. However, this TLR has some limitations, including the choice of the TLR over the SLR methodology, potentially affecting the comprehensiveness of the findings, and the study prioritization process, which might have excluded some relevant studies. Nevertheless, this is balanced by the assurance that crucial data were obtained by examining recent reviews/SLRs from the past 2–3 years concerning the same subject. Finally, publication bias and geographical restrictions may have influenced the generalizability of the findings.
Conclusions
HFmrEF and HFpEF present a meaningful and growing burden on the global healthcare system. Recent advances have improved our understanding of the epidemiology, pathophysiology, and diagnosis of these conditions, along with the approval of drugs offering promising treatment options. However, there remain key knowledge gaps in terms of the burden of illness and unmet medical needs requiring alternative treatment approaches. Further research and efforts are needed to address these gaps and develop more effective strategies to manage and improve outcomes for patients with HFmrEF/HFpEF.
Data availability
This manuscript has data included as supplementary material.
Notes
Authors analyzed the KCCQ total symptom score as a composite outcome based on the rank of the change in score from baseline to moth 8, with a corresponding win ratio used to estimate the magnitude of the treatment effect.
References
McDonagh TA, Metra M, Adamo M et al (2021) 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: Developed by the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) With the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 42(36):3599–3726. https://doi.org/10.1093/eurheartj/ehab368
Heidenreich PA, Bozkurt B, Aguilar D et al (2022) 2022 AHA/ACC/HFSA guideline for the management of heart failure: A report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation 145(18):e895–e1032. https://doi.org/10.1161/CIR.0000000000001063
Tsutsui H, Ide T, Ito H et al (2021) JCS/JHFS 2021 guideline focused update on diagnosis and treatment of acute and chronic heart failure. Circ J 85(12):2252–2291. https://doi.org/10.1253/circj.CJ-21-0431
Teramoto K, Teng T-HK, Chandramouli C, Tromp J, Sakata Y, Lam CSP (2022) Epidemiology and clinical features of heart failure with preserved ejection fraction. Card Fail Rev 8:e27. https://doi.org/10.15420/cfr.2022.06
Shah SJ, Borlaug BA, Kitzman DW et al (2020) Research priorities for heart failure with preserved ejection fraction. Circulation 141(12):1001–1026. https://doi.org/10.1161/CIRCULATIONAHA.119.041886
European Medicines Agency (2022) Jardiance Summary of Product Characteristics. Boehringer Ingelheim. https://www.ema.europa.eu/en/documents/product-information/jardiance-epar-product-information_en.pdf. Accessed 7 Nov 2023
US Food and Drug Administration (2023) Jardiance prescribing information. Boehringer Ingelheim. https://content.boehringer-ingelheim.com/DAM/7d9c411c-ec33-4f82-886f-af1e011f35bb/jardiance-us-pi.pdf. Accessed 7 Nov 2023
European Medicines Agency (2023) Forxiga Summary of Product Characteristics. AstraZeneca. https://www.ema.europa.eu/en/documents/product-information/forxiga-epar-product-information_en.pdf
US Food and Drug Administration (2023) Farxiga prescribing information AstraZeneca. https://www.accessdata.fda.gov/drugsatfda_docs/label/2023/202293s026lbl.pdf. Accessed 7 Nov 2023
US Food and Drug Administration (2021) Entresto prescribing information. Novartis. https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/207620s018lbl.pdf. Accessed 7 Nov 2023
Groenewegen A, Rutten FH, Mosterd A, Hoes AW (2020) Epidemiology of heart failure. Eur J Heart Fail 22(8):1342–1356. https://doi.org/10.1002/ejhf.1858
Dunlay SM, Roger VL, Redfield MM (2017) Epidemiology of heart failure with preserved ejection fraction. Nat Rev Cardiol 14(10):591–602. https://doi.org/10.1038/nrcardio.2017.65
Savarese G, Hage C, Benson L et al (2021) Eligibility for sacubitril/valsartan in heart failure across the ejection fraction spectrum: real-world data from the Swedish Heart Failure Registry. J Intern Med 289(3):369–384. https://doi.org/10.1111/joim.13165
Higgins J, Thomas J, Chandler J, Cumpston M, Li T, Page M, Welch V (2022) Cochrane Handbook for Systematic Reviews of Interventions version 6.3 (updated February 2022). Cochrane. www.training.cochrane.org/handbook. Accessed 7 Nov 2023
Centre for Reviews and Dissemination (2009) Systematic Reviews: CRD’s guidance for undertaking reviews in health care. CRD, University of York. https://www.york.ac.uk/media/crd/Systematic_Reviews.pdf. Accessed 7 Nov 2023
Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P (2012) The Newcastle-Ottawa Scale (NOS) for assessing the quality if nonrandomized studies in meta-analyses. The Ottawa Hospital. http://www.hrica/programs/clinical_epidemiology/oxfordasp. Accessed 7 Nov 2023
DGK (2021) Acute and chronic HF, Version 2021. German Cardiac Society, Düsseldorf, Germany
HAS (2014) Guide Du Parcours De Soins. Insuffisance cardiaque. https://www.has-sante.fr/upload/docs/application/pdf/2012-04/guide_parcours_de_soins_ic_web.pdf. Accessed 7 Nov 2023
IQWiG (2021) Leitliniensynopse für die Aktualisierung des DMP Herzinsuffizienz. Auftrag: V20-05, Version: 1.0, Stand: 19.07.2021. https://www.iqwig.de/download/v20-05_dmp-herzinsuffizienz_vorbericht_v1-0.pdf. Accessed 7 Nov 2023
LOK nätverket för Sveriges läkemedelskommittéer (2022) Drug treatment in chronic HF. Pharmaceutical Committees’ National Network, Stockholm
NBHW (2018) National guidelines for cardiac care. National Board of Health and Welfare (Socialstyrelsen), Stockholm
NICE (2018) Chronic heart failure in adults: diagnosis and management. National Institute for Health and Care Excellence, London
NVL (2019) National care guideline: chronic health failure. National Health Care Guidelines, Berlin
SKS (2021) Person-centred and integrated care course in HF. Swedish Knowledge Support, Stockholm
SMA (2015) HF: therapy recommendations (se. Hjärtsvikt). Swedish Medicines Agency. https://lakemedelsboken.se/kapitel/hjarta-karl/hjartsvikt.html. Accessed 7 Nov 2023
Pieske B, Tschope C, de Boer RA et al (2020) How to diagnose heart failure with preserved ejection fraction: the HFA-PEFF diagnostic algorithm: a consensus recommendation from the Heart Failure Association (HFA) of the European Society of Cardiology (ESC). Eur J Heart Fail 22(3):391–412. https://doi.org/10.1002/ejhf.1741
Edelmann F, Knosalla C, Mörike K, Muth C, Prien P, Störk S (2018) Clinical Practice Guideline Chronic Heart Failure. Dtsch Arztebl Int 115(8):124–130. https://doi.org/10.3238/arztebl.2018.0124
Hanon O, Belmin J, Benetos A et al (2021) Consensus of experts from the French Society of Geriatrics and Gerontology on the management of heart failure in very old subjects. Arch Cardiovasc Dis 114(3):246–259. https://doi.org/10.1016/j.acvd.2020.12.001
HAS (2015) Heart failure with preserved systolic function Acts and benefits–long-term condition. French National Authority for Health, Paris
Kasiakogias A, Rosei EA, Camafort M et al (2021) Hypertension and heart failure with preserved ejection fraction: position paper by the European Society of Hypertension. J Hypertens 39(8):1522–1545. https://doi.org/10.1097/HJH.0000000000002910
CaReMeUK-HF (2022) HF management algorithm. British Cardiovascular Society. https://www.britishcardiovascularsociety.org/resources/careme. Accessed 7 Nov 2023
Pieske B, Wachter R, Shah SJ et al (2021) Effect of sacubitril/valsartan vs standard medical therapies on plasma NT-proBNP concentration and submaximal exercise capacity in patients with heart failure and preserved ejection fraction: The PARALLAX randomized clinical trial. JAMA 326(19):1919–1929. https://doi.org/10.1001/jama.2021.18463
Sakata Y, Shiba N, Takahashi J et al (2015) Clinical impacts of additive use of olmesartan in hypertensive patients with chronic heart failure: the supplemental benefit of an angiotensin receptor blocker in hypertensive patients with stable heart failure using olmesartan (SUPPORT) trial. Eur Heart J 36(15):915–923. https://doi.org/10.1093/eurheartj/ehu504
Bhatt DL, Szarek M, Pitt B et al (2020) Sotagliflozin in patients with diabetes and chronic kidney disease. N Engl J Med 384(2):129–139. https://doi.org/10.1056/NEJMoa2030186
Feng M, He B, Wang B, Chen X, Chu H (2022) Clinical study of heart failure with left ventricular ejection fraction regimen treated with entresto. Contrast Media Mol Imaging 2022:4164089. https://doi.org/10.1155/2022/4164089
Uijl A, Savarese G, Vaartjes I et al (2021) Identification of distinct phenotypic clusters in heart failure with preserved ejection fraction. Eur J Heart Fail 23(6):973–982. https://doi.org/10.1002/ejhf.2169
Harmon D, Rathousky J, Choudhry F et al (2020) Readmission risk factors and heart failure with preserved ejection fraction. J Am Osteopath Assoc 120(12):831–838. https://doi.org/10.7556/jaoa.2020.154
Hage C, Svedlund S, Saraste A et al (2020) Association of coronary microvascular dysfunction with heart failure hospitalizations and mortality in heart failure with preserved ejection fraction: A follow-up in the PROMIS-HFpEF study. J Card Fail 26(11):1016–1021. https://doi.org/10.1016/j.cardfail.2020.08.010
Shah SJ, Lam CSP, Svedlund S et al (2018) Prevalence and correlates of coronary microvascular dysfunction in heart failure with preserved ejection fraction: PROMIS-HFpEF. Eur Heart J 39(37):3439–3450. https://doi.org/10.1093/eurheartj/ehy531
Takahari K, Hidaka T, Ueda Y et al (2019) H(2)FPEF score for the prediction of exercise intolerance and abnormal hemodynamics in Japanese–evaluation by exercise stress echocardiography combined with cardiopulmonary exercise testing. Circ J 83(12):2487–2493. https://doi.org/10.1253/circj.CJ-19-0699
Yoshihisa A, Sato Y, Kanno Y et al (2020) Prognostic impacts of changes in left ventricular ejection fraction in heart failure patients with preserved left ventricular ejection fraction. Open Heart 7(1):e001112. https://doi.org/10.1136/openhrt-2019-001112
Hornsby WE, Sareini MA, Golbus JR, Willer CJ, McNamara JL, Konerman MC, Hummel SL (2019) Lower extremity function is independently associated with hospitalization burden in heart failure with preserved ejection fraction. J Card Fail 25(1):2–9. https://doi.org/10.1016/j.cardfail.2018.09.002
Fudim M, Kelly JP, Brophy TJ et al (2020) Trends in treatment for patients hospitalized with heart failure with preserved ejection fraction before and after treatment of preserved cardiac function heart failure with an aldosterone antagonist (TOPCAT). Am J Cardiol 125(11):1655–1660. https://doi.org/10.1016/j.amjcard.2020.02.038
Meyer M, Du Fay LJ, Benson L, Savarese G, Dahlström U, Lund LH (2021) Association between β-blockers and outcomes in heart failure with preserved ejection fraction: current insights from the SwedeHF registry. J Card Fail 27(11):1165–1174. https://doi.org/10.1016/j.cardfail.2021.04.015
Bekfani T, Pellicori P, Morris D et al (2019) Iron deficiency in patients with heart failure with preserved ejection fraction and its association with reduced exercise capacity, muscle strength and quality of life. Clin Res Cardiol 108(2):203–211. https://doi.org/10.1007/s00392-018-1344-x
Perry AS, Mudigonda P, Huang GS, Qureshi B, Cheng RK, Levy WC, Li S (2022) Long-term outcomes and risk stratification of patients with heart failure with recovered ejection fraction. Am J Cardiol 173:80–87. https://doi.org/10.1016/j.amjcard.2022.03.006
Wenzel JP, Nikorowitsch J, Bei der Kellen R et al (2022) Heart failure in the general population and impact of the 2021 European Society of Cardiology Heart Failure Guidelines. ESC Heart Fail 9(4):2157–2169. https://doi.org/10.1002/ehf2.13948
Davies DR, Redfield MM, Scott CG et al (2022) A simple score to identify increased risk of transthyretin amyloid cardiomyopathy in heart failure with preserved ejection fraction. JAMA Cardiol 7(10):1036–1044. https://doi.org/10.1001/jamacardio.2022.1781
Brann A, Janvanishstaporn S, Greenberg B (2020) Association of prior left ventricular ejection fraction with clinical outcomes in patients with heart failure with midrange ejection fraction. JAMA Cardiol 5(9):1027–1035. https://doi.org/10.1001/jamacardio.2020.2081
Li DL, Quispe R, Onyekwelu C, Faillace RT, Taub CC (2019) Racial differences of heart failure with midrange ejection fraction (HFmrEF): a large urban centre-based retrospective cohort study in the USA. BMJ Open 9(4):e026479. https://doi.org/10.1136/bmjopen-2018-026479
Cosentino F, Cannon CP, Cherney DZI et al (2020) Efficacy of ertugliflozin on heart failure-related events in patients with type 2 diabetes mellitus and established atherosclerotic cardiovascular disease: Results of the VERTIS CV trial. Circulation 142(23):2205–2215. https://doi.org/10.1161/circulationaha.120.050255
Cannon CP, Pratley R, Dagogo-Jack S et al (2020) Cardiovascular outcomes with ertugliflozin in type 2 diabetes. N Engl J Med 383(15):1425–1435. https://doi.org/10.1056/NEJMoa2004967
Kato ET, Silverman MG, Mosenzon O et al (2019) Effect of dapagliflozin on heart failure and mortality in type 2 diabetes mellitus. Circulation 139(22):2528–2536. https://doi.org/10.1161/CIRCULATIONAHA.119.040130
Szarek M, Bhatt DL, Steg PG et al (2021) Effect of Sotagliflozin on Total Hospitalizations in Patients With Type 2 Diabetes and Worsening Heart Failure : A Randomized Trial. Ann Intern Med 174(8):1065–1072. https://doi.org/10.7326/m21-0651
Miura M, Sakata Y, Miyata S et al (2016) Influence of left ventricular ejection fraction on the effects of supplemental use of angiotensin receptor blocker olmesartan in hypertensive patients with heart failure. Circ J 80(10):2155–2164. https://doi.org/10.1253/circj.CJ-16-0577
Tromp J, Lim SL, Tay WT et al (2019) Microvascular disease in patients with diabetes with heart failure and reduced ejection versus preserved ejection fraction. Diabetes Care 42(9):1792–1799. https://doi.org/10.2337/dc18-2515
Subramaniam AV, Weston SA, Killian JM et al (2022) Development of advanced heart failure: a population-based study. Circ Heart Fail 15(5):e009218. https://doi.org/10.1161/circheartfailure.121.009218
Ho JE, Redfield MM, Lewis GD, Paulus WJ, Lam CSP (2020) Deliberating the diagnostic dilemma of heart failure with preserved ejection fraction. Circulation 142(18):1770–1780. https://doi.org/10.1161/CIRCULATIONAHA.119.041818
Garg P, Dakshi A, Assadi H et al (2021) Characterisation of the patients with suspected heart failure: experience from the SHEAF Registry. Open Heart 8(1):e001448. https://doi.org/10.1136/openhrt-2020-001448
Cohen-Solal A, Philip JL, Picard F et al (2022) Iron deficiency in heart failure patients: the French CARENFER prospective study. ESC Heart Fail 9(2):874–884. https://doi.org/10.1002/ehf2.13850
Lindberg F, Lund LH, Benson L et al (2022) Patient profile and outcomes associated with follow-up in specialty vs. primary care in heart failure. ESC Heart Fail 9(2):822–833. https://doi.org/10.1002/ehf2.13848
Lorenzo CJ, Conte JI, Villasmil RJ, Abdelal QK, Pierce D, Wiese-Rometsch W, Garcia-Fernandez JA (2022) Heart failure ejection fraction class conversions: impact of biomarkers, co-morbidities, and pharmacotherapy. ESC Heart Fail 9(4):2538–2547. https://doi.org/10.1002/ehf2.13965
Shiga T, Suzuki A, Haruta S et al (2019) Clinical characteristics of hospitalized heart failure patients with preserved, mid-range, and reduced ejection fractions in Japan. ESC Heart Fail 6(3):475–486. https://doi.org/10.1002/ehf2.12418
An M, Mehta A, Min BH et al (2023) Sequential pembrolizumab cooperates with platinum/5FU to remodel the tumor microenvironment in advanced gastric cancer: a phase II chemoimmunotherapy trial. medRxiv. https://doi.org/10.1101/2023.04.03.23288062
Ibrahim NE, Song Y, Cannon CP et al (2019) Heart failure with mid-range ejection fraction: characterization of patients from the PINNACLE Registry®. ESC Heart Fail 6(4):784–792. https://doi.org/10.1002/ehf2.12455
Göbel S, Prochaska JH, Tröbs SO et al (2021) Rationale, design and baseline characteristics of the MyoVasc study: A prospective cohort study investigating development and progression of heart failure. Eur J Prev Cardiol 28(9):1009–1018. https://doi.org/10.1177/2047487320926438
Aizawa N, Konishi M, Kitai T et al (2022) Infrequent use of nighttime dialysis for emergency admission due to worsening heart failure in patients on maintenance hemodialysis. Ther Apher Dial 26(1):85–93. https://doi.org/10.1111/1744-9987.13644
Tsukamoto K, Suzuki A, Shiga T, Arai K, Hagiwara N (2021) Changes in the left ventricular ejection fraction and outcomes in hospitalized heart failure patients with mid-range ejection fraction: a prospective observational study. Intern Med 60(10):1509–1518. https://doi.org/10.2169/internalmedicine.6388-20
Yoshihisa A, Ichijo Y, Sato Y et al (2020) Comprehensive clinical characteristics of hospitalized patients with mid-range left ventricular ejection fraction. Eur J Prev Cardiol 27(19):2084–2088. https://doi.org/10.1177/2047487319859689
Tromp J, Tay WT, Ouwerkerk W et al (2018) Multimorbidity in patients with heart failure from 11 Asian regions: A prospective cohort study using the ASIAN-HF registry. PLoS Med 15(3):e1002541. https://doi.org/10.1371/journal.pmed.1002541
Abraham WT, Lindenfeld J, Ponikowski P et al (2021) Effect of empagliflozin on exercise ability and symptoms in heart failure patients with reduced and preserved ejection fraction, with and without type 2 diabetes. Eur Heart J 42(6):700–710. https://doi.org/10.1093/eurheartj/ehaa943
Greenberg B, Peterson ED, Berger JS et al (2019) Ejection fraction, B-type natriuretic peptide and risk of stroke and acute myocardial infarction among patients with heart failure. Clin Cardiol 42(2):277–284. https://doi.org/10.1002/clc.23140
Jentzer JC, Reddy YN, Rosenbaum AN, Dunlay SM, Borlaug BA, Hollenberg SM (2022) Outcomes and predictors of mortality among cardiac intensive care unit patients with heart failure. J Card Fail 28(7):1088–1099. https://doi.org/10.1016/j.cardfail.2022.02.015
Fayol A, Wack M, Livrozet M et al (2022) Aetiological classification and prognosis in patients with heart failure with preserved ejection fraction. ESC Heart Fail 9(1):519–530. https://doi.org/10.1002/ehf2.13717
Alasdair H, Jingzhou H, Alice C, Stelios I, Phil K (2020) The impact of an integrated heart failure service in a medium-sized district general hospital. Open Heart 7(1):e001218. https://doi.org/10.1136/openhrt-2019-001218
Seki T, Kubota Y, Matsuda J, Tokita Y, Iwasaki YK, Shimizu W (2022) Clinical features and long-term prognosis of patients with congestive heart failure taking tolvaptan: a comparison of patients with preserved and reduced left ventricular ejection fraction. Heart Vessels 37(4):574–582. https://doi.org/10.1007/s00380-021-01957-1
Arnold SV, Echouffo-Tcheugui JB, Lam CSP et al (2018) Patterns of glucose-lowering medication use in patients with type 2 diabetes and heart failure. Insights from the Diabetes Collaborative Registry (DCR). Am Heart J 203:25–29. https://doi.org/10.1016/j.ahj.2018.05.016
Butler J, Filippatos G, Jamal Siddiqi T et al (2022) Empagliflozin, health status, and quality of life in patients with heart failure and preserved ejection fraction: The EMPEROR-Preserved Trial. Circulation 145(3):184–193. https://doi.org/10.1161/circulationaha.121.057812
Solomon SD, McMurray JJV, Claggett B et al (2022) Dapagliflozin in heart failure with mildly reduced or preserved ejection fraction. N Engl J Med 387(12):1089–1098. https://doi.org/10.1056/NEJMoa2206286
Nassif ME, Windsor SL, Borlaug BA et al (2021) The SGLT2 inhibitor dapagliflozin in heart failure with preserved ejection fraction: a multicenter randomized trial. Nat Med 27(11):1954–1960. https://doi.org/10.1038/s41591-021-01536-x
Anker SD, Siddiqi TJ, Filippatos G et al (2022) Outcomes with empagliflozin in heart failure with preserved ejection fraction using DELIVER-like endpoint definitions. Eur J Heart Fail 24(8):1400–1405. https://doi.org/10.1002/ejhf.2558
Anker SD, Butler J, Filippatos G et al (2021) Empagliflozin in heart failure with a preserved ejection fraction. N Engl J Med 385(16):1451–1461. https://doi.org/10.1056/NEJMoa2107038
Yusuf S, Pfeffer MA, Swedberg K et al (2003) Effects of candesartan in patients with chronic heart failure and preserved left-ventricular ejection fraction: the CHARM-Preserved Trial. Lancet 362(9386):777–781. https://doi.org/10.1016/s0140-6736(03)14285-7
Cleland JG, Tendera M, Adamus J, Freemantle N, Polonski L, Taylor J (2006) The perindopril in elderly people with chronic heart failure (PEP-CHF) study. Eur Heart J 27(19):2338–2345. https://doi.org/10.1093/eurheartj/ehl250
Solomon SD, McMurray JJV, Anand IS et al (2019) Angiotensin–neprilysin inhibition in heart failure with preserved ejection fraction. N Engl J Med 381(17):1609–1620. https://doi.org/10.1056/NEJMoa1908655
Pitt B, Pfeffer MA, Assmann SF et al (2014) Spironolactone for heart failure with preserved ejection fraction. N Engl J Med 370(15):1383–1392. https://doi.org/10.1056/NEJMoa1313731
Afzal A, van Zyl J, Nisar T et al (2022) Trends in hospital admissions for systolic and diastolic heart failure in the United States between 2004 and 2017. Am J Cardiol 171:99–104. https://doi.org/10.1016/j.amjcard.2022.01.047
Clark KAA, Reinhardt SW, Chouairi F et al (2022) Trends in heart failure hospitalizations in the US from 2008 to 2018. J Card Fail 28(2):171–180. https://doi.org/10.1016/j.cardfail.2021.08.020
Reinhardt SW, Chouairi F, Miller PE et al (2021) National trends in the burden of atrial fibrillation during hospital admissions for heart failure. J Am Heart Assoc 10(11):e019412. https://doi.org/10.1161/jaha.120.019412
Ambrosy AP, Parikh RV, Sung SH et al (2021) A natural language processing-based approach for identifying hospitalizations for worsening heart failure within an integrated health care delivery system. JAMA Netw Open 4(11):e2135152. https://doi.org/10.1001/jamanetworkopen.2021.35152
Desai RJ, Mahesri M, Chin K et al (2021) Epidemiologic characterization of heart failure with reduced or preserved ejection fraction populations identified using Medicare claims. Am J Med 134(4):e241–e251. https://doi.org/10.1016/j.amjmed.2020.09.038
Desai RJ, Solomon SD, Vaduganathan M (2022) Rates of spironolactone initiation and subsequent hyperkalemia hospitalizations in patients with heart failure with preserved ejection fraction following the TOPCAT trial: A cohort study of Medicare beneficiaries. J Card Fail 28(6):1035–1039. https://doi.org/10.1016/j.cardfail.2022.01.012
European Medicines Agency (2017) Guideline on clinical investigation of medicinal products for the treatment of chronic heart failure CPMP/EWP/235/95, Rev.2. 7 Nov 2023. https://www.ema.europa.eu/en/documents/scientific-guideline/guideline-clinical-investigation-medicinal-products-treatment-chronic-heart-failure-revision-2_en.pdf
Spertus J (2016) Medical Device Development Tool (MDDT) qualification decision summary for Kansas City Cardiomyopathy Questionnaire (KCCQ). St Luke's Mid America Heart Institute. https://www.fda.gov/media/108301/download. Accessed 7 Nov 2023
Huang W, Teng TK, Tay WT et al (2020) Patient-reported outcomes in heart failure with preserved vs. reduced ejection fraction: focus on physical independence. ESC Heart Fail 7(5):2051–2062. https://doi.org/10.1002/ehf2.12950
Joseph SM, Novak E, Arnold SV et al (2013) Comparable performance of the Kansas City Cardiomyopathy Questionnaire in patients with heart failure with preserved and reduced ejection fraction. Circ Heart Fail 6(6):1139–1146. https://doi.org/10.1161/circheartfailure.113.000359
Spertus JA, Jones PG, Sandhu AT, Arnold SV (2020) Interpreting the Kansas City Cardiomyopathy Questionnaire in clinical trials and clinical care: JACC state-of-the-art review. J Am Coll Cardiol 76(20):2379–2390. https://doi.org/10.1016/j.jacc.2020.09.542
Lewis EF, Kim HY, Claggett B et al (2016) Impact of spironolactone on longitudinal changes in health-related quality of life in the treatment of preserved cardiac function heart failure with an aldosterone antagonist trial. Circ Heart Fail 9(3):e001937. https://doi.org/10.1161/circheartfailure.114.001937
Streng KW, Nauta JF, Hillege HL et al (2018) Non-cardiac comorbidities in heart failure with reduced, mid-range and preserved ejection fraction. Int J Cardiol 271:132–139. https://doi.org/10.1016/j.ijcard.2018.04.001
Lam CSP, Wood R, Vaduganathan M et al (2021) Contemporary economic burden in a real-world heart failure population with Commercial and Medicare supplemental plans. Clin Cardiol 44(5):646–655. https://doi.org/10.1002/clc.23585
Kiuchi S, Hisatake S, Kabuki T, Oka T, Dobashi S, Fujii T, Ikeda T (2020) Comparable effect of tolvaptan in heart failure patients with preserved or reduced ejection fraction. Clin Exp Hypertens 42(2):110–117. https://doi.org/10.1080/10641963.2019.1583244
Center for Drug Evaluation and Research (2015) Approval package for application number 207620Orig1s018. Trade name: Entresto. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2015/207620Orig1s000Approv.pdf. Accessed 7 Nov 2023
Stewart J (2021) Entresto FDA approval history 2023. https://www.drugs.com/history/entresto.html. Accessed 7 Nov 2023
European Medicines Agency (2023) Entresto Summary of Product Characteristics. 7 Nov 2023. https://www.ema.europa.eu/en/documents/product-information/entresto-epar-product-information_en.pdf.
US Food and Drug Administration (2023) Drugs@FDA: FDA-Approved Drugs. https://www.accessdata.fda.gov/scripts/cder/daf/index.cfm. Accessed 7 Nov 2023
Boehringer Ingelheim (2022) Jardiance® (empagliflozin) becomes the first and only approved treatment in Europe for adults with symptomatic chronic heart failure regardless of ejection fraction (Press Release). https://www.boehringer-ingelheim.com/human-health/heart-diseases/heart-failure/preserved-heart-failure-treatment-approval-europe. Accessed 7 Nov 2023
Eckford C (European Pharmaceutical Review) (2022) Dapagliflozin approved for heart failure across LVEFs. https://www.europeanpharmaceuticalreview.com/news/177359/dapagliflozin-approved-for-heart-failure-across-lvefs/. Accessed 7 Nov 2023
Gallagher A (2023) FDA approves expanded label for dapagliflozin to reduce risk of cardiovascular death, hospitalization from heart failure. PharmacyTimes. https://www.pharmacytimes.com/view/fda-approves-expanded-label-for-dapagliflozin-to-reduce-risk-of-cardiovascular-death-hospitalization-from-heart-failure. Accessed 7 Nov 2023
Pharmaceuticals and Medical Devices Agency (2020) New Drugs Approved in FY 2020. 7 Nov 2023. https://www.pmda.go.jp/files/000242574.pdf
Pharmaceutical and Medical Devices Agency (2021) New Drugs Approved in FY 2021. 7 Nov 2023. https://www.pmda.go.jp/files/000250462.pdf
Wohlfahrt P, Nativi-Nicolau J, Zhang M et al (2021) Quality of life in patients with heart failure with recovered ejection fraction. JAMA Cardiol 6(8):957–962. https://doi.org/10.1001/jamacardio.2021.0939
Borlaug BA, Sharma K, Shah SJ, Ho JE (2023) Heart Failure with preserved ejection fraction: JACC scientific statement. J Am Coll Cardiol 81(18):1810–1834. https://doi.org/10.1016/j.jacc.2023.01.049
Savarese G, Becher PM, Lund LH, Seferovic P, Rosano GMC, Coats AJS (2023) Global burden of heart failure: a comprehensive and updated review of epidemiology. Cardiovasc Res 118(17):3272–3287. https://doi.org/10.1093/cvr/cvac013
Dunlay SM, Roger VL, Weston SA, Jiang R, Redfield MM (2012) Longitudinal changes in ejection fraction in heart failure patients with preserved and reduced ejection fraction. Circ Heart Fail 5(6):720–726. https://doi.org/10.1161/circheartfailure.111.966366
Cintron G, Johnson G, Francis G, Cobb F, Cohn JN (1993) Prognostic significance of serial changes in left ventricular ejection fraction in patients with congestive heart failure. The V-HeFT VA Cooperative Studies Group. Circulation 87(6 Suppl):Vi17–23
Basuray A, French B, Ky B et al (2014) Heart failure with recovered ejection fraction: clinical description, biomarkers, and outcomes. Circulation 129(23):2380–2387. https://doi.org/10.1161/circulationaha.113.006855
Kalogeropoulos AP, Fonarow GC, Georgiopoulou V et al (2016) Characteristics and outcomes of adult outpatients with heart failure and improved or recovered ejection fraction. JAMA Cardiol 1(5):510–518. https://doi.org/10.1001/jamacardio.2016.1325
Chamberlain AM, Boyd CM, Manemann SM et al (2020) Risk factors for heart failure in the community: Differences by age and ejection fraction. Am J Med 133(6):e237–e248. https://doi.org/10.1016/j.amjmed.2019.10.030
Chamberlain AM, St Sauver JL, Gerber Y et al (2015) Multimorbidity in heart failure: a community perspective. Am J Med 128(1):38–45. https://doi.org/10.1016/j.amjmed.2014.08.024
Murtaza G, Paul TK, Rahman ZU, Kelvas D, Lavine SJ (2020) Clinical characteristics, comorbidities and prognosis in patients with heart failure with mid-range ejection fraction. Am J Med Sci 359(6):325–333. https://doi.org/10.1016/j.amjms.2020.03.008
European Medicines Agency (2022) EMA/954956/2022 – Forxiga European Public Assessment Report, 2022, https://www.ema.europa.eu/en/documents/variation-report/forxiga-h-c-ws-2299-epar-assessment-report-variation_en.pdf. Accessed 7 Nov 2023.
Center for Drug Evaluation and Research (2015) Approval package for application number 204629Orig1s001. Trade name: Jardiance. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2021/204629Orig1s001.pdf. Accessed 7 Nov 2023
European Medicines Agency (2022) CHMP extension of indication variation assessment report: Jardiance. 7 Nov 2023. https://www.ema.europa.eu/en/documents/variation-report/jardiance-h-c-002677-ii-0060-epar-assessment-report-variation_en.pdf
JCS/JHFS (2023) Recommendations for the appropriate use of SGLT2 inhibitors in the treatment of heart failure. https://www.j-circ.or.jp/cms/wp-content/uploads/2023/06/jcs_jhfs_Recommendation_SGLT2_Inhibitors__HF.pdf. Accessed 7 Nov 2023
McDonagh TA, Metra M, Adamo M et al (2023) 2023 Focused Update of the 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: Developed by the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) With the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J:ehad195. 7 Nov 2023. https://doi.org/10.1093/eurheartj/ehad195
ClinicalTrials.gov (2023) A study of tirzepatide (LY3298176) in participants with heart failure with preserved ejection fraction and obesity (SUMMIT) (ClinicalTrials.gov ID: NCT04847557). https://clinicaltrials.gov/ct2/show/NCT04847557. Accessed 7 Nov 2023
ClinicalTrials.gov (2023) Research study to look at how well semaglutide works in people living with heart failure, obesity and type 2 diabetes (STEP HFpEF DM) (ClinicalTrials.gov ID: NCT04916470). https://clinicaltrials.gov/ct2/show/NCT04916470. Accessed 7 Nov 2023
ClinicalTrials.gov (2023) A research study to look at how ziltivekimab works compared to placebo in people with heart failure and inflammation (HERMES) (ClinicalTrials.gov ID: NCT05636176). https://clinicaltrials.gov/ct2/show/NCT05636176. Accessed 7 Nov 2023
ClinicalTrials.gov (2023) Study to evaluate the efficacy and safety of AZD4831 in participants with heart failure with left ventricular ejection fraction > 40% (ENDEAVOR) (ClinicalTrials.gov ID: NCT04986202). https://clinicaltrials.gov/ct2/show/NCT04986202. Accessed 7 Nov 2023
Hashemi H, Mechanick J (2021) The Pooled SCORED and SOLOIST-WHF Analysis. https://accessmedicine.mhmedical.com/updatesContent.aspx?gbosid=556865. Accessed 7 Nov 2023
Edelmann F, Wachter R, Schmidt AG et al (2013) Effect of spironolactone on diastolic function and exercise capacity in patients with heart failure with preserved ejection fraction: the Aldo-DHF randomized controlled trial. JAMA 309(8):781–791. https://doi.org/10.1001/jama.2013.905
Ueda T, Kasama S, Yamamoto M et al (2021) Effect of the sodium-glucose cotransporter 2 inhibitor canagliflozin for heart failure with preserved ejection fraction in patients with type 2 diabetes. Circ Rep 3(8):440–448. https://doi.org/10.1253/circrep.CR-21-0030
ClinicalTrials.gov (2021) DETERMINE-preserved-dapagliflozin effect on exercise capacity using a 6-minute walk test in patients with heart failure with preserved ejection fraction. https://classic.clinicaltrials.gov/ct2/show/NCT03877224. Accessed 7 Nov 2023
Massie BM, Carson PE, McMurray JJ et al (2008) Irbesartan in patients with heart failure and preserved ejection fraction. N Engl J Med 359(23):2456–2467. https://doi.org/10.1056/NEJMoa0805450
Kosmala W, Rojek A, Przewlocka-Kosmala M, Wright L, Mysiak A, Marwick TH (2016) Effect of aldosterone antagonism on exercise tolerance in heart failure with preserved ejection fraction. J Am Coll Cardiol 68(17):1823–1834. https://doi.org/10.1016/j.jacc.2016.07.763
Upadhya B, Hundley WG, Brubaker PH, Morgan TM, Stewart KP, Kitzman DW (2017) Effect of spironolactone on exercise tolerance and arterial function in older adults with heart failure with preserved ejection fraction. J Am Geriatr Soc 65(11):2374–2382. https://doi.org/10.1111/jgs.14940
Yip GW, Wang M, Wang T et al (2008) The Hong Kong diastolic heart failure study: a randomised controlled trial of diuretics, irbesartan and ramipril on quality of life, exercise capacity, left ventricular global and regional function in heart failure with a normal ejection fraction. Heart 94(5):573–580. https://doi.org/10.1136/hrt.2007.117978
Yuksek U, Cerit L, Eren NK, Ergene O (2019) The effect of perindopril on echocardiographic parameters, NYHA functional class and serum NT-proBNP values in patients with diastolic heart failure. Cardiovasc J Afr 30(4):222–227. https://doi.org/10.5830/cvja-2019-022
Zi M, Carmichael N, Lye M (2003) The effect of quinapril on functional status of elderly patients with diastolic heart failure. Cardiovasc Drugs Ther 17(2):133–139. https://doi.org/10.1023/a:1025387702212
Davis BR, Kostis JB, Simpson LM et al (2008) Heart failure with preserved and reduced left ventricular ejection fraction in the antihypertensive and lipid-lowering treatment to prevent heart attack trial. Circulation 118(22):2259–2267. https://doi.org/10.1161/circulationaha.107.762229
Tanaka A, Hisauchi I, Taguchi I et al (2020) Effects of canagliflozin in patients with type 2 diabetes and chronic heart failure: a randomized trial (CANDLE). ESC Heart Fail 7(4):1585–1594. https://doi.org/10.1002/ehf2.12707
Spertus JA, Birmingham MC, Nassif M et al (2022) The SGLT2 inhibitor canagliflozin in heart failure: the CHIEF-HF remote, patient-centered randomized trial. Nat Med 28(4):809–813. https://doi.org/10.1038/s41591-022-01703-8
Tamisier R, Damy T, Davy JM et al (2020) Cohort profile: FACE, prospective follow-up of chronic heart failure patients with sleep-disordered breathing indicated for adaptive servo ventilation. BMJ Open 10(7):e038403. https://doi.org/10.1136/bmjopen-2020-038403
Hawley A, He J, Crabtree A, Iacovides S, Keeling P (2020) The impact of an integrated heart failure service in a medium-sized district general hospital. Open Heart 7(1). https://doi.org/10.1136/openhrt-2019-001218
Verdu-Rotellar JM, Vaillant-Roussel H, Abellana R et al (2020) Precipitating factors of heart failure decompensation, short-term morbidity and mortality in patients attended in primary care. Scand J Prim Health Care 38(4):473–480. https://doi.org/10.1080/02813432.2020.1844387
Arora S, Jaswaney R, Jani C et al (2020) Catheter ablation for atrial fibrillation in patients with concurrent heart failure. Am J Cardiol 137:45–54. https://doi.org/10.1016/j.amjcard.2020.09.035
Buckallew AR, Tellor KB, Watson R et al (2021) Evaluation of the safety and tolerability of spironolactone in patients with heart failure and chronic kidney disease. Eur J Clin Pharmacol 77(7):955–960. https://doi.org/10.1007/s00228-020-03069-7
Contreras JP, Hong KN, Castillo J et al (2019) Anticoagulation in patients with atrial fibrillation and heart failure: Insights from the NCDR PINNACLE-AF registry. Clin Cardiol 42(3):339–345. https://doi.org/10.1002/clc.23142
Dunlay SM, Roger VL, Killian JM et al (2021) Advanced heart failure epidemiology and outcomes: A population-based study. JACC Heart Fail 9(10):722–732. https://doi.org/10.1016/j.jchf.2021.05.009
Hamo CE, Fonarow GC, Greene SJ et al (2021) Temporal trends in risk profiles among patients hospitalized for heart failure. Am Heart J 232:154–163. https://doi.org/10.1016/j.ahj.2020.11.015
Joyce E, Chung C, Badloe S et al (2016) Variable contribution of heart failure to quality of life in ambulatory heart failure with reduced, better, or preserved ejection fraction. JACC Heart Fail 4(3):184–193. https://doi.org/10.1016/j.jchf.2015.12.011
Lopuszynski JB, Downing AJ, Finley CM, Zahid M (2021) Prognosticators of All-cause mortality in patients with heart failure with preserved ejection fraction. Am J Cardiol 158:66–73. https://doi.org/10.1016/j.amjcard.2021.07.044
Luo N, Xu H, Jneid H et al (2018) Use of oral anticoagulation in eligible patients discharged with heart failure and atrial fibrillation. Circ Heart Fail 11(10):e005356. https://doi.org/10.1161/circheartfailure.118.005356
Navid P, Nguyen L, Jaber D et al (2021) Attitudes toward deprescribing among adults with heart failure with preserved ejection fraction. J Am Geriatr Soc 69(7):1948–1955. https://doi.org/10.1111/jgs.17204
Patel RB, Fonarow GC, Greene SJ et al (2021) Kidney function and outcomes in patients hospitalized with heart failure. J Am Coll Cardiol 78(4):330–343. https://doi.org/10.1016/j.jacc.2021.05.002
Regmi MR, Bhattarai M, Parajuli P et al (2020) Heart failure with preserved ejection fraction and 30-day readmission. Clin Med Res 18(4):126–132. https://doi.org/10.3121/cmr.2020.1521
Yee D, Novak E, Platts A, Nassif ME, LaRue SJ, Vader JM (2019) Comparison of the Kansas City Cardiomyopathy Questionnaire and Minnesota Living With Heart Failure Questionnaire in predicting heart failure outcomes. Am J Cardiol 123(5):807–812. https://doi.org/10.1016/j.amjcard.2018.11.037
Kinugawa K, Sato N, Inomata T, Yasuda M, Shimakawa T, Fukuta Y (2019) A prospective, multicenter, post-marketing surveillance study to evaluate the safety and effectiveness of tolvaptan in patients with reduced, preserved, and mid-range ejection fraction heart failure. Int Heart J 60(5):1123–1130. https://doi.org/10.1536/ihj.18-671
Suzuki S, Motoki H, Minamisawa M et al (2019) Prognostic significance of high-sensitivity cardiac troponin in patients with heart failure with preserved ejection fraction. Heart Vessels 34(10):1650–1656. https://doi.org/10.1007/s00380-019-01393-2
Tomii D, Horiuchi Y, Gonda Y et al (2021) The role of the renal resistance index in patients with heart failure with reduced or preserved ejection fraction. J Cardiol 78(4):301–307. https://doi.org/10.1016/j.jjcc.2021.05.007
Chandramouli C, Tay WT, Bamadhaj NS et al (2019) Association of obesity with heart failure outcomes in 11 Asian regions: A cohort study. PLoS Med 16(9):e1002916. https://doi.org/10.1371/journal.pmed.1002916
Kapelios CJ, Laroche C, Crespo-Leiro MG et al (2020) Association between loop diuretic dose changes and outcomes in chronic heart failure: observations from the ESC-EORP Heart Failure Long-Term Registry. Eur J Heart Fail 22(8):1424–1437. https://doi.org/10.1002/ejhf.1796
Acknowledgements
Medical writing was provided by Mohammed Alshaikheid from Putnam and editing support was provided by Lucy Moffitt from Putnam.
Funding
The study was funded by Bayer AG.
Author information
Authors and Affiliations
Contributions
All named authors have reviewed and approved the final version of the manuscript. All authors contributed to the design and the writing of the manuscript.
Corresponding author
Ethics declarations
Ethical approval
Not applicable.
Competing interests
Nihar Desai works under contract with the Centers for Medicare and Medicaid Services to develop and maintain performance measures used for public reporting and pay for performance programs. He reports research grants and consulting for Amgen, Astra Zeneca, Bayer, Boehringer Ingelheim, Bristol Myers Squibb, CSL Behring, Cytokinetics, Merck, Novartis, SCPharmaceuticals, and Vifor. Elzbieta Olewinska, Agata Famulska, Cécile Remuzat and Clément Francois are employees of Putnam which received funding from Bayer AG to conduct the study. Kerstin Folkerts is employee of Bayer AG.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Desai, N., Olewinska, E., Famulska, A. et al. Heart failure with mildly reduced and preserved ejection fraction: A review of disease burden and remaining unmet medical needs within a new treatment landscape. Heart Fail Rev 29, 631–662 (2024). https://doi.org/10.1007/s10741-024-10385-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10741-024-10385-y