Abstract
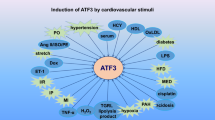
Cardiovascular disease (CVD) is the leading cause of death worldwide and encompasses diverse diseases of the vasculature, myocardium, cardiac electrical circuit, and cardiac development. Forkhead box protein P1 (Foxp1) is a large multi-domain transcriptional regulator belonging to the Fox family with winged helix DNA-binding protein, which plays critical roles in cardiovascular homeostasis and disorders. The broad distribution of Foxp1 and alternative splicing isoforms implicate its distinct functions in diverse cardiac and vascular cells and tissue types. Foxp1 is essential for diverse biological processes and has been shown to regulate cellular proliferation, apoptosis, oxidative stress, fibrosis, angiogenesis, cardiovascular remodeling, and dysfunction. Notably, both loss-of-function and gain-of-function approaches have defined critical roles of Foxp1 in CVD. Genetic deletion of Foxp1 results in pathological cardiac remodeling, exacerbation of atherosclerotic lesion formation, prolonged occlusive thrombus formation, severe cardiac defects, and embryo death. In contrast, activation of Foxp1 performs a wide range of physiological effects, including cell growth, hypertrophy, differentiation, angiogenesis, and cardiac development. More importantly, Foxp1 exerts anti-inflammatory and anti-atherosclerotic effects in controlling coronary thrombus formation and myocardial infarction (MI). Thus, targeting for Foxp1 signaling has emerged as a pre-warning biomarker and a novel therapeutic approach against progression of CVD, and an increased understanding of cardiovascular actions of the Foxp1 signaling will help to develop effective interventions. In this review, we focus on the diverse actions and underlying mechanisms of Foxp1 highlighting its roles in CVD, including heart failure, MI, atherosclerosis, congenital heart defects, and atrial fibrillation.


Similar content being viewed by others
References
Wang J, Wei L, Yang X, Zhong JC (2019) Roles of growth differentiation factor 15 in atherosclerosis and coronary artery disease. J Am Heart Assoc 8:e012826
Patel VB, Zhong JC, Grant MB, Oudit GY (2016) Role of the ACE2/angiotensin 1–7 axis of the renin–angiotensin system in heart failure. Circ Res 118(8):1313–1326
Farzadfar F (2019) Cardiovascular disease risk prediction models: challenges and perspectives. Lancet Glob Health 7(10):e1288–e1289
Katoh M, Igarashi M, Fukuda H, Nakagama H, Katoh M (2013) Cancer genetics and genomics of human FOX family genes. Cancer Lett 328(2):198–206
Shu W, Yang H, Zhang L, Lu M, Morrisey E (2001) Characterization of a new subfamily of winged-helix/forkhead (fox) genes that are expressed in the lung and act as transcriptional repressors. J Biol Chem 276(29):27488–27497
Wang B, Lin D, Li C, Tucker P (2003) Multiple domains define the expression and regulatory properties of Foxp1 forkhead transcriptional repressors. J Biol Chem 278(27):24259–24268
Laissue P (2019) The forkhead-box family of transcription factors: key molecular players in colorectal cancer pathogenesis. Mol Cancer 18(1):5
Santos ME, Athanasiadis A, Leitão AB, DuPasquier L, Sucena E (2011) Alternative splicing and gene duplication in the evolution of the FoxP gene subfamily. Mol Biol Evol 28(1):237–247
Hannenhalli S, Putt ME, Gilmore JM, Wang J, Parmacek MS, Epstein JA et al (2006) Transcriptional genomics associates FOX transcription factors with human heart failure. Circulation 11(12):1269–1276
Kim JH, Hwang J, Jung JH, Lee HJ, Lee DY, Kim SH (2019) Molecular networks of FOXP family: dual biologic functions, interplay with other molecules and clinical implications in cancer progression. Mol Cancer 18(1):180
Zhang SP, Yang RH, Shang J, Gao T, Wang R, Peng XD, Miao X, Pan L, Yuan WJ, Lin L, Hu QK (2019) FOXC1 up-regulates the expression of toll-like receptors in myocardial ischaemia. J Cell Mol Med 23(11):7566–7580
Wang C, Xu W, Zhang Y, Zhang F, Huang K (2018) PARP1 promote autophagy in cardiomyocytes via modulating FoxO3a transcription. Cell Death Dis 9(11):1047
Evans-Anderson HJ, Alfieri CM, Yutzey KE (2008) Regulation of cardiomyocyte proliferation and myocardial growth during development by FOXO transcription factors. Circ Res 102(6):686–694
Li S, Weidenfeld J, Morrisey EE (2004) Transcriptional and DNA binding activity of the Foxp1/2/4 family is modulated by heterotypic and homotypic protein interactions. Mol Cell Biol 24(2):809–822
Yang Y, Del Re DP, Nakano N, Sciarretta S, Zhai P, Park J et al (2015) miR-206 mediates YAP induced cardiac hypertrophy and survival. Circ Res 117(10):891–904
Wang B (2004) Foxp1 regulates cardiac outflow tract, endocardial cushion morphogenesis and myocyte proliferation and maturation. Development 131(18):4477–4487
Zhang Y, Li S, Yuan L, Tian Y, Weidenfeld J, Yang J, Liu F, Chokas AL, Morrisey EE (2010) Foxp1 coordinates cardiomyocyte proliferation through both cell-autonomous and nonautonomous mechanisms. Genes Dev 24(16):1746–1757
Xing T, Du L, Zhuang X, Zhang L, Hao J, Wang J (2017) Upregulation of microRNA-206 induces apoptosis of vascular smooth muscle cells and decreases risk of atherosclerosis through modulating FOXP1. Exp Ther Med 14(5):4097–4103
Liu J, Zhuang T, Pi J, Chen X, Zhang Q, Li Y, Wang H, Shen Y, Tomlinson B, Chan P, Yu Z, Cheng Y, Zheng X, Reilly M, Morrisey E, Zhang L, Liu Z, Zhang Y (2019) Endothelial Foxp1 regulates pathological cardiac remodeling through TGF-β1-endothelin-1 signal pathway. Circulation 140(8):665–680
Bai S, Kerppola TK (2011) Opposing roles of FoxP1 and Nfat3 in transcriptional control of cardiomyocyte hypertrophy. Mol Cell Biol 31(14):3068–3080
Grundmann S, Lindmayer C, Hans FP, Hoefer I, Helbing T, Pasterkamp G (2013) FoxP1 stimulates angiogenesis by repressing the inhibitory guidance protein semaphorin 5B in endothelial cells. PLoS One 8(9):e70873
Zhuang T, Liu J, Chen X, Zhang L, Pi J, Sun H, Li L, Bauer R, Wang H, Yu Z, Zhang Q, Tomlinson B, Chan P, Zheng X, Morrisey E, Liu Z, Reilly M, Zhang Y (2019) Endothelial Foxp1 suppresses atherosclerosis via modulation of Nlrp3 inflammasome activation. Circ Res 125(6):590–605
Wang Y, Gao H, Shi C, Erhardt PW, Pavlovsky A, Soloviev DA, Bledzka K, Ustinov V, Zhu L, Qin J, Munday AD, Lopez J, Plow E, Simon DI (2017) Leukocyte integrin Mac-1 regulates thrombosis via interaction with platelet GPIbα. Nat Commun 8:16124
Co M, Anderson AG, Konopka G (2020) FOXP transcription factors in vertebrate brain development, function, and disorders. Wiley Interdiscip Rev Dev Biol 30:e375
Shu W, Lu MM, Zhang Y, Tucker PW, Zhou D, Morrisey EE (2007) Foxp2 and Foxp1 cooperatively regulate lung and esophagus development. Development 134(10):1991–2000
Jepsen K, Gleiberman AS, Shi C, Simon DI, Rosenfeld MG (2008) Cooperative regulation in development by SMRT and FOXP1. Genes Dev 22(6):740–745
Bot PT, Grundmann S, Goumans MJ, de Kleijn D, Moll F, de Boer O, van der Wal AC, van Soest A, de Vries JP, van Royen N, Piek JJ, Pasterkamp G, Hoefer IE (2011) Forkhead box protein P1 as a downstream target of transforming growth factor-β induces collagen synthesis and correlates with a more stable plaque phenotype. Atherosclerosis 218(1):33–43
Cerna K, Mraz M (2018) p53 limits B cell receptor (BCR) signalling: a new role for miR-34a and FOXP1. Oncotarget 9(92):36409–36410
Gadage V, Kembhavi S, Kumar P, Shet T (2011) Primary cardiac diffuse large B-cell lymphoma with activated B-cell-like phenotype. Indian J Pathol Microbiol 54(3):591–593
Patzelt T, Keppler SJ, Gorka O, Thoene S, Wartewig T, Reth M, Förster I, Lang R, Buchner M, Ruland J (2018) Foxp1 controls mature B cell survival and the development of follicular and B-1 B cells. Proc Natl Acad Sci U S A 115(12):3120–3125
Konopacki C, Pritykin Y, Rubtsov Y, Leslie CS, Rudensky AY (2019) Transcription factor Foxp1 regulates Foxp3 chromatin binding and coordinates regulatory T cell function. Nat Immunol 20(2):232–242
Stephen TL, Rutkowski MR, Allegrezza MJ, Perales-Puchalt A, Tesone AJ, Svoronos N, Nguyen JM, Sarmin F, Borowsky ME, Tchou J, Conejo-Garcia JR (2014) Transforming growth factor β-mediated suppression of antitumor T cells requires FoxP1 transcription factor expression. Immunity 41(3):427–439
Shi C, Sakuma M, Mooroka T, Liscoe A, Gao H, Croce KJ, Sharma A, Kaplan D, Greaves DR, Wang Y, Simon DI (2008) Down-regulation of the forkhead transcription factor Foxp1 is required for monocyte differentiation and macrophage function. Blood 112(12):4699–4711
Shi C, Zhang X, Chen Z, Sulaiman K, Feinberg MW, Ballantyne CM, Jain MK, Simon DI (2004) Integrin engagement regulates monocyte differentiation through the forkhead transcription factor Foxp1. J Clin Invest 114(3):408–418
Zou Y, Gong N, Cui Y, Wang X, Cui A, Chen Q, Jiao T, Dong X, Yang H, Zhang S, Fang F, Chang Y (2015) Forkhead box P1 (FOXP1) transcription factor regulates hepatic glucose homeostasis. J Biol Chem 290(51):30607–30615
Xiang H, Xue W, Wu X, Zheng J, Ding C, Li Y, Dou M (2019) FOXP1 inhibits high glucose-induced ECM accumulation and oxidative stress in mesangial cells. Chem Biol Interact 313:108818
Zhang XL, Zhu HQ, Zhang Y, Zhang CY, Jiao JS, Xing XY (2020) LncRNA CASC2 regulates high glucose-induced proliferation, extracellular matrix accumulation and oxidative stress of human mesangial cells via miR-133b FOXP1 axis. Eur Rev Med Pharmacol Sci 24(2):802–812
Ya J, Schilham MW, de Boer PA, Moorman AF, Clevers H, Lamers WH (1998) Sox4-deficiency syndrome in mice is an animal model for common trunk. Circ Res 83(10):986–994
Kumai M, Nishii K, Nakamura K, Takeda N, Suzuki M, Shibata Y (2000) Loss of connexin45 causes a cushion defect in early cardiogenesis. Development 127(16):3501–3512
Wang Y, Morrisey EE (2010) Regulation of cardiomyocyte proliferation by Foxp1. Cell Cycle 9(21):4251–4252
Günthel M, Phil B, Christoffels VM (2018) Development, proliferation, and growth of the mammalian heart. Mol Ther 26(7):1599–1609
Ponnusamy M, Li PF, Wang K (2017) Understanding cardiomyocyte proliferation: an insight into cell cycle activity. Cell Mol Life Sci 74(6):1019–1034
Chang SW, Mislankar M, Misra C, Huang N, Dajusta DG, Harrison SM et al (2013) Genetic abnormalities in FOXP1 are associated with congenital heart defects. Hum Mutat 34(9):1226–1230
Prall OW, Menon MK, Solloway MJ, Watanabe Y, Zaffran S, Bajolle F et al (2007) An Nkx2.5/Bmp2/Smad1 negative feedback loop controls heart progenitor specification and proliferation. Cell 128(5):947–959
Chamorro MN, Schwartz DR, Vonica A, Brivanlou AH, Cho KR, Varmus HE (2005) FGF-20 and DKK1 are transcriptional targets of beta-catenin and FGF-20 is implicated in cancer and development. EMBO J 24(1):73–84
He Q, Zhao L, Liu Y, Liu X, Zheng J, Yu H, Cai H, Ma J, Liu L, Wang P, Li Z, Xue Y (2018) Circ-SHKBP1 regulates the angiogenesis of U87 glioma-exposed endothelial cells through miR-544a/FOXP1 and miR-379/FOXP2 pathways. Mol Ther Nucleic Acids 10:331–348
Lähteenvuo JE, Lähteenvuo MT, Kivelä A, Rosenlew C, Falkevall A, Klar J et al (2009) Vascular endothelial growth factor-β induces myocardium-specific angiogenesis and arteriogenesis via vascular endothelial growth factor receptor-1- and neuropilin receptor-1-dependent mechanisms. Circulation 119(6):845–856
De Windt LJ, Lim HW, Taigen T, Wencker D, Condorelli G, Dorn GW 2nd et al (2000) Calcineurin-mediated hypertrophy protects cardiomyocytes from apoptosis in vitro and in vivo: an apoptosis-independent model of dilated heart failure. Circ Res 86(3):255–263
Passier R, Zeng H, Frey N, Naya FJ, Nicol RL, McKinsey TA et al (2000) CaM kinase signaling induces cardiac hypertrophy and activates the MEF2 transcription factor in vivo. J Clin Invest 105(10):1395–1406
Li X, Chu G, Zhu F, Zheng Z, Wang X, Zhang G, Wang F (2020) Epoxyeicosatrienoic acid prevents maladaptive remodeling in pressure overload by targeting calcineurin/NFAT and Smad-7. Exp Cell Res 386(1):111716
Ikeda S, Sadoshima J (2016) Regulation of myocardial cell growth and death by the Hippo pathway. Circ J 80(7):1511–1519
Shao D, Zhai P, Del Re DP, Sciarretta S, Yabuta N, Nojima H et al (2014) A functional interaction between Hippo-YAP signalling and FoxO1 mediates the oxidative stress response. Nat Commun 5:3315
Eisinger TS, Mucaj V, Biju KM, Nakazawa MS, Gohil M, Cash TP et al (2015) Deregulation of the Hippo pathway in soft-tissue sarcoma promotes FOXM1 expression and tumorigenesis. Proc Natl Acad Sci U S A 112(26):E3402–E3411
Shimizu I, Minamino T (2016) Physiological and pathological cardiac hypertrophy. J Mol Cell Cardiol 97:245–262
Kamo T, Akazawa H, Komuro I (2015) Cardiac nonmyocytes in the hub of cardiac hypertrophy. Circ Res 117(1):89–98
Zhang S, Liu X, Ge LL, Li K, Sun Y, Wang F, Han Y, Sun C, Wang J, Jiang W, Xin Q, Xu C, Chen Y, chen O, Zhang Z, Luan Y (2020) Mesenchymal stromal cell-derived exosomes improve pulmonary hypertension through inhibition of pulmonary vascular remodeling. Respir Res 21(1):71
Jalali S, Ramanathan GK, Parthasarathy PT, Aljubran S, Galam L, Yunus A, Garcia S, Cox RR, Lockey RF, Kolliputi N (2012) Mir-206 regulates pulmonary artery smooth muscle cell proliferation and differentiation. PLoS One 7(10):e46808
Shi C, Miley J, Nottingham A, Morooka T, Prosdocimo DA, Simon DI (2019) Leukocyte integrin signaling regulates FOXP1 gene expression. Biochim Biophys Acta Gene Regul Mech 1862(4):493–508
Shi C, Simon DI (2006) Integrin signals, transcription factors, and monocyte differentiation. Trends Cardiovasc Med 16(5):146–152
Simon DI (2012) Inflammation and vascular injury: basic discovery to drug development. Circ J 76(8):1811–1818
Koupenova M, Clancy L, Corkrey HA, Freedman JE (2018) Circulating platelets as mediators of immunity, inflammation, and thrombosis. Circ Res 122(2):337–351
Sansbury BE, Spite M (2016) Resolution of acute inflammation and the role of Resolvins in immunity, thrombosis, and vascular biology. Circ Res 119(1):113–130
Pierpont M, Basson C, Benson D, Gelb B, Giglia T, Goldmuntz E (2007) Genetic basis for congenital heart defects: current knowledge. Pediatrics 120(2):447
Kathiresan S, Srivastava D (2012) Genetics of human cardiovascular disease. Cell 148(6):1242–1257
Gambetta K, Al-Ahdab MK, Ilbawi MN, Hassaniya N, Gupta M (2008) Transcription repression and blocks in cell cycle progression in hypoplastic left heart syndrome. Am J Physiol Heart Circ Physiol 294(5):H2268–H2275
Linglart L, Gelb BD (2020) Congenital heart defects in Noonan syndrome: diagnosis, management, and treatment. Am J Med Genet C Semin Med Genet 184(1):73–80
Lauriol J, Cabrera JR, Roy A, Keith K, Hough SM, Damilano F, Wang B, Segarra GC, Flessa ME, Miller LE, Das S, Bronson R, Lee KH, Kontaridis MI (2016) Developmental SHP2 dysfunction underlies cardiac hypertrophy in Noonan syndrome with multiple lentigines. J Clin Invest 126(8):2989–3005
Williams JW, Huang LH, Randolph GJ (2019) Cytokine circuits in cardiovascular disease. Immunity 50(4):941–954
Mangge H, Almer G (2019) Immune-mediated inflammation in vulnerable atherosclerotic plaques. Molecules 24(17):E3072
Moore KJ, Sheedy FJ, Fisher EA (2013) Macrophages in atherosclerosis: a dynamic balance. Nat Rev Immunol 13(10):709–721
Lavine KJ, Pinto AR, Epelman S, Kopecky BJ, Clemente-Casares X, Godwin J, Rosenthal N, Kovacic JC (2018) The macrophage in cardiac homeostasis and disease JACC macrophage in CVD series. J Am Coll Cardiol 72(18):2213–2230
An N, Gao Y, Si Z, Zhang H, Wang L, Tian C, Yuan M, Yang X, Li X, Shang H, Xiong X, Xing Y (2019) Regulatory mechanisms of the NLRP3 inflammasome, a novel immune-inflammatory marker in cardiovascular. Front Immunol 10:1592
Castillo-Díaz SA, Garay-Sevilla ME, Hernández-González MA, Solís-Martínez MO, Zaina S (2010) Extensive demethylation of normally hypermethylated CpG islands occurs in human atherosclerotic arteries. Int J Mol Med 26(5):691–700
Falk E, Nakano M, Bentzon JF, Finn AV, Virmani R (2013) Update on acute coronary syndromes: the pathologists' view. Eur Heart J 34(10):719–728
Jackson CL, Bennett MR, Biessen EA, Johnson JL, Krams R (2007) Assessment of unstable atherosclerosis in mice. Arterioscler Thromb Vasc Biol 27(4):714–720
Yang M, Song JJ, Liu XY, Zhao L, Wang J, Zuo K et al (2020) Inhibition of miRNA-122-5p counterregulates against angiotensin II-mediated loss of autophagy and promotion of apoptosis in rat cardiofibroblasts by modulation of the APLN-AMPK-mTOR signaling. Artif Cells Nanomed Biotechnol 49(1):LABB-2019–LABB-2082
Ma Z, Song JJ, Martin S, Yang XC, Zhong JC (2020) The Elabela-APJ axis: a promising therapeutic target for heart failure. Heart Fail Rev 26:1–10. https://doi.org/10.1007/s10741-020-09957-5
Gheblawi M, Wang K, Viveiros A, Nguyen O, Zhong J, Turner AJ et al (2020) Angiotensin converting enzyme 2: SARS-CoV-2 receptor and regulator of the renin-angiotensin system--celebrating the 20th anniversary of the discovery of ACE2. Circ Res 126:1457–1475
Nattel S (1999) Atrial electrophysiological remodeling caused by rapid atrial activation: underlying mechanisms and clinical relevance to atrial fibrillation. Cardiovasc Res 42(2):298–308
Laforest B, Dai W, Tyan L, Lazarevic S, Shen KM, Gadek M, Broman MT, Weber CR, Moskowitz IP (2019) Atrial fibrillation risk loci interact to modulate Ca2+-dependent atrial rhythm homeostasis. J Clin Invest 129(11):4937–4950
Mulla W, Hajaj B, Elyagon S, Mor M, Gillis R, Murninkas M, Klapper-Goldstein H, Plaschkes I, Chalifa-Caspi V, Etzion S, Etzion Y (2019) Rapid atrial pacing promotes atrial fibrillation substrate in unanesthetized instrumented rats. Front Physiol 10:1218
van Duijvenboden K, de Bakker DEM, Man JCK, Janssen R, Günthel M, Hill MC, Hooijkaas IB, van der Made I, van der Kraak PH, Vink A, Creemers EE, Martin JF, Barnett P, Bakkers J, Christoffels VM (2019) Conserved NPPB+ border zone switches from MEF2 to AP-1-driven gene program. Circulation 140(10):864–879
Panizzi P, Swirski FK, Figueiredo JL, Waterman P, Sosnovik DE, Aikawa E, Libby P, Pittet M, Weissleder R, Nahrendorf M (2010) Impaired infarct healing in atherosclerotic mice with Ly-6C(hi) monocytosis. J Am Coll Cardiol 55(15):1629–1638
Ridker PM, Libby P, MacFadyen JG, Thuren T, Ballantyne C, Fonseca F et al (2018) Modulation of the interleukin-6 signalling pathway and incidence rates of atherosclerotic events and all-cause mortality: analyses from the canakinumab anti-inflammatory thrombosis outcomes study (CANTOS). Eur Heart J 39(38):3499–3507
Zeglinski MR, Moghadam AR, Ande SR, Sheikholeslami K, Mokarram P, Sepehri Z et al (2018) Myocardial cell signaling during the transition to heart failure: cellular signaling and therapeutic approaches. Compr Physiol 9(1):75–125
Del Re DP, Amgalan D, Linkermann A, Liu Q, Kitsis RN (2019) Fundamental mechanisms of regulated cell death and implications for heart disease. Physiol Rev 99(4):1765–1817
Funding
This work was supported by the National Natural Science Foundation of China (81770253, 81370362), the National Major Research Plan Training Program (91849111), and talent project of Beijing Chaoyang Hospital Affiliated to Capital Medical University.
Author information
Authors and Affiliations
Contributions
Xin-Ming Liu: Writing original draft, making figures and tables, writing-reviewing and editing.
Sheng-Li Du, Ran Miao: Discussed the revision, writing original draft preparation, designed figures, and reviewed literatures.
Le-Feng Wang, Jiu-Chang Zhong: Conceptualization, writing original draft and revision, writing review and editing, making figures and tables.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declared that they have no conflict of interest.
Ethical standard
The manuscript does not contain clinical studies or patient data.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Liu, XM., Du, SL., Miao, R. et al. Targeting the forkhead box protein P1 pathway as a novel therapeutic approach for cardiovascular diseases. Heart Fail Rev 27, 345–355 (2022). https://doi.org/10.1007/s10741-020-09992-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10741-020-09992-2