Abstract
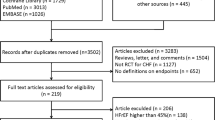
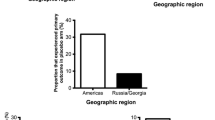
This study aims to assess the comparative benefit and risk profile of treatment with mineralocorticoid receptor antagonists (MRAs) with regard to all-cause mortality (primary endpoint), cardiovascular mortality, or heart failure (HF)–related hospitalization (secondary endpoints) and the safety endpoints hyperkalemia, acute renal failure, and gynecomastia in patients with chronic HF. We conducted a systematic review and network meta-analysis following PRISMA-P and PRISMA-NMA guidelines. From 16 different sources, 14 randomized controlled trials totaling 12,213 patients testing an active treatment of either spironolactone, eplerenone, or canrenone/potassium-canreonate in adults with symptomatic HF due to systolic dysfunction reporting any of the above endpoints were retained. Efficacy in comparison to placebo/standard medical care with respect to all-cause mortality was confirmed for spironolactone and eplerenone while no conclusion could be drawn for canrenone (HR 0.69 (0.62; 0.77), 0.82 (0.75; 0.91), and 0.50 (0.17; 1.45), respectively). Indirect comparisons hint a potential (non-significant) preference of spironolactone over eplerenone (HR 0.84 (0.68; 1.03)). The overall risk of bias was low to intermediate. Results for secondary endpoints as well as sensitivity analyses essentially mirrored these findings. The beta-blocker adjusted meta-analysis for the primary endpoint showed the same tendency as the unadjusted one (HR 0.39 (0.07; 2.03)). Results need to be interpreted with caution, though, as the resultant mix of patient- and study-level covariates produced unstable statistical modeling. We found no significant and systematic superiority of either MRA regarding efficacy toward all endpoints considered in both direct and indirect comparisons.






Similar content being viewed by others
References
Hunt SA, Abraham WT, Chin MH, Feldman AM, Francis GS, Ganiats TG, Jessup M, Konstam MA, Mancini DM, Michl K, Oates JA, Rahko PS, Silver MA, Stevenson LW, Yancy CW, Antman EM, Smith SC Jr, Adams CD, Anderson JL, Faxon DP, Fuster V, Halperin JL, Hiratzka LF, Jacobs AK, Nishimura R, Ornato JP, Page RL, Riegel B, American College of C, American Heart Association Task Force on Practice G, American College of Chest P, International Society for H, Lung T, Heart Rhythm S (2005) ACC/AHA 2005 Guideline update for the diagnosis and management of chronic heart failure in the adult: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure): developed in collaboration with the American College of Chest Physicians and the International Society for Heart and Lung Transplantation: endorsed by the Heart Rhythm Society. Circulation 112(12):e154–e235. https://doi.org/10.1161/CIRCULATIONAHA.105.167586
Dickstein K, Cohen-Solal A, Filippatos G, McMurray JJ, Ponikowski P, Poole-Wilson PA, Stromberg A, van Veldhuisen DJ, Atar D, Hoes AW, Keren A, Mebazaa A, Nieminen M, Priori SG, Swedberg K, Guidelines ESCCP (2008) ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: the Task Force for the diagnosis and treatment of acute and chronic heart failure 2008 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association of the ESC (HFA) and endorsed by the European Society of Intensive Care Medicine (ESICM). Eur J Heart Fail 10(10):933–989. https://doi.org/10.1016/j.ejheart.2008.08.005
Writing Committee M, Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Colvin MM, Drazner MH, Filippatos G, Fonarow GC, Givertz MM, Hollenberg SM, Lindenfeld J, Masoudi FA, McBride PE, Peterson PN, Stevenson LW, Westlake C (2016) 2016 ACC/AHA/HFSA focused update on new pharmacological therapy for heart failure: an update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. Circulation 134(13):e282–e293. https://doi.org/10.1161/CIR.0000000000000435
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, Falk V, Gonzalez-Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GM, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P, Authors/task force M, Document R (2016) 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail 18(8):891–975. https://doi.org/10.1002/ejhf.592
Remme WJ, Swedberg K (2001) Task force for the D, treatment of chronic heart failure ESoC (2001) Guidelines for the diagnosis and treatment of chronic heart failure. Eur Heart J 22(17):1527–1560. https://doi.org/10.1053/euhj.2001.2783
Remme WJ, Swedberg K, European Society of C (2002) Comprehensive guidelines for the diagnosis and treatment of chronic heart failure. Task force for the diagnosis and treatment of chronic heart failure of the European Society of Cardiology. Eur J Heart Fail 4(1):11–22
Swedberg K, Cleland J, Dargie H, Drexler H, Follath F, Komajda M, Tavazzi L, Smiseth OA, Gavazzi A, Haverich A, Hoes A, Jaarsma T, Korewicki J, Levy S, Linde C, Lopez-Sendon JL, Nieminen MS, Pierard L, Remme WJ, Task force for the D, treatment of chronic heart failure of the European Society of C (2005) Guidelines for the diagnosis and treatment of chronic heart failure: executive summary (update 2005): the task force for the diagnosis and treatment of chronic heart failure of the European Society of Cardiology. Eur Heart J 26(11):1115–1140. https://doi.org/10.1093/eurheartj/ehi204
McMurray JJ, Adamopoulos S, Anker SD, Auricchio A, Bohm M, Dickstein K, Falk V, Filippatos G, Fonseca C, Gomez-Sanchez MA, Jaarsma T, Kober L, Lip GY, Maggioni AP, Parkhomenko A, Pieske BM, Popescu BA, Ronnevik PK, Rutten FH, Schwitter J, Seferovic P, Stepinska J, Trindade PT, Voors AA, Zannad F, Zeiher A, Guidelines ESCCP (2012) ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: the task force for the diagnosis and treatment of acute and chronic heart failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J 33(14):1787–1847. https://doi.org/10.1093/eurheartj/ehs104
Pitt B, Zannad F, Remme WJ, Cody R, Castaigne A, Perez A, Palensky J, Wittes J (1999) The effect of spironolactone on morbidity and mortality in patients with severe heart failure. Randomized Aldactone Evaluation Study Investigators. N Engl J Med 341(10):709–717. https://doi.org/10.1056/NEJM199909023411001
Pitt B, Remme W, Zannad F, Neaton J, Martinez F, Roniker B, Bittman R, Hurley S, Kleiman J, Gatlin M, Eplerenone post-acute myocardial infarction heart failure E, survival study I (2003) Eplerenone, a selective aldosterone blocker, in patients with left ventricular dysfunction after myocardial infarction. N Engl J Med 348(14):1309–1321. https://doi.org/10.1056/NEJMoa030207
Zannad F, McMurray JJ, Krum H, van Veldhuisen DJ, Swedberg K, Shi H, Vincent J, Pocock SJ, Pitt B, Group E-HS (2011) Eplerenone in patients with systolic heart failure and mild symptoms. N Engl J Med 364(1):11–21. https://doi.org/10.1056/NEJMoa1009492
Frankenstein L, Katus HA, Grundtvig M, Hole T, de Blois J, Schellberg D, Atar D, Zugck C, Agewall S (2013) Norwegian Heart Failure Registry Steering C (2013) Association between spironolactone added to beta-blockers and ACE inhibition and survival in heart failure patients with reduced ejection fraction: a propensity score-matched cohort study. Eur J Clin Pharmacol 69(10):1747–1755. https://doi.org/10.1007/s00228-013-1512-x
Ezekowitz JA, McAlister FA (2009) Aldosterone blockade and left ventricular dysfunction: a systematic review of randomized clinical trials. Eur Heart J 30(4):469–477. https://doi.org/10.1093/eurheartj/ehn543
Chatterjee S, Moeller C, Shah N, Bolorunduro O, Lichstein E, Moskovits N, Mukherjee D (2012) Eplerenone is not superior to older and less expensive aldosterone antagonists. Am J Med 125(8):817–825. https://doi.org/10.1016/j.amjmed.2011.12.018
Hu LJ, Chen YQ, Deng SB, Du JL, She Q (2013) Additional use of an aldosterone antagonist in patients with mild to moderate chronic heart failure: a systematic review and meta-analysis. Br J Clin Pharmacol 75(5):1202–1212. https://doi.org/10.1111/bcp.12012
Bapoje SR, Bahia A, Hokanson JE, Peterson PN, Heidenreich PA, Lindenfeld J, Allen LA, Masoudi FA (2013) Effects of mineralocorticoid receptor antagonists on the risk of sudden cardiac death in patients with left ventricular systolic dysfunction: a meta-analysis of randomized controlled trials. Circ Heart Fail 6(2):166–173. https://doi.org/10.1161/CIRCHEARTFAILURE.112.000003
Higgins J, Green S (2011) Cochrane handbook for systematic reviews of interventions version 5.1.0 [updated march 2011]
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339:b2535. https://doi.org/10.1136/bmj.b2535
Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, Cameron C, Ioannidis JP, Straus S, Thorlund K, Jansen JP, Mulrow C, Catala-Lopez F, Gotzsche PC, Dickersin K, Boutron I, Altman DG, Moher D (2015) The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med 162(11):777–784. https://doi.org/10.7326/M14-2385
Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA, Cochrane Bias Methods G, Cochrane Statistical Methods G (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928. https://doi.org/10.1136/bmj.d5928
Woods BS, Hawkins N, Scott DA (2010) Network meta-analysis on the log-hazard scale, combining count and hazard ratio statistics accounting for multi-arm trials: a tutorial. BMC Med Res Methodol 10:54. https://doi.org/10.1186/1471-2288-10-54
Chaimani A, Higgins JP, Mavridis D, Spyridonos P, Salanti G (2013) Graphical tools for network meta-analysis in STATA. PLoS One 8(10):e76654. https://doi.org/10.1371/journal.pone.0076654
Salanti G, Ades AE, Ioannidis JP (2011) Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J Clin Epidemiol 64(2):163–171. https://doi.org/10.1016/j.jclinepi.2010.03.016
Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Colvin MM, Drazner MH, Filippatos G, Fonarow GC, Givertz MM, Hollenberg SM, Lindenfeld J, Masoudi FA, McBride PE, Peterson PN, Stevenson LW, Westlake C (2016) 2016 ACC/AHA/HFSA focused update on new pharmacological therapy for heart failure: an update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. J Am Coll Cardiol 68(13):1476–1488. https://doi.org/10.1016/j.jacc.2016.05.011
Salanti G (2012) Indirect and mixed-treatment comparison, network, or multiple-treatments meta-analysis: many names, many benefits, many concerns for the next generation evidence synthesis tool. Res Synth Methods 3(2):80–97. https://doi.org/10.1002/jrsm.1037
Salanti G, Marinho V, Higgins JP (2009) A case study of multiple-treatments meta-analysis demonstrates that covariates should be considered. J Clin Epidemiol 62(8):857–864. https://doi.org/10.1016/j.jclinepi.2008.10.001
R: a language and environment for statistical computing (2018) R Foundation for Statistical Computing. https://www.R-project.org/
netmeta: Network Meta-Analysis using Frequentist Methods. R package version 0.9-8 (2018) https://CRAN.R-project.org/package=netmeta
Thomas A, O'Hara B, Ligges U, Sturtz S (2006) Making BUGS Open. R News 6(1):12–17
Lunn DJ, Thomas A, Best N, Spiegelhalter D (2000) WinBUGS—a Bayesian modeling framework: concepts, structure and extensibility. Stat Comput 10:325–337
Agostoni P, Magini A, Andreini D, Contini M, Apostolo A, Bussotti M, Cattadori G, Palermo P (2005) Spironolactone improves lung diffusion in chronic heart failure. Eur Heart J 26(2):159–164. https://doi.org/10.1093/eurheartj/ehi023
Akbulut M, Ozbay Y, Ilkay E, Karaca I, Arslan N (2003) Effects of spironolactone and metoprolol on QT dispersion in heart failure. Jpn Heart J 44(5):681–692
Barr CS, Lang CC, Hanson J, Arnott M, Kennedy N, Struthers AD (1995) Effects of adding spironolactone to an angiotensin-converting enzyme inhibitor in chronic congestive heart failure secondary to coronary artery disease. Am J Cardiol 76(17):1259–1265
Boccanelli A, Mureddu GF, Cacciatore G, Clemenza F, Di Lenarda A, Gavazzi A, Porcu M, Latini R, Lucci D, Maggioni AP, Masson S, Vanasia M, de Simone G, Investigators AI-C (2009) Anti-remodelling effect of canrenone in patients with mild chronic heart failure (AREA IN-CHF study): final results. Eur J Heart Fail 11(1):68–76. https://doi.org/10.1093/eurjhf/hfn015
Chan AK, Sanderson JE, Wang T, Lam W, Yip G, Wang M, Lam YY, Zhang Y, Yeung L, Wu EB, Chan WW, Wong JT, So N, Yu CM (2007) Aldosterone receptor antagonism induces reverse remodeling when added to angiotensin receptor blockade in chronic heart failure. J Am Coll Cardiol 50(7):591–596. https://doi.org/10.1016/j.jacc.2007.03.062
Cicoira M, Zanolla L, Rossi A, Golia G, Franceschini L, Brighetti G, Marino P, Zardini P (2002) Long-term, dose-dependent effects of spironolactone on left ventricular function and exercise tolerance in patients with chronic heart failure. J Am Coll Cardiol 40(2):304–310
Kasama S, Toyama T, Sumino H, Matsumoto N, Sato Y, Kumakura H, Takayama Y, Ichikawa S, Suzuki T, Kurabayashi M (2007) Additive effects of spironolactone and candesartan on cardiac sympathetic nerve activity and left ventricular remodeling in patients with congestive heart failure. J Nucl Med 48(12):1993–2000. https://doi.org/10.2967/jnumed.107.045427
Effectiveness of spironolactone added to an angiotensin-converting enzyme inhibitor and a loop diuretic for severe chronic congestive heart failure (the Randomized Aldactone Evaluation Study [RALES]) (1996) Am J Cardiol 78(8):902–907
Ramires FJ, Mansur A, Coelho O, Maranhao M, Gruppi CJ, Mady C, Ramires JA (2000) Effect of spironolactone on ventricular arrhythmias in congestive heart failure secondary to idiopathic dilated or to ischemic cardiomyopathy. Am J Cardiol 85(10):1207–1211
Tsutamoto T, Wada A, Maeda K, Mabuchi N, Hayashi M, Tsutsui T, Ohnishi M, Sawaki M, Fujii M, Matsumoto T, Matsui T, Kinoshita M (2001) Effect of spironolactone on plasma brain natriuretic peptide and left ventricular remodeling in patients with congestive heart failure. J Am Coll Cardiol 37(5):1228–1233
Wu J-L, Hou D-Y, Ma G-L, Liang Y-H, Wand H, Xu L, Zhao W-S, Zhang Z-Y, Chen J, Liu J-M, Zhang L (2016) Effects of long-term low-dose spironolactone treatment in patients with New York Heart Association functional class II heart failure: a 10-year prospective study. Int J Clin Exp Med 9(8):15689–15698
Boccanelli A, Cacciatore G, Mureddu GF, de Simone G, Clemenza F, De Maria R, Di Lenarda A, Gavazzi A, Latini R, Masson S, Porcu M, Vanasia M, Gonzini L, Maggioni AP (2007) Baseline characteristics of patients recruited in the AREA IN-CHF study (Antiremodelling Effect of Aldosterone Receptors Blockade with Canrenone in Mild Chronic Heart Failure). J Cardiovasc Med (Hagerstown) 8(9):683–691. https://doi.org/10.2459/JCM.0b013e3281053a9a
Korol S, Mottet F, Perreault S, Baker WL, White M, de Denus S (2017) A systematic review and meta-analysis of the impact of mineralocorticoid receptor antagonists on glucose homeostasis. Medicine (Baltimore) 96(48):e8719. https://doi.org/10.1097/MD.0000000000008719
Zhao JV, Xu L, Lin SL, Schooling CM (2016) Spironolactone and glucose metabolism, a systematic review and meta-analysis of randomized controlled trials. J Am Soc Hypertens 10(8):671–682. https://doi.org/10.1016/j.jash.2016.05.013
Struthers AD, MacDonald TM (2004) Review of aldosterone- and angiotensin II-induced target organ damage and prevention. Cardiovasc Res 61(4):663–670. https://doi.org/10.1016/j.cardiores.2003.11.037
Macdonald JE, Kennedy N, Struthers AD (2004) Effects of spironolactone on endothelial function, vascular angiotensin converting enzyme activity, and other prognostic markers in patients with mild heart failure already taking optimal treatment. Heart 90(7):765–770. https://doi.org/10.1136/hrt.2003.017368
Funding
All authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Author information
Authors and Affiliations
Contributions
L.F., T.T., H.F.: conception and design of the work, and acquisition and interpretation of data; drafting and revising of the manuscript; final approval of the manuscript submitted. S.S., K.J., L.U.: design of the work and analysis and interpretation of data; revising of the manuscript; final approval of the manuscript submitted. A.C., M.S., H.K., P.N., H.N., D.A.: design of the work and interpretation of data; revising of the manuscript; final approval of the manuscript submitted.
Corresponding author
Ethics declarations
Competing interests
None declared.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 99 kb)
Rights and permissions
About this article
Cite this article
Frankenstein, L., Seide, S., Täger, T. et al. Relative Efficacy of Spironolactone, Eplerenone, and cAnRenone in patients with Chronic Heart failure (RESEARCH): a systematic review and network meta-analysis of randomized controlled trials. Heart Fail Rev 25, 161–171 (2020). https://doi.org/10.1007/s10741-019-09832-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10741-019-09832-y