Abstract
The cardiovascular system is particularly sensitive to androgens, but some controversies exist regarding the effect of testosterone on the heart. While among anabolic abusers, cases of sudden cardiac death have been described, recently it was reported that low serum level of testosterone was correlated with increased risk of cardiovascular diseases (CVD) and mortality rate. This review aims to evaluate the effect of testosterone on myocardial tissue function, coronary artery disease (CAD), and death. Low testosterone level is associated with increased incidence of CAD and mortality. Testosterone administration in hypogonadal elderly men and women has a positive effect on cardiovascular function and improved clinical outcomes and survival time. Although at supraphysiologic doses, androgen may have a toxic effect, and at physiological levels, testosterone is safe and exerts a beneficial effect on myocardial function including mechanisms at cellular and mitochondrial level. The interaction with free testosterone and estradiol should be considered. Further studies are necessary to better understand the interaction mechanisms for an optimal androgen therapy in CVD.

Similar content being viewed by others
References
Calof OM, Singh AB, Lee ML, Kenny AM, Urban RJ, Tenover JL, Bhasin S (2005) Adverse events associated with testosterone replacement in middle-aged and older men: a meta-analysis of randomized, placebo-controlled trials. J Gerontol A Biol Sci Med Sci 60(11):1451–1457
Haddad RM, Kennedy CC, Caples SM, Tracz MJ, Bolona ER, Sideras K, Uraga MV, Erwin PJ, Montori VM (2007) Testosterone and cardiovascular risk in men: a systematic review and meta-analysis of randomized placebo-controlled trials. Mayo Clin Proc 82(1):29–39. https://doi.org/10.4065/82.1.29
Fernandez-Balsells MM, Murad MH, Lane M, Lampropulos JF, Albuquerque F, Mullan RJ, Agrwal N, Elamin MB, Gallegos-Orozco JF, Wang AT, Erwin PJ, Bhasin S, Montori VM (2010) Clinical review 1: adverse effects of testosterone therapy in adult men: a systematic review and meta-analysis. J Clin Endocrinol Metab 95(6):2560–2575. https://doi.org/10.1210/jc.2009-2575
Huie MJ (1994) An acute myocardial infarction occurring in an anabolic steroid user. Med Sci Sports Exerc 26(4):408–413
Wysoczanski M, Rachko M, Bergmann SR (2008) Acute myocardial infarction in a young man using anabolic steroids. Angiology 59(3):376–378. https://doi.org/10.1177/0003319707304883
Stergiopoulos K, Brennan JJ, Mathews R, Setaro JF, Kort S (2008) Anabolic steroids, acute myocardial infarction and polycythemia: a case report and review of the literature. Vasc Health Risk Manag 4(6):1475–1480
Kennedy C (1993) Myocardial infarction in association with misuse of anabolic steroids. Ulster Med J 62(2):174–176
McNutt RA, Ferenchick GS, Kirlin PC, Hamlin NJ (1988) Acute myocardial infarction in a 22-year-old world class weight lifter using anabolic steroids. Am J Cardiol 62(1):164
Bowman S (1990) Anabolic steroids and infarction. Bmj 300(6726):750
Goldstein DR, Dobbs T, Krull B, Plumb VJ (1998) Clenbuterol and anabolic steroids: a previously unreported cause of myocardial infarction with normal coronary arteriograms. South Med J 91(8):780–784
Fisher M, Appleby M, Rittoo D, Cotter L (1996) Myocardial infarction with extensive intracoronary thrombus induced by anabolic steroids. Br J Clin Pract 50(4):222–223
Kennedy MC, Lawrence C (1993) Anabolic steroid abuse and cardiac death. Med J Aust 158(5):346–348
Weidemann W, Hanke H (2002) Cardiovascular effects of androgens. Cardiovasc Drug Rev 20(3):175–198
Sullivan ML, Martinez CM, Gennis P, Gallagher EJ (1998) The cardiac toxicity of anabolic steroids. Prog Cardiovasc Dis 41(1):1–15
Parssinen M, Seppala T (2002) Steroid use and long-term health risks in former athletes. Sports Med 32(2):83–94
Wilson JD (1988) Androgen abuse by athletes. Endocr Rev 9(2):181–199. https://doi.org/10.1210/edrv-9-2-181
Yesalis CE, Kennedy NJ, Kopstein AN, Bahrke MS (1993) Anabolic-androgenic steroid use in the United States. JAMA 270(10):1217–1221
Araujo AB, O’Donnell AB, Brambilla DJ, Simpson WB, Longcope C, Matsumoto AM, McKinlay JB (2004) Prevalence and incidence of androgen deficiency in middle-aged and older men: estimates from the Massachusetts Male aging study. J Clin Endocrinol Metab 89(12):5920–5926. https://doi.org/10.1210/jc.2003-031719
Travison TG, Araujo AB, Kupelian V, O’Donnell AB, McKinlay JB (2007) The relative contributions of aging, health, and lifestyle factors to serum testosterone decline in men. J Clin Endocrinol Metab 92(2):549–555. https://doi.org/10.1210/jc.2006-1859
Cunningham GO, Michael YL (2004) Concepts guiding the study of the impact of the built environment on physical activity for older adults: a review of the literature. Am J Health Promot 18(6):435–443
Araujo AB, Esche GR, Kupelian V, O’Donnell AB, Travison TG, Williams RE, Clark RV, McKinlay JB (2007) Prevalence of symptomatic androgen deficiency in men. J Clin Endocrinol Metab 92(11):4241–4247. https://doi.org/10.1210/jc.2007-1245
Bassil N, Alkaade S, Morley JE (2009) The benefits and risks of testosterone replacement therapy: a review. Ther Clin Risk Manag 5(3):427–448
Gan EH, Pattman S, Pearce S, Quinton R (2012) Many men are receiving unnecessary testosterone prescriptions. BMJ 345:e5469. https://doi.org/10.1136/bmj.e5469
Altieri P, Barisione C, Lazzarini E, Garuti A, Bezante GP, Canepa M, Spallarossa P, Tocchetti CG, Bollini S, Brunelli C, Ameri P (2016) Testosterone antagonizes doxorubicin-induced senescence of cardiomyocytes. J Am Heart Assoc 8(5):1-13. https://doi.org/10.1161/JAHA.115.002383
Borst SE, Quindry JC, Yarrow JF, Conover CF, Powers SK (2010) Testosterone administration induces protection against global myocardial ischemia. Horm Metab Res 42(2):122–129. https://doi.org/10.1055/s-0029-1241843
Pongkan W, Chattipakorn SC, Chattipakorn N (2015) Roles of testosterone replacement in cardiac ischemia-reperfusion injury. J Cardiovasc Pharmacol Ther. 21(1):27–43. https://doi.org/10.1177/1074248415587977
Yang J, Wang F, Sun W, Dong Y, Li M, Fu L (2016) Testosterone replacement modulates cardiac metabolic remodeling after myocardial infarction by upregulating PPARalpha. PPAR Res 2016:4518754. https://doi.org/10.1155/2016/4518754
Xiao FY, Nheu L, Komesaroff P, Ling S (2015) Testosterone protects cardiac myocytes from superoxide injury via NF-kappaB signalling pathways. Life Sci 133:45–52. https://doi.org/10.1016/j.lfs.2015.05.009
Manning BD, Cantley LC (2007) AKT/PKB signaling: navigating downstream. Cell 129(7):1261–1274. https://doi.org/10.1016/j.cell.2007.06.009
Perkins ND (2007) Integrating cell-signalling pathways with NF-kappaB and IKK function. Nat Rev Mol Cell Biol 8(1):49–62. https://doi.org/10.1038/nrm2083
Witayavanitkul N, Woranush W, Bupha-Intr T, Wattanapermpool J (2013) Testosterone regulates cardiac contractile activation by modulating SERCA but not NCX activity. Am J Physiol Heart Circ Physiol 304(3):H465–H472. https://doi.org/10.1152/ajpheart.00555.2012
Tsang S, Wong SS, Wu S, Kravtsov GM, Wong TM (2009) Testosterone-augmented contractile responses to alpha1- and beta1-adrenoceptor stimulation are associated with increased activities of RyR, SERCA, and NCX in the heart. Am J Physiol Cell Physiol 296(4):C766–C782. https://doi.org/10.1152/ajpcell.00193.2008
Dutta D, Calvani R, Bernabei R, Leeuwenburgh C, Marzetti E (2012) Contribution of impaired mitochondrial autophagy to cardiac aging: mechanisms and therapeutic opportunities. Circ Res 110(8):1125–1138. https://doi.org/10.1161/CIRCRESAHA.111.246108
Wang F, Yang J, Sun J, Dong Y, Zhao H, Shi H, Fu L (2015) Testosterone replacement attenuates mitochondrial damage in a rat model of myocardial infarction. J Endocrinol 225(2):101–111. https://doi.org/10.1530/JOE-14-0638
Usui T, Kajita K, Kajita T, Mori I, Hanamoto T, Ikeda T, Okada H, Taguchi K, Kitada Y, Morita H, Sasaki T, Kitamura T, Sato T, Kojima I, Ishizuka T (2014) Elevated mitochondrial biogenesis in skeletal muscle is associated with testosterone-induced body weight loss in male mice. FEBS Lett 588(10):1935–1941. https://doi.org/10.1016/j.febslet.2014.03.051
Ikeda Y, Aihara K, Akaike M, Sato T, Ishikawa K, Ise T, Yagi S, Iwase T, Ueda Y, Yoshida S, Azuma H, Walsh K, Tamaki T, Kato S, Matsumoto T (2010) Androgen receptor counteracts doxorubicin-induced cardiotoxicity in male mice. Mol Endocrinol 24(7):1338–1348. https://doi.org/10.1210/me.2009-0402
Skogastierna C, Hotzen M, Rane A, Ekstrom L (2014) A supraphysiological dose of testosterone induces nitric oxide production and oxidative stress. Eur J Prev Cardiol 21(8):1049–1054. https://doi.org/10.1177/2047487313481755
Victor VM, Rocha M, Banuls C, Rovira-Llopis S, Gomez M, Hernandez-Mijares A (2014) Mitochondrial impairment and oxidative stress in leukocytes after testosterone administration to female-to-male transsexuals. J Sex Med 11(2):454–461. https://doi.org/10.1111/jsm.12376
Hanke H, Lenz C, Hess B, Spindler KD, Weidemann W (2001) Effect of testosterone on plaque development and androgen receptor expression in the arterial vessel wall. Circulation 103(10):1382–1385
Fujimoto R, Morimoto I, Morita E, Sugimoto H, Ito Y, Eto S (1994) Androgen receptors, 5 alpha-reductase activity and androgen-dependent proliferation of vascular smooth muscle cells. J Steroid Biochem Mol Biol 50(3–4):169–174
Marsh JD, Lehmann MH, Ritchie RH, Gwathmey JK, Green GE, Schiebinger RJ (1998) Androgen receptors mediate hypertrophy in cardiac myocytes. Circulation 98(3):256–261
Ikeda Y, Aihara K, Sato T, Akaike M, Yoshizumi M, Suzaki Y, Izawa Y, Fujimura M, Hashizume S, Kato M, Yagi S, Tamaki T, Kawano H, Matsumoto T, Azuma H, Kato S, Matsumoto T (2005) Androgen receptor gene knockout male mice exhibit impaired cardiac growth and exacerbation of angiotensin II-induced cardiac fibrosis. J Biol Chem 280(33):29661–29666. https://doi.org/10.1074/jbc.M411694200
Ikeda Y, Aihara K, Yoshida S, Sato T, Yagi S, Iwase T, Sumitomo Y, Ise T, Ishikawa K, Azuma H, Akaike M, Kato S, Matsumoto T (2009) Androgen-androgen receptor system protects against angiotensin II-induced vascular remodeling. Endocrinology 150(6):2857–2864. https://doi.org/10.1210/en.2008-1254
Liu K, Shen C, Chen X (2015) Expression of androgen receptor in coronary artery in the cases of sudden coronary death. Int J Clin Exp Pathol 8(4):3742–3747
Svartberg J, von Muhlen D, Mathiesen E, Joakimsen O, Bonaa KH, Stensland-Bugge E (2006) Low testosterone levels are associated with carotid atherosclerosis in men. J Intern Med 259(6):576–582. https://doi.org/10.1111/j.1365-2796.2006.01637.x
Sieveking DP, Lim P, Chow RW, Dunn LL, Bao S, McGrath KC, Heather AK, Handelsman DJ, Celermajer DS, Ng MK (2010) A sex-specific role for androgens in angiogenesis. J Exp Med 207(2):345–352. https://doi.org/10.1084/jem.20091924
Grohe C, Kahlert S, Lobbert K, Vetter H (1998) Expression of oestrogen receptor alpha and beta in rat heart: role of local oestrogen synthesis. J Endocrinol 156(2):R1–R7
Karas RH, Patterson BL, Mendelsohn ME (1994) Human vascular smooth muscle cells contain functional estrogen receptor. Circulation 89(5):1943–1950
Losordo DW, Kearney M, Kim EA, Jekanowski J, Isner JM (1994) Variable expression of the estrogen receptor in normal and atherosclerotic coronary arteries of premenopausal women. Circulation 89(4):1501–1510
Hodges YK, Tung L, Yan XD, Graham JD, Horwitz KB, Horwitz LD (2000) Estrogen receptors alpha and beta: prevalence of estrogen receptor beta mRNA in human vascular smooth muscle and transcriptional effects. Circulation 101(15):1792–1798
Mendelsohn ME, Karas RH (1999) The protective effects of estrogen on the cardiovascular system. N Engl J Med 340(23):1801–1811. https://doi.org/10.1056/NEJM199906103402306
Bell JR, Mellor KM, Wollermann AC, Ip WT, Reichelt ME, Meachem SJ, Simpson ER, Delbridge LM (2011) Aromatase deficiency confers paradoxical postischemic cardioprotection. Endocrinology 152(12):4937–4947. https://doi.org/10.1210/en.2011-1212
Kararigas G, Nguyen BT, Jarry H (2014) Estrogen modulates cardiac growth through an estrogen receptor alpha-dependent mechanism in healthy ovariectomized mice. Mol Cell Endocrinol 382(2):909–914. https://doi.org/10.1016/j.mce.2013.11.011
Babiker FA, Lips DJ, Delvaux E, Zandberg P, Janssen BJ, Prinzen F, van Eys G, Grohe C, Doevendans PA (2007) Oestrogen modulates cardiac ischaemic remodelling through oestrogen receptor-specific mechanisms. Acta Physiol (Oxford) 189(1):23–31. https://doi.org/10.1111/j.1748-1716.2006.01633.x
Pugach EK, Blenck CL, Dragavon JM, Langer SJ, Leinwand LA (2016) Estrogen receptor profiling and activity in cardiac myocytes. Mol Cell Endocrinol 431:62–70. https://doi.org/10.1016/j.mce.2016.05.004
Schuster I, Mahmoodzadeh S, Dworatzek E, Jaisser F, Messaoudi S, Morano I, Regitz-Zagrosek V (2016) Cardiomyocyte-specific overexpression of oestrogen receptor beta improves survival and cardiac function after myocardial infarction in female and male mice. Clin Sci (Lond) 130(5):365–376. https://doi.org/10.1042/CS20150609
Weinberg EO, Thienelt CD, Katz SE, Bartunek J, Tajima M, Rohrbach S, Douglas PS, Lorell BH (1999) Gender differences in molecular remodeling in pressure overload hypertrophy. J Am Coll Cardiol 34(1):264–273
Cavasin MA, Sankey SS, Yu AL, Menon S, Yang XP (2003) Estrogen and testosterone have opposing effects on chronic cardiac remodeling and function in mice with myocardial infarction. Am J Phys Heart Circ Phys 284(5):H1560–H1569. https://doi.org/10.1152/ajpheart.01087.2002
Malhotra A, Buttrick P, Scheuer J (1990) Effects of sex hormones on development of physiological and pathological cardiac hypertrophy in male and female rats. Am J Phys 259(3 Pt 2):H866–H871
Pham TV, Rosen MR (2002) Sex, hormones, and repolarization. Cardiovasc Res 53(3):740–751
Morita H, Wu J, Zipes DP (2008) The QT syndromes: long and short. Lancet 372(9640):750–763. https://doi.org/10.1016/S0140-6736(08)61307-0
Surawicz B, Parikh SR (2003) Differences between ventricular repolarization in men and women: description, mechanism and implications. Ann Noninvasive Electrocardiol 8(4):333–340
Charbit B, Christin-Maitre S, Demolis JL, Soustre E, Young J, Funck-Brentano C (2009) Effects of testosterone on ventricular repolarization in hypogonadic men. Am J Cardiol 103(6):887–890. https://doi.org/10.1016/j.amjcard.2008.11.041
Rautaharju PM, Zhou SH, Wong S, Calhoun HP, Berenson GS, Prineas R, Davignon A (1992) Sex differences in the evolution of the electrocardiographic QT interval with age. Can J Cardiol 8(7):690–695
Pecori Giraldi F, Toja PM, Filippini B, Michailidis J, Scacchi M, Stramba Badiale M, Cavagnini F (2010) Increased prevalence of prolonged QT interval in males with primary or secondary hypogonadism: a pilot study. Int J Androl 33(1):e132–e138. https://doi.org/10.1111/j.1365-2605.2009.00985.x
Pecori Giraldi F, Manzoni G, Michailidis J, Scacchi M, Stramba-Badiale M, Cavagnini F (2011) High prevalence of prolonged QT interval in obese hypogonadal males. Obesity (Silver Spring) 19(10):2015–2018. https://doi.org/10.1038/oby.2011.33
Bidoggia H, Maciel JP, Capalozza N, Mosca S, Blaksley EJ, Valverde E, Bertran G, Arini P, Biagetti MO, Quinteiro RA (2000) Sex differences on the electrocardiographic pattern of cardiac repolarization: possible role of testosterone. Am Heart J 140(4):678–683. https://doi.org/10.1067/mhj.2000.109918
Lubart E, Yarovoy A, Gal G, Krakover R, Leibovitz A (2015) QT interval length in elderly prostatic cancer patients on anti-testosterone treatment. Isr Med Assoc J 17(6):356–359
Cheng J (2006) Evidences of the gender-related differences in cardiac repolarization and the underlying mechanisms in different animal species and human. Fundam Clin Pharmacol 20(1):1–8. https://doi.org/10.1111/j.1472-8206.2005.00384.x
Malkin CJ, Morris PD, Pugh PJ, English KM, Channer KS (2003) Effect of testosterone therapy on QT dispersion in men with heart failure. Am J Cardiol 92(10):1241–1243
van Noord C, Dorr M, Sturkenboom MC, Straus SM, Reffelmann T, Felix SB, Hofman A, Kors JA, Haring R, de Jong FH, Nauck M, Uitterlinden AG, Wallaschofski H, Witteman JC, Volzke H, Stricker BH (2010) The association of serum testosterone levels and ventricular repolarization. Eur J Epidemiol 25(1):21–28. https://doi.org/10.1007/s10654-009-9406-z
Bai CX, Kurokawa J, Tamagawa M, Nakaya H, Furukawa T (2005) Nontranscriptional regulation of cardiac repolarization currents by testosterone. Circulation 112(12):1701–1710. https://doi.org/10.1161/CIRCULATIONAHA.104.523217
Kurokawa J, Furukawa T (2013) Non-genomic action of sex steroid hormones and cardiac repolarization. Biol Pharm Bull 36(1):8–12
Fulop L, Banyasz T, Szabo G, Toth IB, Biro T, Lorincz I, Balogh A, Peto K, Miko I, Nanasi PP (2006) Effects of sex hormones on ECG parameters and expression of cardiac ion channels in dogs. Acta Physiol 188(3–4):163–171. https://doi.org/10.1111/j.1748-1716.2006.01618.x
James AF, Choisy SC, Hancox JC (2007) Recent advances in understanding sex differences in cardiac repolarization. Prog Biophys Mol Biol 94(3):265–319. https://doi.org/10.1016/j.pbiomolbio.2005.05.010
Bigi MA, Aslani A, Aslani A (2009) Short qt interval: a novel predictor of androgen abuse in strength trained athletes. Ann Noninvasive Electrocardiol 14(1):35–39. https://doi.org/10.1111/j.1542-474X.2008.00271.x
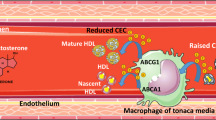
Nettleship JE, Jones TH, Channer KS, Jones RD (2007) Physiological testosterone replacement therapy attenuates fatty streak formation and improves high-density lipoprotein cholesterol in the Tfm mouse: an effect that is independent of the classic androgen receptor. Circulation 116(21):2427–2434. https://doi.org/10.1161/CIRCULATIONAHA.107.708768
Chung SD, Chen YK, Wu FJ, Lin HC (2012) Hormone therapy for prostate cancer and the risk of stroke: a 5-year follow-up study. BJU Int 109(7):1001–1005. https://doi.org/10.1111/j.1464-410X.2011.10459.x
Martin-Merino E, Johansson S, Morris T, Garcia Rodriguez LA (2011) Androgen deprivation therapy and the risk of coronary heart disease and heart failure in patients with prostate cancer: a nested case-control study in UK primary care. Drug Saf 34(11):1061–1077. https://doi.org/10.2165/11594540-000000000-00000
Nguyen CT, Aaronson A, Morrissey RP, Agarwal M, Willix RD, Schwarz ER (2011) Myths and truths of growth hormone and testosterone therapy in heart failure. Expert Rev Cardiovasc Ther 9(6):711–720. https://doi.org/10.1586/erc.11.25
Collier A, Ghosh S, McGlynn B, Hollins G (2012) Prostate cancer, androgen deprivation therapy, obesity, the metabolic syndrome, type 2 diabetes, and cardiovascular disease: a review. Am J Clin Oncol 35(5):504–509. https://doi.org/10.1097/COC.0b013e318201a406
Tsai HK, D’Amico AV, Sadetsky N, Chen MH, Carroll PR (2007) Androgen deprivation therapy for localized prostate cancer and the risk of cardiovascular mortality. J Natl Cancer Inst 99(20):1516–1524. https://doi.org/10.1093/jnci/djm168
Huang F (2018) Is a previously or currently reduced testosterone level in male patients with type 2 diabetes mellitus a risk factor for the development of coronary artery disease? A Systematic Review and Meta-analysis. Diabetes Ther 9(3):1061-1072. https://doi.org/10.1007/s13300-018-0415-3
Budoff MJ, Ellenberg SS, Lewis CE, Mohler ER 3rd, Wenger NK, Bhasin S, Barrett-Connor E, Swerdloff RS, Stephens-Shields A, Cauley JA, Crandall JP, Cunningham GR, Ensrud KE, Gill TM, Matsumoto AM, Molitch ME, Nakanishi R, Nezarat N, Matsumoto S, Hou X, Basaria S, Diem SJ, Wang C, Cifelli D, Snyder PJ (2017) Testosterone treatment and coronary artery plaque volume in older men with low testosterone. JAMA 317(7):708–716. https://doi.org/10.1001/jama.2016.21043
Abd Alamir M, Ellenberg SS, Swerdloff RS, Wenger NK, Mohler ER 3rd, Lewis CE, Barrett-Conner E, Nakanishi R, Darabian S, Alani A, Matsumoto S, Nezarat N, Snyder PJ, Budoff MJ (2016) The Cardiovascular trial of the testosterone trials: rationale, design, and baseline data of a clinical trial using computed tomographic imaging to assess the progression of coronary atherosclerosis. Coron Artery Dis 27(2):95–103. https://doi.org/10.1097/MCA.0000000000000321
Chan YX, Knuiman MW, Hung J, Divitini ML, Handelsman DJ, Beilby JP, McQuillan B, Yeap BB (2015) Testosterone, dihydrotestosterone and estradiol are differentially associated with carotid intima-media thickness and the presence of carotid plaque in men with and without coronary artery disease. Endocr J 62(9):777–786. https://doi.org/10.1507/endocrj.EJ15-0196
Khazai B, Golden SH, Colangelo LA, Swerdloff R, Wang C, Honoris L, Gapstur SM, Ouyang P, Cushman M, Li D, Kopp P, Vaidya D, Liu K, Dobs A, Budoff M (2016) Association of endogenous testosterone with subclinical atherosclerosis in men: the multi-ethnic study of atherosclerosis. Clin Endocrinol 84(5):700–707. https://doi.org/10.1111/cen.12997
Basaria S, Harman SM, Travison TG, Hodis H, Tsitouras P, Budoff M, Pencina KM, Vita J, Dzekov C, Mazer NA, Coviello AD, Knapp PE, Hally K, Pinjic E, Yan M, Storer TW, Bhasin S (2015) Effects of testosterone administration for 3 years on subclinical atherosclerosis progression in older men with low or low-normal testosterone levels: a randomized clinical trial. JAMA 314(6):570–581. https://doi.org/10.1001/jama.2015.8881
Srinath R, Hill Golden S, Carson KA, Dobs A (2015) Endogenous testosterone and its relationship to preclinical and clinical measures of cardiovascular disease in the atherosclerosis risk in communities study. J Clin Endocrinol Metab 100(4):1602–1608. https://doi.org/10.1210/jc.2014-3934
Ouyang P, Vaidya D, Dobs A, Golden SH, Szklo M, Heckbert SR, Kopp P, Gapstur SM (2009) Sex hormone levels and subclinical atherosclerosis in postmenopausal women: the Multi-ethnic study of atherosclerosis. Atherosclerosis 204(1):255–261. https://doi.org/10.1016/j.atherosclerosis.2008.08.037
Vikan T, Johnsen SH, Schirmer H, Njolstad I, Svartberg J (2009) Endogenous testosterone and the prospective association with carotid atherosclerosis in men: the Tromso study. Eur J Epidemiol 24(6):289–295. https://doi.org/10.1007/s10654-009-9322-2
Soisson V, Brailly-Tabard S, Empana JP, Feart C, Ryan J, Bertrand M, Guiochon-Mantel A, Scarabin PY (2012) Low plasma testosterone and elevated carotid intima-media thickness: importance of low-grade inflammation in elderly men. Atherosclerosis 223(1):244–249. https://doi.org/10.1016/j.atherosclerosis.2012.05.009
Yeap BB, Alfonso H, Chubb SA, Handelsman DJ, Hankey GJ, Golledge J, Flicker L, Norman PE (2013) Lower plasma testosterone or dihydrotestosterone, but not estradiol, is associated with symptoms of intermittent claudication in older men. Clin Endocrinol 79(5):725–732. https://doi.org/10.1111/cen.12208
Li L, Guo CY, Jia EZ, Zhu TB, Wang LS, Cao KJ, Ma WZ, Yang ZJ (2012) Testosterone is negatively associated with the severity of coronary atherosclerosis in men. Asian J Androl 14(6):875–878. https://doi.org/10.1038/aja.2012.95
Hu X, Rui L, Zhu T, Xia H, Yang X, Wang X, Liu H, Lu Z, Jiang H (2011) Low testosterone level in middle-aged male patients with coronary artery disease. Eur J Intern Med 22(6):e133–e136. https://doi.org/10.1016/j.ejim.2011.08.016
Phillips GB, Pinkernell BH, Jing TY (1994) The association of hypotestosteronemia with coronary artery disease in men. Arterioscler Thromb 14(5):701–706
Debing E, Peeters E, Duquet W, Poppe K, Velkeniers B, Van Den Brande P (2008) Men with atherosclerotic stenosis of the carotid artery have lower testosterone levels compared with controls. Int Angiol 27(2):135–141
Brand JS, van der Schouw YT (2010) Testosterone, SHBG and cardiovascular health in postmenopausal women. Int J Impot Res 22(2):91–104. https://doi.org/10.1038/ijir.2009.64
Pierpoint T, McKeigue PM, Isaacs AJ, Wild SH, Jacobs HS (1998) Mortality of women with polycystic ovary syndrome at long-term follow-up. J Clin Epidemiol 51(7):581–586
Bernini GP, Sgro M, Moretti A, Argenio GF, Barlascini CO, Cristofani R, Salvetti A (1999) Endogenous androgens and carotid intimal-medial thickness in women. J Clin Endocrinol Metab 84(6):2008–2012. https://doi.org/10.1210/jcem.84.6.5824
Debing E, Peeters E, Duquet W, Poppe K, Velkeniers B, Van den Brande P (2007) Endogenous sex hormone levels in postmenopausal women undergoing carotid artery endarterectomy. Eur J Endocrinol 156(6):687–693. https://doi.org/10.1530/EJE-06-0702
Rexrode KM, Manson JE, Lee IM, Ridker PM, Sluss PM, Cook NR, Buring JE (2003) Sex hormone levels and risk of cardiovascular events in postmenopausal women. Circulation 108(14):1688–1693. https://doi.org/10.1161/01.CIR.0000091114.36254.F3
Meun C, Franco OH, Dhana K, Jaspers L, Muka T, Louwers Y, Ikram MA, Fauser B, Kavousi M, Laven JSE (2018) High androgens in postmenopausal women and the risk for atherosclerosis and cardiovascular disease: the Rotterdam study. J Clin Endocrinol Metab 103(4):1622-1630. https://doi.org/10.1210/jc.2017-02421
Rosano GM, Spoletini I, Vitale C (2017) Cardiovascular disease in women, is it different to men? The role of sex hormones. Climacteric 20(2):125–128. https://doi.org/10.1080/13697137.2017.1291780
Rosano GM, Leonardo F, Pagnotta P, Pelliccia F, Panina G, Cerquetani E, della Monica PL, Bonfigli B, Volpe M, Chierchia SL (1999) Acute anti-ischemic effect of testosterone in men with coronary artery disease. Circulation 99(13):1666–1670
White CM, Ferraro-Borgida MJ, Moyna NM, McGill CC, Ahlberg AW, Thompson PD, Chow MS, Heller GV (1998) The pharmacokinetics of intravenous testosterone in elderly men with coronary artery disease. J Clin Pharmacol 38(9):792–797
Webb CM, Adamson DL, de Zeigler D, Collins P (1999) Effect of acute testosterone on myocardial ischemia in men with coronary artery disease. Am J Cardiol 83(3):437–439 A439
Thompson PD, Ahlberg AW, Moyna NM, Duncan B, Ferraro-Borgida M, White CM, McGill CC, Heller GV (2002) Effect of intravenous testosterone on myocardial ischemia in men with coronary artery disease. Am Heart J 143(2):249–256
Jaffe MD (1977) Effect of testosterone cypionate on postexercise ST segment depression. Br Heart J 39(11):1217–1222
English KM, Steeds RP, Jones TH, Diver MJ, Channer KS (2000) Low-dose transdermal testosterone therapy improves angina threshold in men with chronic stable angina: a randomized, double-blind, placebo-controlled study. Circulation 102(16):1906–1911
Mathur A, Malkin C, Saeed B, Muthusamy R, Jones TH, Channer K (2009) Long-term benefits of testosterone replacement therapy on angina threshold and atheroma in men. Eur J Endocrinol 161(3):443–449. https://doi.org/10.1530/EJE-09-0092
Wu SZ, Weng XZ (1993) Therapeutic effects of an androgenic preparation on myocardial ischemia and cardiac function in 62 elderly male coronary heart disease patients. Chin Med J 106(6):415–418
Molinari C, Battaglia A, Grossini E, Mary DA, Vassanelli C, Vacca G (2002) The effect of testosterone on regional blood flow in prepubertal anaesthetized pigs. J Physiol 543(Pt 1):365–372
Perusquia M, Greenway CD, Perkins LM, Stallone JN (2015) Systemic hypotensive effects of testosterone are androgen structure-specific and neuronal nitric oxide synthase-dependent. Am J Physiol Regul Integr Comp Physiol 309(2):R189–R195. https://doi.org/10.1152/ajpregu.00110.2015
English KM, Jones RD, Jones TH, Morice AH, Channer KS (2000) Aging reduces the responsiveness of coronary arteries from male Wistar rats to the vasodilatory action of testosterone. Clin Sci 99(1):77–82
Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, de Ferranti S, Despres JP, Fullerton HJ, Howard VJ, Huffman MD, Judd SE, Kissela BM, Lackland DT, Lichtman JH, Lisabeth LD, Liu S, Mackey RH, Matchar DB, McGuire DK, Mohler ER 3rd, Moy CS, Muntner P, Mussolino ME, Nasir K, Neumar RW, Nichol G, Palaniappan L, Pandey DK, Reeves MJ, Rodriguez CJ, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Willey JZ, Woo D, Yeh RW, Turner MB, American Heart Association Statistics C, Stroke Statistics S (2015) Heart disease and stroke statistics—2015 update: a report from the American heart association. Circulation 131(4):e29–e322. https://doi.org/10.1161/CIR.0000000000000152
Moriyama Y, Yasue H, Yoshimura M, Mizuno Y, Nishiyama K, Tsunoda R, Kawano H, Kugiyama K, Ogawa H, Saito Y, Nakao K (2000) The plasma levels of dehydroepiandrosterone sulfate are decreased in patients with chronic heart failure in proportion to the severity. J Clin Endocrinol Metab 85(5):1834–1840. https://doi.org/10.1210/jcem.85.5.6568
Jankowska EA, Biel B, Majda J, Szklarska A, Lopuszanska M, Medras M, Anker SD, Banasiak W, Poole-Wilson PA, Ponikowski P (2006) Anabolic deficiency in men with chronic heart failure: prevalence and detrimental impact on survival. Circulation 114(17):1829–1837. https://doi.org/10.1161/CIRCULATIONAHA.106.649426
Kontoleon PE, Anastasiou-Nana MI, Papapetrou PD, Alexopoulos G, Ktenas V, Rapti AC, Tsagalou EP, Nanas JN (2003) Hormonal profile in patients with congestive heart failure. Int J Cardiol 87(2–3):179–183
Pugh PJ, Jones RD, West JN, Jones TH, Channer KS (2004) Testosterone treatment for men with chronic heart failure. Heart 90(4):446–447
Caminiti G, Volterrani M, Iellamo F, Marazzi G, Massaro R, Miceli M, Mammi C, Piepoli M, Fini M, Rosano GM (2009) Effect of long-acting testosterone treatment on functional exercise capacity, skeletal muscle performance, insulin resistance, and baroreflex sensitivity in elderly patients with chronic heart failure a double-blind, placebo-controlled, randomized study. J Am Coll Cardiol 54(10):919–927. https://doi.org/10.1016/j.jacc.2009.04.078
Malkin CJ, Pugh PJ, West JN, van Beek EJ, Jones TH, Channer KS (2006) Testosterone therapy in men with moderate severity heart failure: a double-blind randomized placebo controlled trial. Eur Heart J 27(1):57–64. https://doi.org/10.1093/eurheartj/ehi443
Pugh PJ, Jones TH, Channer KS (2003) Acute haemodynamic effects of testosterone in men with chronic heart failure. Eur Heart J 24(10):909–915
Iellamo F, Volterrani M, Caminiti G, Karam R, Massaro R, Fini M, Collins P, Rosano GM (2010) Testosterone therapy in women with chronic heart failure: a pilot double-blind, randomized, placebo-controlled study. J Am Coll Cardiol 56(16):1310–1316. https://doi.org/10.1016/j.jacc.2010.03.090
Stout M, Tew GA, Doll H, Zwierska I, Woodroofe N, Channer KS, Saxton JM (2012) Testosterone therapy during exercise rehabilitation in male patients with chronic heart failure who have low testosterone status: a double-blind randomized controlled feasibility study. Am Heart J 164(6):893–901. https://doi.org/10.1016/j.ahj.2012.09.016
Mirdamadi A, Garakyaraghi M, Pourmoghaddas A, Bahmani A, Mahmoudi H, Gharipour M (2014) Beneficial effects of testosterone therapy on functional capacity, cardiovascular parameters, and quality of life in patients with congestive heart failure. Biomed Res Int 2014:392432. https://doi.org/10.1155/2014/392432
Jankowska EA, Filippatos G, Ponikowska B, Borodulin-Nadzieja L, Anker SD, Banasiak W, Poole-Wilson PA, Ponikowski P (2009) Reduction in circulating testosterone relates to exercise capacity in men with chronic heart failure. J Card Fail 15(5):442–450. https://doi.org/10.1016/j.cardfail.2008.12.011
Wehr E, Pilz S, Boehm BO, Marz W, Grammer T, Obermayer-Pietsch B (2011) Low free testosterone is associated with heart failure mortality in older men referred for coronary angiography. Eur J Heart Fail 13(5):482–488. https://doi.org/10.1093/eurjhf/hfr007
Toma M, McAlister FA, Coglianese EE, Vidi V, Vasaiwala S, Bakal JA, Armstrong PW, Ezekowitz JA (2012) Testosterone supplementation in heart failure: a meta-analysis. Circ Heart Fail 5(3):315–321. https://doi.org/10.1161/CIRCHEARTFAILURE.111.965632
Dos Santos MR, Sayegh AL, Bacurau AV, Arap MA, Brum PC, Pereira RM, Takayama L, Barretto AC, Negrao CE, Alves MJ (2016) Effect of exercise training and testosterone replacement on skeletal muscle wasting in patients with heart failure with testosterone deficiency. Mayo Clin Proc 91(5):575–586. https://doi.org/10.1016/j.mayocp.2016.02.014
Sun J, Fu L, Tang X, Han Y, Ma D, Cao J, Kang N, Ji H (2011) Testosterone modulation of cardiac beta-adrenergic signals in a rat model of heart failure. Gen Comp Endocrinol 172(3):518–525. https://doi.org/10.1016/j.ygcen.2011.04.019
Kelly DM, Jones TH (2014) Testosterone and cardiovascular risk in men. Front Horm Res 43:1–20. https://doi.org/10.1159/000360553
Wehr E, Pilz S, Boehm BO, Grammer TB, Marz W, Obermayer-Pietsch B (2011) Low free testosterone levels are associated with all-cause and cardiovascular mortality in postmenopausal diabetic women. Diabetes Care 34(8):1771–1777. https://doi.org/10.2337/dc11-0596
Haring R, Teng Z, Xanthakis V, Coviello A, Sullivan L, Bhasin S, Murabito JM, Wallaschofski H, Vasan RS (2013) Association of sex steroids, gonadotrophins, and their trajectories with clinical cardiovascular disease and all-cause mortality in elderly men from the Framingham heart study. Clin Endocrinol 78(4):629–634. https://doi.org/10.1111/cen.12013
Khaw KT, Dowsett M, Folkerd E, Bingham S, Wareham N, Luben R, Welch A, Day N (2007) Endogenous testosterone and mortality due to all causes, cardiovascular disease, and cancer in men: European prospective investigation into cancer in Norfolk (EPIC-Norfolk) prospective population study. Circulation 116(23):2694–2701. https://doi.org/10.1161/CIRCULATIONAHA.107.719005
Laughlin GA, Barrett-Connor E, Bergstrom J (2008) Low serum testosterone and mortality in older men. J Clin Endocrinol Metab 93(1):68–75. https://doi.org/10.1210/jc.2007-1792
Tivesten A, Vandenput L, Labrie F, Karlsson MK, Ljunggren O, Mellstrom D, Ohlsson C (2009) Low serum testosterone and estradiol predict mortality in elderly men. J Clin Endocrinol Metab 94(7):2482–2488. https://doi.org/10.1210/jc.2008-2650
Araujo AB, Dixon JM, Suarez EA, Murad MH, Guey LT, Wittert GA (2011) Clinical review: endogenous testosterone and mortality in men: a systematic review and meta-analysis. J Clin Endocrinol Metab 96(10):3007–3019. https://doi.org/10.1210/jc.2011-1137
Corona G, Monami M, Boddi V, Cameron-Smith M, Fisher AD, de Vita G, Melani C, Balzi D, Sforza A, Forti G, Mannucci E, Maggi M (2010) Low testosterone is associated with an increased risk of MACE lethality in subjects with erectile dysfunction. J Sex Med 7(4 Pt 1):1557–1564. https://doi.org/10.1111/j.1743-6109.2009.01690.x
Malkin CJ, Pugh PJ, Morris PD, Asif S, Jones TH, Channer KS (2010) Low serum testosterone and increased mortality in men with coronary heart disease. Heart 96(22):1821–1825. https://doi.org/10.1136/hrt.2010.195412
Shores MM, Biggs ML, Arnold AM, Smith NL, Longstreth WT Jr, Kizer JR, Hirsch CH, Cappola AR, Matsumoto AM (2014) Testosterone, dihydrotestosterone, and incident cardiovascular disease and mortality in the cardiovascular health study. J Clin Endocrinol Metab 99(6):2061–2068. https://doi.org/10.1210/jc.2013-3576
Lehtonen A, Huupponen R, Tuomilehto J, Lavonius S, Arve S, Isoaho H, Huhtaniemi I, Tilvis R (2008) Serum testosterone but not leptin predicts mortality in elderly men. Age Ageing 37(4):461–464. https://doi.org/10.1093/ageing/afn048
Khurana KK, Navaneethan SD, Arrigain S, Schold JD, Nally JV Jr, Shoskes DA (2014) Serum testosterone levels and mortality in men with CKD stages 3-4. Am J Kidney Dis 64(3):367–374. https://doi.org/10.1053/j.ajkd.2014.03.010
Menke A, Guallar E, Rohrmann S, Nelson WG, Rifai N, Kanarek N, Feinleib M, Michos ED, Dobs A, Platz EA (2010) Sex steroid hormone concentrations and risk of death in US men. Am J Epidemiol 171(5):583–592. https://doi.org/10.1093/aje/kwp415
Militaru C, Donoiu I, Dracea O, Ionescu DD (2010) Serum testosterone and short-term mortality in men with acute myocardial infarction. Cardiol J 17(3):249–253
Ohlsson C, Labrie F, Barrett-Connor E, Karlsson MK, Ljunggren O, Vandenput L, Mellstrom D, Tivesten A (2010) Low serum levels of dehydroepiandrosterone sulfate predict all-cause and cardiovascular mortality in elderly Swedish men. J Clin Endocrinol Metab 95(9):4406–4414. https://doi.org/10.1210/jc.2010-0760
Carrero JJ, Qureshi AR, Parini P, Arver S, Lindholm B, Barany P, Heimburger O, Stenvinkel P (2009) Low serum testosterone increases mortality risk among male dialysis patients. J Am Soc Nephrol 20(3):613–620. https://doi.org/10.1681/ASN.2008060664
Vikan T, Schirmer H, Njolstad I, Svartberg J (2009) Endogenous sex hormones and the prospective association with cardiovascular disease and mortality in men: the Tromso study. Eur J Endocrinol 161(3):435–442. https://doi.org/10.1530/EJE-09-0284
Araujo AB, Kupelian V, Page ST, Handelsman DJ, Bremner WJ, McKinlay JB (2007) Sex steroids and all-cause and cause-specific mortality in men. Arch Intern Med 167(12):1252–1260. https://doi.org/10.1001/archinte.167.12.1252
Ponikowska B, Jankowska EA, Maj J, Wegrzynowska-Teodorczyk K, Biel B, Reczuch K, Borodulin-Nadzieja L, Banasiak W, Ponikowski P (2010) Gonadal and adrenal androgen deficiencies as independent predictors of increased cardiovascular mortality in men with type II diabetes mellitus and stable coronary artery disease. Int J Cardiol 143(3):343–348. https://doi.org/10.1016/j.ijcard.2009.03.072
Hyde Z, Norman PE, Flicker L, Hankey GJ, Almeida OP, McCaul KA, Chubb SA, Yeap BB (2012) Low free testosterone predicts mortality from cardiovascular disease but not other causes: the Health in men study. J Clin Endocrinol Metab 97(1):179–189. https://doi.org/10.1210/jc.2011-1617
Holmboe SA, Vradi E, Jensen TK, Linneberg A, Husemoen LL, Scheike T, Skakkebaek NE, Juul A, Andersson AM (2015) the association of reproductive hormone levels and all-cause, cancer, and cardiovascular disease mortality in men. J Clin Endocrinol Metab 100(12):4472–4480. https://doi.org/10.1210/jc.2015-2460
Hsu B, Cumming RG, Naganathan V, Blyth FM, Le Couteur DG, Hirani V, Waite LM, Seibel MJ, Handelsman DJ (2016) Temporal changes in androgens and estrogens are associated with all-cause and cause-specific mortality in older men. J Clin Endocrinol Metab 101(5):2201–2210. https://doi.org/10.1210/jc.2016-1025
Muraleedharan V, Marsh H, Kapoor D, Channer KS, Jones TH (2013) Testosterone deficiency is associated with increased risk of mortality and testosterone replacement improves survival in men with type 2 diabetes. Eur J Endocrinol 169(6):725–733. https://doi.org/10.1530/EJE-13-0321
Pye SR, Huhtaniemi IT, Finn JD, Lee DM, O’Neill TW, Tajar A, Bartfai G, Boonen S, Casanueva FF, Forti G, Giwercman A, Han TS, Kula K, Lean ME, Pendleton N, Punab M, Rutter MK, Vanderschueren D, Wu FC, Group ES (2014) Late-onset hypogonadism and mortality in aging men. J Clin Endocrinol Metab 99(4):1357–1366. https://doi.org/10.1210/jc.2013-2052
Hamilton EJ, Davis WA, Makepeace A, Lim EM, Yeap BB, Peters KE, Davis TM (2016) Prevalence and prognosis of a low serum testosterone in men with type 2 diabetes: the fremantle diabetes study phase II. Clin Endocrinol 85(3):444–452. https://doi.org/10.1111/cen.13087
Hackett G, Heald AH, Sinclair A, Jones PW, Strange RC, Ramachandran S (2016) Serum testosterone, testosterone replacement therapy and all-cause mortality in men with type 2 diabetes: retrospective consideration of the impact of PDE5 inhibitors and statins. Int J Clin Pract 70(3):244–253. https://doi.org/10.1111/ijcp.12779
Tint AN, Hoermann R, Wong H, Ekinci EI, MacIsaac RJ, Jerums G, Zajac JD, Grossmann M (2016) Association of sex hormone-binding globulin and free testosterone with mortality in men with type 2 diabetes mellitus. Eur J Endocrinol 174(1):59–68. https://doi.org/10.1530/EJE-15-0672
Daka B, Langer RD, Larsson CA, Rosen T, Jansson PA, Rastam L, Lindblad U (2015) Low concentrations of serum testosterone predict acute myocardial infarction in men with type 2 diabetes mellitus. BMC Endocr Disord 15:35. https://doi.org/10.1186/s12902-015-0034-1
Wu HY, Wang XF, Wang JH, Li JY (2011) Testosterone level and mortality in elderly men with systolic chronic heart failure. Asian J Androl 13(5):759–763. https://doi.org/10.1038/aja.2011.26
Shores MM, Smith NL, Forsberg CW, Anawalt BD, Matsumoto AM (2012) Testosterone treatment and mortality in men with low testosterone levels. J Clin Endocrinol Metab 97(6):2050–2058. https://doi.org/10.1210/jc.2011-2591
Yeap BB, Alfonso H, Chubb SA, Handelsman DJ, Hankey GJ, Almeida OP, Golledge J, Norman PE, Flicker L (2014) In older men an optimal plasma testosterone is associated with reduced all-cause mortality and higher dihydrotestosterone with reduced ischemic heart disease mortality, while estradiol levels do not predict mortality. J Clin Endocrinol Metab 99(1):E9–E18. https://doi.org/10.1210/jc.2013-3272
Yoshihisa A, Suzuki S, Sato Y, Kanno Y, Abe S, Miyata M, Sato T, Oikawa M, Kobayashi A, Yamaki T, Kunii H, Nakazato K, Ishida T, Takeishi Y (2018) Relation of testosterone levels to mortality in men with heart failure. Am J Cardiol 121(11):1321-1327. https://doi.org/10.1016/j.amjcard.2018.01.052
Haring R, Volzke H, Steveling A, Krebs A, Felix SB, Schofl C, Dorr M, Nauck M, Wallaschofski H (2010) Low serum testosterone levels are associated with increased risk of mortality in a population-based cohort of men aged 20-79. Eur Heart J 31(12):1494–1501. https://doi.org/10.1093/eurheartj/ehq009
Sharma R, Oni OA, Gupta K, Chen G, Sharma M, Dawn B, Sharma R, Parashara D, Savin VJ, Ambrose JA, Barua RS (2015) Normalization of testosterone level is associated with reduced incidence of myocardial infarction and mortality in men. Eur Heart J 36(40):2706–2715. https://doi.org/10.1093/eurheartj/ehv346
Shores MM, Matsumoto AM, Sloan KL, Kivlahan DR (2006) Low serum testosterone and mortality in male veterans. Arch Intern Med 166(15):1660–1665. https://doi.org/10.1001/archinte.166.15.1660
Maggio M, Lauretani F, Ceda GP, Bandinelli S, Ling SM, Metter EJ, Artoni A, Carassale L, Cazzato A, Ceresini G, Guralnik JM, Basaria S, Valenti G, Ferrucci L (2007) Relationship between low levels of anabolic hormones and 6-year mortality in older men: the aging in the Chianti area (InCHIANTI) study. Arch Intern Med 167(20):2249–2254. https://doi.org/10.1001/archinte.167.20.2249
Hackett GI (2016) Testosterone replacement therapy and mortality in older men. Drug Saf 39(2):117–130. https://doi.org/10.1007/s40264-015-0348-y
Alexander GC, Iyer G, Lucas E, Lin D, Singh S (2017) Cardiovascular risks of exogenous testosterone use among men: a systematic review and meta-analysis. Am J Med 130(3):293–305. https://doi.org/10.1016/j.amjmed.2016.09.017
Nahrendorf M, Frantz S, Hu K, von zur Muhlen C, Tomaszewski M, Scheuermann H, Kaiser R, Jazbutyte V, Beer S, Bauer W, Neubauer S, Ertl G, Allolio B, Callies F (2003) Effect of testosterone on post-myocardial infarction remodeling and function. Cardiovasc Res 57(2):370–378
Tan RS, Cook KR, Reilly WG (2015) Myocardial infarction and stroke risk in young healthy men treated with injectable testosterone. Int J Endocrinol 2015:970750. https://doi.org/10.1155/2015/970750
Baillargeon J, Urban RJ, Kuo YF, Ottenbacher KJ, Raji MA, Du F, Lin YL, Goodwin JS (2014) Risk of myocardial infarction in older men receiving testosterone therapy. Ann Pharmacother 48(9):1138–1144. https://doi.org/10.1177/1060028014539918
Morgentaler A, Miner MM, Caliber M, Guay AT, Khera M, Traish AM (2015) Testosterone therapy and cardiovascular risk: advances and controversies. Mayo Clin Proc 90(2):224–251. https://doi.org/10.1016/j.mayocp.2014.10.011
Eisenberg ML, Li S, Herder D, Lamb DJ, Lipshultz LI (2015) Testosterone therapy and mortality risk. Int J Impot Res 27(2):46–48. https://doi.org/10.1038/ijir.2014.29
Yeap BB, Alfonso H, Chubb SA, Hankey GJ, Handelsman DJ, Golledge J, Almeida OP, Flicker L, Norman PE (2014) In older men, higher plasma testosterone or dihydrotestosterone is an independent predictor for reduced incidence of stroke but not myocardial infarction. J Clin Endocrinol Metab 99(12):4565–4573. https://doi.org/10.1210/jc.2014-2664
Xu L, Freeman G, Cowling BJ, Schooling CM (2013) Testosterone therapy and cardiovascular events among men: a systematic review and meta-analysis of placebo-controlled randomized trials. BMC Med 11:108. https://doi.org/10.1186/1741-7015-11-108
Finkle WD, Greenland S, Ridgeway GK, Adams JL, Frasco MA, Cook MB, Fraumeni JF Jr, Hoover RN (2014) Increased risk of non-fatal myocardial infarction following testosterone therapy prescription in men. PLoS One 9(1):e85805. https://doi.org/10.1371/journal.pone.0085805
Shores MM, Matsumoto AM (2014) Testosterone, aging and survival: biomarker or deficiency. Curr Opin Endocrinol Diabetes Obes 21(3):209–216. https://doi.org/10.1097/MED.0000000000000057
Schooling CM (2014) Testosterone and cardiovascular disease. Curr Opin Endocrinol Diabetes Obes 21(3):202–208. https://doi.org/10.1097/MED.0000000000000065
Vigen R, O’Donnell CI, Baron AE, Grunwald GK, Maddox TM, Bradley SM, Barqawi A, Woning G, Wierman ME, Plomondon ME, Rumsfeld JS, Ho PM (2013) Association of testosterone therapy with mortality, myocardial infarction, and stroke in men with low testosterone levels. JAMA 310(17):1829–1836. https://doi.org/10.1001/jama.2013.280386
Tam LM, Kim J, Blumenthal RS, Nasir K, Al-Mallah MH, Blaha MJ (2013) Absolute coronary artery calcium score is the best predictor of non-calcified plaque involvement in patients with low calcium scores (1-100). Atherosclerosis 230(1):76–79. https://doi.org/10.1016/j.atherosclerosis.2013.06.022
Lai J, Ge Y, Shao Y, Xuan T, Xia S, Li M (2015) Low serum testosterone level was associated with extensive coronary artery calcification in elderly male patients with stable coronary artery disease. Coron Artery Dis 26(5):437–441. https://doi.org/10.1097/MCA.0000000000000260
Park BJ, Shim JY, Lee YJ, Lee JH, Lee HR (2012) Inverse relationship between bioavailable testosterone and subclinical coronary artery calcification in non-obese Korean men. Asian J Androl 14(4):612–615. https://doi.org/10.1038/aja.2012.19
Ahmadi A, Stone GW, Leipsic J, Shaw LJ, Villines TC, Kern MJ, Hecht H, Erlinge D, Ben-Yehuda O, Maehara A, Arbustini E, Serruys P, Garcia-Garcia HM, Narula J (2016) Prognostic determinants of coronary atherosclerosis in stable ischemic heart disease: anatomy, physiology, or morphology? Circ Res 119(2):317–329. https://doi.org/10.1161/CIRCRESAHA.116.308952
Snyder PJ, Bhasin S, Cunningham GR, Matsumoto AM, Stephens-Shields AJ, Cauley JA, Gill TM, Barrett-Connor E, Swerdloff RS, Wang C, Ensrud KE, Lewis CE, Farrar JT, Cella D, Rosen RC, Pahor M, Crandall JP, Molitch ME, Cifelli D, Dougar D, Fluharty L, Resnick SM, Storer TW, Anton S, Basaria S, Diem SJ, Hou X, Mohler ER 3rd, Parsons JK, Wenger NK, Zeldow B, Landis JR, Ellenberg SS, Testosterone Trials I (2016) Effects of testosterone treatment in older men. N Engl J Med 374(7):611–624. https://doi.org/10.1056/NEJMoa1506119
Gianatti EJ, Hoermann R, Lam Q, Dupuis P, Zajac JD, Grossmann M (2015) Effect of testosterone treatment on cardiac biomarkers in a randomized controlled trial of men with type 2 diabetes. Clin Endocrinol 84(1):55-62. https://doi.org/10.1111/cen.12842
Ruige JB, Ouwens DM, Kaufman JM (2013) Beneficial and adverse effects of testosterone on the cardiovascular system in men. J Clin Endocrinol Metab 98(11):4300–4310. https://doi.org/10.1210/jc.2013-1970
Pereira TV, Ioannidis JP (2011) Statistically significant meta-analyses of clinical trials have modest credibility and inflated effects. J Clin Epidemiol 64(10):1060–1069. https://doi.org/10.1016/j.jclinepi.2010.12.012
Maki-Nunes C, Toschi-Dias E, Cepeda FX, Rondon MU, Alves MJ, Fraga RF, Braga AM, Aguilar AM, Amaro AC, Drager LF, Lorenzi-Filho G, Negrao CE, Trombetta IC (2015) Diet and exercise improve chemoreflex sensitivity in patients with metabolic syndrome and obstructive sleep apnea. Obesity (Silver Spring) 23(8):1582–1590. https://doi.org/10.1002/oby.21126
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bianchi, V.E. Testosterone, myocardial function, and mortality. Heart Fail Rev 23, 773–788 (2018). https://doi.org/10.1007/s10741-018-9721-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10741-018-9721-0