Abstract
We carry out computational simulations of the Valsalva compression of an inferior vena cava (IVC) with a filter implanted in it. We find that when we treat the IVC wall as simply a boundary between 2 fluids and apply an external pressure on the IVC, the deformation magnitudes and patterns do not agree with data in the literature. We conclude that IVC compression is mainly caused by solid bodies (i.e. tissue and organs) compressing the IVC, and develop a model to simulate this phenomenon. We calibrate our model to data in the literature for Valsalva compression with and without an implanted filter. We then use our approach to predict the area reduction of the IVC during breathing when 2 different types of filters are implanted. Not surprisingly, we find that a compliant filter is less able to resist the compression of the IVC during respiration than a stiffer one, and we quantify the difference. We anticipate that, with further development, our model can be used to make assessments of design and testing parameters that can help to avoid fatigue failure of a filter that is subjected to millions of compressions due to breathing.














Similar content being viewed by others
References
Netter, F.H.: Atlas of Human Anatomy. Elsevier, Amsterdam (2019)
Greenfield, L.J., Zocco, J., Wilk, J., Schroeder, T.M., Elkins, R.C.: Clinical experience with the Kim-Ray Greenfield vena caval filter. Ann. Surg. 185, 692–698 (1977). https://doi.org/10.1097/00000658-197706000-00012
Grassi, C.J.: Inferior vena caval filters: analysis of five currently available devices. Am. J. Roentgenol. 156, 813–821 (1991)
Neuerburg, J., Günther, R.W., Rassmussen, E., Vorwerk, D., Tonn, K., Handt, S., Küpper, W., Hansen, J.V.: New retrievable percutaneous vena cava filter: experimental in vitro and in vivo evaluation. Cardiovasc. Interv. Radiol. 16, 224–229 (1993). https://doi.org/10.1007/BF02602965
Deso, S.E., Idakoji, I.A., Kuo, W.T.: Evidence-based evaluation of inferior vena cava filter complications based on filter type. Semin. Intervent. Radiol. 33, 93–100 (2016). https://doi.org/10.1055/s-0036-1583208
Grant, E., Rendano, F., Sevinc, E., Gammelgaard, J., Holm, H., Grovall, S.: Normal inferior vena cava: Caliber changes observed by dynamic ultrasound. Am. J. Roentgenol. 135, 335–338 (1980)
Murphy, E.H., Johnson, E.D., Arko, F.R.: Evaluation of wall motion and dynamic geometry of the inferior vena cava using intravascular ultrasound: implications for future device design. J. Endovasc. Ther. 15, 349–355 (2008). https://doi.org/10.1583/08-2424.1
Klabunde, R.E.: Cardiovascular Physiology Concepts, 2nd edn. LWW, Philadelphia (2011)
Tibbs, D.J.: Varicose Veins and Related Disorders. Butterworth-Heinemann, Stoneham (1991)
Uva, B., Aliverti, A., Bovio, D., Kayser, B.: The “abdominal circulatory pump”: an auxiliary heart during exercise? Front. Physiol. 6, 1–12 (2016). https://doi.org/10.3389/fphys.2015.00411
LoMauro, A., Aliverti, A.: Blood shift during cough: negligible or significant? Front. Physiol. 9, 1–7 (2018). https://doi.org/10.3389/fphys.2018.00501
De Gregorio, M.A., Gamboa, P., Bonilla, D.L., Sanchez, M., Higuera, M.T., Medrano, J., Mainar, A., Lostalé, F., Laborda, A.: Retrieval of Günther Tulip optional vena cava filters 30 days after implantation: a prospective clinical study. J. Vasc. Interv. Radiol. 17, 1781–1789 (2006). https://doi.org/10.1097/01.RVI.0000244837.46324.72
Blehar, D.J., Resop, D., Chin, B., Dayno, M., Gaspari, R.: Inferior vena cava displacement during respirophasic ultrasound imaging. Crit. Ultrasound J. 4, 1–5 (2012). https://doi.org/10.1186/2036-7902-4-18
Pstras, L., Thomaseth, K., Waniewski, J., Balzani, I., Bellavere, F.: The Valsalva manoeuvre: physiology and clinical examples. Acta Physiol. 217, 103–119 (2016). https://doi.org/10.1111/apha.12639
Laborda, A., Sierra, S., Malve, M., De Blas, I., Ioakeim, I., Kuo, W.T., De Gregorio, M.A.: Influence of breathing movements and Valsalva maneuver on vena caval dynamics. World J. Radiol. 6, 833–839 (2014). https://doi.org/10.4329/wjr.v6.i10.833
Laborda, A., Kuo, W.T., Ioakeim, I., De Blas, I., Malvè, M., Lahuerta, C., De Gregorio, M.A.: Respiratory-induced haemodynamic changes: a contributing factor to IVC filter penetration. Cardiovasc. Interv. Radiol. 38, 1192–1197 (2015). https://doi.org/10.1007/s00270-015-1077-4
Joseph, A.A., Voit, D., Frahm, J.: Inferior vena cava revisited – real-time flow MRI of respiratory maneuvers. NMR Biomed. 33, 1–8 (2020). https://doi.org/10.1002/nbm.4232
Kalva, S.P., Wicky, S., Waltman, A.C., Athanasoulis, C.A.: TrapEase vena cava filter: experience in 751 patients. J. Endovasc. Ther. 13, 365–372 (2006). https://doi.org/10.1583/05-1741.1
Johnson, M.S., Nemcek, A.A. Jr., Benenati, J.F., Baumann, D.S., Dolmatch, B.L., Kaufman, J.A., Garcia, M.J., Stecker, M.S., Venbrux, A.C., Haskal, Z.J., Avelar, R.L.: The safety and effectiveness of the retrievable Option inferior vena cava filter: a United States prospective multicenter clinical study. J. Vasc. Interv. Radiol. 21, 1173–1184 (2010). https://doi.org/10.1016/j.jvir.2010.04.004
Stavropoulos, S.W., Sing, R.F., Elmasri, F., Silver, M.J., Powell, A., Lynch, F.C., Aal, A.K.A., Lansky, A.J., Settlage, R.A., Muhs, B.E.: The Denali trial: an interim analysis of a prospective, multicenter study of the Denali retrievable inferior vena cava filter. J. Vasc. Interv. Radiol. 25, 1497–1505.e1 (2014). https://doi.org/10.1016/j.jvir.2014.07.001
Smouse, H.B., Rosenthal, D., Van Ha, T., Knox, M.F., Dixon, R.G., Voorhees, W.D., McCann-Brown, J.A.: Long-term retrieval success rate profile for the Günther Tulip vena cava filter. J. Vasc. Interv. Radiol. 20, 871–877 (2009). https://doi.org/10.1016/j.jvir.2009.03.033
Le Blanche, A.F., Benazzouz, A., Reynaud, P., Fernandez, R.O., Emanuelli, G., Ricco, J.B., Delcour, C.: The VenaTech LP permanent caval filter: effectiveness and safety in the prevention of pulmonary embolism-a European multicenter study. J. Vasc. Interv. Radiol. 19, 509–515 (2008). https://doi.org/10.1016/j.jvir.2007.11.024
Lyon, S.M., Riojas, G.E., Uberoi, R., Patel, J., Lipp, M.E.B., Plant, G.R., De Gregorio, M.A., Günther, R.W., Voorhees, W.D., McCann-Brown, J.A.: Short- and long-term retrievability of the Celect vena cava filter: results from a multi-institutional registry. J. Vasc. Interv. Radiol. 20, 1441–1448 (2009). https://doi.org/10.1016/j.jvir.2009.07.038
Roehm, J.O.F.: The bird’s nest filter: a new percutaneous transcatheter inferior vena cava filter. J. Vasc. Surg. 1, 498–501 (1984). https://doi.org/10.1016/0741-5214(84)90092-2
Robertson, S.W., Pelton, A.R., Ritchie, R.O.: Mechanical fatigue and fracture of Nitinol. Int. Mater. Rev. 57, 1–36 (2012). https://doi.org/10.1179/1743280411Y.0000000009
Schmidt, P.A., Blair, R.R., Earthman, J.C.: Development of a novel specimen geometry for fatigue testing of fine wire. J. Test. Eval. 23, 73–79 (1995). https://doi.org/10.1520/jte10897j
Kobayashi, E., Mochizuki, H., Doi, H., Yoneyama, T., Hanawa, T.: Fatigue life prediction of biomedical titanium alloys under tensile/torsional stress. Mater. Trans. 47, 1826–1831 (2006). https://doi.org/10.2320/matertrans.47.1826
Huang, J.Y., Yen, J.J., Jeng, S.L., Chen, C.Y., Kuo, R.C.: High-cycle fatigue behavior of type 316L stainless steel. Mater. Trans. 47, 409–417 (2006). https://doi.org/10.2320/matertrans.47.409
Hull, J.E., Robertson, S.W.: Bard Recovery filter: evaluation and management of vena cava limb perforation, fracture, and migration. J. Vasc. Interv. Radiol. 20, 52–60 (2009). https://doi.org/10.1016/j.jvir.2008.09.032
Kuo, W.T., Robertson, S.W., Odegaard, J.I., Hofmann, L.V.: Complex retrieval of fractured, embedded, and penetrating inferior vena cava filters: a prospective study with histologic and electron microscopic analysis. J. Vasc. Interv. Radiol. 24, 622–630.e1 (2013). https://doi.org/10.1016/j.jvir.2013.01.008
Birring, S.S., Matos, S., Patel, R.B., Prudon, B., Evans, D.H., Pavord, I.D.: Cough frequency, cough sensitivity and health status in patients with chronic cough. Respir. Med. 100, 1105–1109 (2006). https://doi.org/10.1016/j.rmed.2005.09.023
McGrath, D.J., Thiebes, A.L., Cornelissen, C.G., O’Brien, B., Jockenhoevel, S., Bruzzi, M., McHugh, P.E.: Evaluating the interaction of a tracheobronchial stent in an ovine in-vivo model. Biomech. Model. Mechanobiol. 17, 499–516 (2018). https://doi.org/10.1007/s10237-017-0974-7
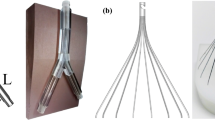
Special 510(k): Device Modification, K121057, Günther Tulip Vena Cava Filter Sets and Cook Celect Vena Cava Filter Sets, Cook Medical–William Cook Europe ApS (2012)
Nicolás, M., Lucea, B., Laborda, A., Peña, E., De Gregorio, M.A., Martínez, M.A., Malvè, M.: Influence of a commercial antithrombotic filter on the caval blood flow during neutra and Valsalva maneuver. J. Med. Devices, Trans. ASME. 11, 1–11 (2017). https://doi.org/10.1115/1.4035983
Aycock, K.I., Campbell, R.L., Manning, K.B., Sastry, S.P., Shontz, S.M., Lynch, F.C., Craven, B.A.: A computational method for predicting inferior vena cava filter performance on a patient-specific basis. J. Biomech. Eng. 136, 1–14 (2014). https://doi.org/10.1115/1.4027612
Pérez-Andrés, A., Peña, E.: Calibration of interface properties and application to a finite element model for predicting vena cava filter–induced vein wall failure. Int. J. Numer. Methods Biomed. Eng. 34, 1–13 (2018). https://doi.org/10.1002/cnm.3098
Ogden, R.W.: Large deformation isotropic elasticity – on the correlation of theory and experiment for incompressible rubberlike solids. Proc. R. Soc. Lond. Ser. A, Math. Phys. Sci. 326, 565–584 (1972). https://doi.org/10.1098/rspa.1972.0026
Dassault Systèmes: Abaqus version 2019, Providence RI (2019)
Anonymous: Cobalt Monograph. Brussels: Centre d’information du cobalt (1960)
García, A., Lerga, S., Peña, E., Malve, M., Laborda, A., De Gregorio, M.A., Martínez, M.A.: Evaluation of migration forces of a retrievable filter: experimental setup and finite element study. Med. Eng. Phys. 34, 1167–1176 (2012). https://doi.org/10.1016/j.medengphy.2011.12.005
Kapila, S., Sachdeva, R.: Mechanical properties and clinical applications of orthodontic wires. Am. J. Orthod. Dentofac. Orthop. 96, 100–109 (1989). https://doi.org/10.1016/0889-5406(89)90251-5
Assefpour-Dezfuly, M., Bonfield, W.: Microplasticity in Elgiloy. J. Mater. Sci. 20, 3018–3026 (1985). https://doi.org/10.1007/BF00553068
Dowell, J.D., Castle, J.C., Schickel, M., Andersson, U.K., Zielinski, R., McLoney, E., Guy, G., Yang, X., Ghadiali, S.: Celect inferior vena cava wall strut perforation begets additional strut perforation. J. Vasc. Interv. Radiol. 26, 1510–1518.e3 (2015). https://doi.org/10.1016/j.jvir.2015.06.020
Aycock, K.I., Campbell, R.L., Lynch, F.C., Manning, K.B., Craven, B.A.: The importance of hemorheology and patient anatomy on the hemodynamics in the inferior vena cava. Ann. Biomed. Eng. 44, 3568–3582 (2016). https://doi.org/10.1007/s10439-016-1663-x
Dunn, A.C., Zaveri, T.D., Keselowsky, B.G., Sawyer, W.G.: Macroscopic friction coefficient measurements on living endothelial cells. Tribol. Lett. 27, 233–238 (2007). https://doi.org/10.1007/s11249-007-9230-0
Mummert, J., Sirois, E., Sun, W.: Quantification of biomechanical interaction of transcatheter aortic valve stent deployed in porcine and ovine hearts. Ann. Biomed. Eng. 41, 577–586 (2013). https://doi.org/10.1007/s10439-012-0694-1
McGee, O.M., Sun, W., McNamara, L.M.: An in vitro model quantifying the effect of calcification on the tissue–stent interaction in a stenosed aortic root. J. Biomech. 82, 109–115 (2019). https://doi.org/10.1016/j.jbiomech.2018.10.010
Fung, Y.C.: Biomechanics. Springer, Berlin (1993)
Shi, Y., Glaser, K.J., Venkatesh, S.K., Ben-Abraham, E.I., Ehman, R.L.: Feasibility of using 3D MR elastography to determine pancreatic stiffness in healthy volunteers. J. Magn. Reson. Imaging 41, 369–375 (2015). https://doi.org/10.1002/jmri.24572
Patel, P.N., Smith, C.K., Patrick, C.W.: Rheological and recovery properties of poly(ethylene glycol) diacrylate hydrogels and human adipose tissue. J. Biomed. Mater. Res., Part A 73, 313–319 (2005). https://doi.org/10.1002/jbm.a.30291
Ogneva, I.V., Ushakov, I.B.: The transversal stiffness of skeletal muscle fibers and cardiomyocytes in control and after simulated microgravity. In: Frewin, C. (ed.) At. Force Microsc. Investig. into Biol. – From Cell to Protein, pp. 325–354 (2012). https://doi.org/10.5772/36457
Auricchio, F., Taylor, R.L.: Shape-memory alloys: modelling and numerical simulations of the finite-strain superelastic behavior. Comput. Methods Appl. Mech. Eng. 143, 175–194 (1997)
Auricchio, F., Taylor, R.L., Lubliner, J.: Shape-memory alloys: macromodelling and numerical simulations of the superelastic behavior. Comput. Methods Appl. Mech. Eng. 146, 281–312 (1997)
Cao, H., Wu, M.H., Zhou, F., McMeeking, R.M., Ritchie, R.O.: The influence of mean strain on the high-cycle fatigue of Nitinol with application to medical devices. J. Mech. Phys. Solids 143, 104057 (2020). https://doi.org/10.1016/j.jmps.2020.104057
Kossa, A., McMeeking, R.M.: Bending of a Nitinol cantilever and its fatigue performance. Extrem. Mech. Lett. 42, 101083 (2021). https://doi.org/10.1016/j.eml.2020.101083
Author information
Authors and Affiliations
Ethics declarations
Financial interests
Attila Kossa has given paid expert testimony on finite element analysis of inferior vena cava filters. Robert McMeeking is a consultant to medical implant companies on issues relating to the durability and reliability of medical implants. Robert McMeeking has given paid expert testimony on stress and strain analysis and the reliability and durability of inferior vena cava filters.
Additional information
Dedicated to Gerhard Holzapfel on the occasion of his 60th birthday. In admiration of his many significant contributions to solid mechanics and his leadership of and profound influence on biomechanics and bioengineering. Also, in friendship.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix A: Mesh Dependency Analyses
The simulation depicted in Fig. 8 is carried out using different meshes for the leg. Five different mesh densities are analyzed. In the coarsest mesh, the global seed size is 4 mm, whereas in the finest case we use a 0.25 mm global seed size. Table 3 contains the number of elements for the primary leg and for the secondary leg. Labels M1 … M5 indicate specific meshes.
We analyze the effect of the mesh density on the applied force and the maximum Mises stress in the leg corresponding to a 10 mm displacement of the rigid wall in Fig. 8. We use the linear elastic materials properties of Conichrome. Figure 15 shows the effect of mesh density on the applied force for both the primary and secondary legs, whereas Fig. 16 presents the variation of the maximum Mises stress versus the global seed size. The maximum Mises stress is located in the cross-section at the fixed end of the legs. As can be seen from the figures, the mesh density does not have a significant effect on the results, an outcome that arises from our use of quadratic beam elements. However, we note that the mesh density can have an effect on the contact formulation, but we see that this is also negligible in this case. The maximum Mises stress is almost identical for both the primary and the secondary legs. The secondary leg has a different shape and a smaller cross-section when compared with the primary leg. Thus, it is coincidental that the maximum Mises stress magnitudes in the 2 legs are almost identical. For the simulations utilized for our results, we have chosen the mesh designated M3, with a global seed size of 1 mm.
The effect of the mesh density was also analyzed for the IVC wall. Figure 17 shows a schematic of the configuration used for this mesh dependency analysis. An oval IVC in its undeformed configuration is shown in grey. Two circular rigid cylinders are used to deform the IVC. The deformed configuration is depicted in black in Fig. 17. A vertical displacement \(u=7\text{ mm}\) of the rigid cylinder is prescribed for the calculation. Due to symmetry, we analyze only one quarter of the configuration. Eight-node biquadratic plane strain quadrilateral elements with hybrid formulation are used with uniform thickness of 1 mm. Ten different mesh densities are analyzed. In the coarse case (M1), the global seed size is 1 mm, whereas the finest mesh (M5) contains element having a 0.1 mm global seed size. The details of the meshes are listed in Table 4, whereas Fig. 18 shows three examples of meshes for the purposes of illustration.
As indicators we compute the reaction force at the circular cylinder and the horizontal displacement, \(t\), of the inner point of the IVC wall on the horizontal axis (see Fig. 17). The results are shown in Fig. 19 for the reaction force and in Fig. 20 for the horizontal displacement of the point on the inner surface of the IVC wall. Only the results for meshes M1, M5 and M10 are shown in the plots; the results for the other meshes are bracketed by the curves corresponding to meshes M1 and M10. Very minor differences can be seen among the results. Based on this study we use the mesh M5 in our other computations.
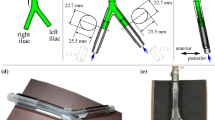
Appendix B: Effect of the Larger Radial Displacement on the Stiffness Values of the Legs
Before implantation, a filter is compressed to fit within a catheter or sheath of narrow diameter that is then passed through the vasculature to position the filter at the desired location within the IVC, usually the infrarenal position. This process involves significant deformation of the filter legs that might lead to permanent deformation or phase transition in the material. Our computational model for the Valsalva maneuver and for normal breathing neglects these deformations as we used only linear elastic behavior for the filter legs. In this appendix, we demonstrate that this is an acceptable approach for the analysis.
We repeat the calculation shown in Fig. 8 but with the following loading history: i) In the 1st step, the leg is compressed radially by the rigid wall until it is 1 mm above the fixed end of the leg. This configuration simulates a filter confined in a sheath or catheter with a representative value of 2 mm for the sheath inner diameter. ii) In the second step, the rigid wall is raised and the leg is allowed to relax back to a configuration, where the rigid wall is 8 mm above the fixed end of the leg. This configuration represents a filter implanted in the IVC. iii) Finally, in the third step, the leg is compressed radially again by the rigid wall being brought down again until it is 6 mm above the fixed end of the leg.
For the legs of a Celect filter we use a linear elastic – perfectly plastic material model with yield stress of 1.93 GPa according to [39, 41]. The legs of the alternative Nitinol filter with the same shape as a Celect filter is modelled using the fitted superelastic material model, with parameters given in Table 1 [54].
The resulting forces applied by the legs to the rigid wall during the entire loading are shown in Fig. 21-Fig. 24, where the radial coordinate is defined as the vertical distance of the rigid wall from the fixed end of the leg in Fig. 8.
Celect filter: The stress in the secondary leg remains below the yield stress and, therefore, the material deforms pure elastically. The loading-unloading-reloading curves are on the same curve in the plot (Fig. 21). The stress in the primary leg reaches the yield stress of the material and, therefore, plastic deformation initiates. However, the resulting permanent deformation is minor and, therefore, only a small amount of hysteresis is visible in the force-displacement plot in Fig. 22. The slope of the curve in the re-loading phase is practically the same as during initial loading. Thus, the deformations of the legs during a Valsalva maneuver and during normal breathing are in the range where only elastic deformation occurs. We note also that we include no work hardening during plastic deformation. Including work hardening during yielding would reduce the hysteresis in the plot.
Alternative Nitinol Filter: A very tiny amount of hysteresis can be seen in the force result for the secondary leg (Fig. 23). This implies that phase transformation occurred during the loading, but had negligible effect on the stiffness of the leg. The primary leg experiences much more phase transformation, as can be seen clearly in Fig. 24. It can be seen that the prior phase transformation that the leg has experienced reduces the radial force applied by the leg to the IVC wall by a small amount in the radial coordinate range from 6 mm to 8 mm compared to that prevailing during the loading phase prior to the martensitic phase transformation. However, it is important to emphasize that in the reloading phase the prior transformation has little effect and the stiffness of the leg is then nearly identical to the stiffness prevailing during initial loading. Similar to the Celect filter, the deformations of the legs during a Valsalva maneuver and during normal breathing are in the range where only linear elastic deformation occurs.
Therefore, the significant deformation that occurs during delivery of these 2 filters in a sheath or catheter, given their mechanical properties, has no major effect thereafter on the stiffness of the filters in the range of deformations corresponding to a Valsalva maneuver and normal breathing. From this we conclude that neglecting nonlinear material behavior during our study of the interaction of the filter with the IVC and surrounding tissue and organs is an appropriate approach.
Rights and permissions
About this article
Cite this article
Kossa, A., McMeeking, R.M. The Effect of an Implanted Filter on Valsalva-Compression and Respiratory-Compression of the Inferior Vena Cava. J Elast 145, 383–408 (2021). https://doi.org/10.1007/s10659-021-09850-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10659-021-09850-8