Abstract
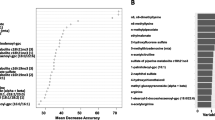
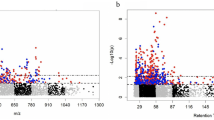
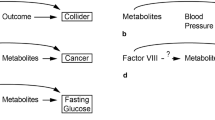
There is growing interest in incorporating metabolomics into public health practice. However, Black women are under-represented in many metabolomics studies. If metabolomic profiles differ between Black and White women, this under-representation may exacerbate existing Black-White health disparities. We therefore aimed to estimate metabolomic differences between Black and White women in the U.S. We leveraged data from two prospective cohorts: the Nurses’ Health Study (NHS; n = 2077) and Women’s Health Initiative (WHI; n = 2128). The WHI served as the replication cohort. Plasma metabolites (n = 334) were measured via liquid chromatography-tandem mass spectrometry. Observed metabolomic differences were estimated using linear regression and metabolite set enrichment analyses. Residual metabolomic differences in a hypothetical population in which the distributions of 14 risk factors were equalized across racial groups were estimated using inverse odds ratio weighting. In the NHS, Black-White differences were observed for most metabolites (75 metabolites with observed differences \(\ge \)|0.50| standard deviations). Black women had lower average levels than White women for most metabolites (e.g., for N6, N6-dimethlylysine, mean Black-White difference = − 0.98 standard deviations; 95% CI: − 1.11, − 0.84). In metabolite set enrichment analyses, Black women had lower levels of triglycerides, phosphatidylcholines, lysophosphatidylethanolamines, phosphatidylethanolamines, and organoheterocyclic compounds, but higher levels of phosphatidylethanolamine plasmalogens, phosphatidylcholine plasmalogens, cholesteryl esters, and carnitines. In a hypothetical population in which distributions of 14 risk factors were equalized, Black-White metabolomic differences persisted. Most results replicated in the WHI (88% of 272 metabolites available for replication). Substantial differences in metabolomic profiles exist between Black and White women. Future studies should prioritize racial representation.


Similar content being viewed by others
Data availability
Due to participant confidentiality and privacy concerns, requests to access the NHS and WHI data must be submitted in writing and must comply with the data request procedures of the NHS and WHI. Investigators wishing to use NHS data are asked to submit a brief description of the proposed project. Go to https://www.nurseshealthstudy.org/researchers (contact email: nhsaccess@channing.harvard.edu) for more details on accessing the NHS data. To request use of the WHI data, go to https://www.whi.org/get-started. Statistical code used in this manuscript is publicly available via GitHub: https://github.com/emma-mcgee/racial-differences-in-metabolomic-profiles
References
Nicholson JK, Lindon JC. Systems biology: metabonomics. Nature. 2008;455(7216):1054–6. https://doi.org/10.1038/4551054a.
Collins FS, Varmus H. A new initiative on precision medicine. N Engl J Med. 2015;372(9):793–5. https://doi.org/10.1056/NEJMp1500523.
Beger RD, Dunn W, Schmidt MA, et al. Metabolomics enables precision medicine: “a white paper, community perspective.” Metabolomics. 2016;12(9):149. https://doi.org/10.1007/s11306-016-1094-6.
Cruz DE, Tahir UA, Hu J, et al. Metabolomic analysis of coronary heart disease in an African American cohort from the Jackson Heart Study. JAMA Cardiol. 2022;7(2):184–94. https://doi.org/10.1001/jamacardio.2021.4925.
Li J, Guasch-Ferré M, Chung W, et al. The mediterranean diet, plasma metabolome, and cardiovascular disease risk. Eur Heart J. 2020;41(28):2645–56. https://doi.org/10.1093/eurheartj/ehaa209.
Cavus E, Karakas M, Ojeda FM, et al. Association of circulating metabolites with risk of coronary heart disease in a European population: results from the Biomarkers for Cardiovascular Risk Assessment in Europe (BiomarCaRE) Consortium. JAMA Cardiol. 2019;4(12):1270–9. https://doi.org/10.1001/jamacardio.2019.4130.
Paynter NP, Balasubramanian R, Giulianini F, et al. Metabolic predictors of incident coronary heart disease in women. Circulation. 2018;137(8):841–53. https://doi.org/10.1161/CIRCULATIONAHA.117.029468.
Ruiz-Canela M, Hruby A, Clish CB, Liang L, Martínez-González MA, Hu FB. Comprehensive metabolomic profiling and incident cardiovascular disease: a systematic review. J Am Heart Assoc. 2017. https://doi.org/10.1161/JAHA.117.005705.
Würtz P, Havulinna AS, Soininen P, et al. Metabolite profiling and cardiovascular event risk: a prospective study of 3 population-based cohorts. Circulation. 2015;131(9):774–85. https://doi.org/10.1161/CIRCULATIONAHA.114.013116.
Zeleznik OA, Clish CB, Kraft P, Avila-Pacheco J, Eliassen AH, Tworoger SS. Circulating lysophosphatidylcholines, phosphatidylcholines, ceramides, and sphingomyelins and ovarian cancer risk: a 23-year prospective study. J Natl Cancer Inst. 2019;112(6):628–36. https://doi.org/10.1093/jnci/djz195.
Moore SC, Playdon MC, Sampson JN, et al. A metabolomics analysis of body mass index and postmenopausal breast cancer risk. J Natl Cancer Inst. 2018;110(6):588–97. https://doi.org/10.1093/jnci/djx244.
Kühn T, Floegel A, Sookthai D, et al. Higher plasma levels of lysophosphatidylcholine 18:0 are related to a lower risk of common cancers in a prospective metabolomics study. BMC Med. 2016;14:13. https://doi.org/10.1186/s12916-016-0552-3.
Huang J, Mondul AM, Weinstein SJ, et al. Serum metabolomic profiling of prostate cancer risk in the prostate, lung, colorectal, and ovarian cancer screening trial. Br J Cancer. 2016;115(9):1087–95. https://doi.org/10.1038/bjc.2016.305.
Mondul AM, Moore SC, Weinstein SJ, Karoly ED, Sampson JN, Albanes D. Metabolomic analysis of prostate cancer risk in a prospective cohort: the alpha-tocolpherol, beta-carotene cancer prevention (ATBC) study. Int J Cancer. 2015;137(9):2124–32. https://doi.org/10.1002/ijc.29576.
Mayers JR, Wu C, Clish CB, et al. Elevation of circulating branched-chain amino acids is an early event in human pancreatic adenocarcinoma development. Nat Med. 2014;20(10):1193–8. https://doi.org/10.1038/nm.3686.
Guasch-Ferré M, Hruby A, Toledo E, et al. Metabolomics in prediabetes and diabetes: a systematic review and meta-analysis. Diabetes Care. 2016;39(5):833–46. https://doi.org/10.2337/dc15-2251.
Yu D, Moore SC, Matthews CE, et al. Plasma metabolomic profiles in association with type 2 diabetes risk and prevalence in Chinese adults. Metabolomics. 2015;12(1):3. https://doi.org/10.1007/s11306-015-0890-8.
Menni C, Fauman E, Erte I, et al. Biomarkers for type 2 diabetes and impaired fasting glucose using a nontargeted metabolomics approach. Diabetes. 2013;62(12):4270–6. https://doi.org/10.2337/db13-0570.
Floegel A, Stefan N, Yu Z, et al. Identification of serum metabolites associated with risk of type 2 diabetes using a targeted metabolomic approach. Diabetes. 2013;62(2):639–48. https://doi.org/10.2337/db12-0495.
Wang TJ, Larson MG, Vasan RS, et al. Metabolite profiles and the risk of developing diabetes. Nat Med. 2011;17(4):448–53. https://doi.org/10.1038/nm.2307.
Huang T, Balasubramanian R, Yao Y, et al. Associations of depression status with plasma levels of candidate lipid and amino acid metabolites: a meta-analysis of individual data from three independent samples of US postmenopausal women. Molecular Psychiatry. 2020. https://doi.org/10.1038/s41380-020-00870-9.
Liu X, Zheng P, Zhao X, et al. Discovery and validation of plasma biomarkers for major depressive disorder classification based on liquid chromatography-mass spectrometry. J Proteome Res. 2015;14(5):2322–30. https://doi.org/10.1021/acs.jproteome.5b00144.
Balasubramanian R, Paynter NP, Giulianini F, et al. Metabolomic profiles associated with all-cause mortality in the Women’s Health Initiative. Int J Epidemiol. 2020;49(1):289–300. https://doi.org/10.1093/ije/dyz211.
Deelen J, Kettunen J, Fischer K, et al. A metabolic profile of all-cause mortality risk identified in an observational study of 44,168 individuals. Nat Commun. 2019;10(1):3346. https://doi.org/10.1038/s41467-019-11311-9.
Yu B, Heiss G, Alexander D, Grams ME, Boerwinkle E. Associations between the serum metabolome and all-cause mortality among African Americans in the Atherosclerosis Risk in Communities (ARIC) study. Am J Epidemiol. 2016;183(7):650–6. https://doi.org/10.1093/aje/kwv213.
Cheng S, Larson MG, McCabe EL, et al. Distinct metabolomic signatures are associated with longevity in humans. Nat Commun. 2015;6:6791. https://doi.org/10.1038/ncomms7791.
Yu B, Zanetti KA, Temprosa M, et al. The Consortium of Metabolomics Studies (COMETS): metabolomics in 47 prospective cohort studies. Am J Epidemiol. 2019;188(6):991–1012. https://doi.org/10.1093/aje/kwz028.
Mahajan S, Caraballo C, Lu Y, et al. Trends in differences in health status and health care access and affordability by race and ethnicity in the United States, 1999–2018. JAMA. 2021;326(7):637–48. https://doi.org/10.1001/jama.2021.9907.
Shiels MS, Berrington de González A, Best AF, et al. Premature mortality from all causes and drug poisonings in the USA according to socioeconomic status and rurality an analysis of death certificate data by county from 2000–2015. Lancet Public Health. 2019;4(2):e97–106. https://doi.org/10.1016/S2468-2667(18)30208-1.
National Center for Health Statistics (US). Health, United States, 2018. National Center for Health Statistics (US); 2019. http://www.ncbi.nlm.nih.gov/books/NBK551095. Accessed 30 Dec 2020.
2019 National Healthcare Quality and Disparities Report. Agency for Healthcare Research and Quality; 2020. https://www.ahrq.gov/research/findings/nhqrdr/nhqdr19/index.html.
Williams DR. Miles to go before we sleep: racial inequities in health. J Health Soc Behav. 2012;53(3):279–95. https://doi.org/10.1177/0022146512455804.
Martin AR, Kanai M, Kamatani Y, Okada Y, Neale BM, Daly MJ. Current clinical use of polygenic scores will risk exacerbating health disparities. Nat Genet. 2019;51(4):584–91. https://doi.org/10.1038/s41588-019-0379-x.
Mahal BA, Alshalalfa M, Kensler KH, et al. Racial differences in genomic profiling of prostate cancer. N Engl J Med. 2020;383(11):1083–5. https://doi.org/10.1056/NEJMc2000069.
Gao Y, Cui Y. Deep transfer learning for reducing health care disparities arising from biomedical data inequality. Nat Commun. 2020;11(1):5131. https://doi.org/10.1038/s41467-020-18918-3.
Hu J, Yao J, Deng S, et al. Differences in metabolomic profiles between Black and White women and risk of coronary heart disease: an observational study of women from four US cohorts. Circ Res. 2022;131(7):601–15. https://doi.org/10.1161/CIRCRESAHA.121.320134.
Butler FM, Utt J, Mathew RO, et al. Plasma metabolomics profiles in Black and White participants of the Adventist Health Study-2 cohort. BMC Med. 2023;21(1):408. https://doi.org/10.1186/s12916-023-03101-4.
Vardarajan B, Kalia V, Manly J, et al. Differences in plasma metabolites related to Alzheimer’s disease, APOE ε4 status, and ethnicity. Alzheimers Dement (N Y). 2020. https://doi.org/10.1002/trc2.12025.
Gohlke JH, Lloyd SM, Basu S, et al. Methionine-homocysteine pathway in African-American prostate cancer. JNCI Cancer Spectr. 2019;3(2):pkz019. https://doi.org/10.1093/jncics/pkz019.
Vantaku V, Donepudi SR, Piyarathna DWB, et al. Large-scale profiling of serum metabolites in African American and European American patients with bladder cancer reveals metabolic pathways associated with patient survival. Cancer. 2019;125(6):921–32. https://doi.org/10.1002/cncr.31890.
Di Poto C, He S, Varghese RS, et al. Identification of race-associated metabolite biomarkers for hepatocellular carcinoma in patients with liver cirrhosis and hepatitis C virus infection. PLoS ONE. 2018;13(3): e0192748. https://doi.org/10.1371/journal.pone.0192748.
Walejko JM, Kim S, Goel R, et al. Gut microbiota and serum metabolite differences in African Americans and White Americans with high blood pressure. Int J Cardiol. 2018;271:336–9. https://doi.org/10.1016/j.ijcard.2018.04.074.
Shen J, Yan L, Liu S, Ambrosone CB, Zhao H. Plasma metabolomic profiles in breast cancer patients and healthy controls: by race and tumor receptor subtypes. Transl Oncol. 2013;6(6):757–65. https://doi.org/10.1593/tlo.13619.
Patel MJ, Batch BC, Svetkey LP, et al. Race and sex differences in small-molecule metabolites and metabolic hormones in overweight and obese adults. OMICS. 2013;17(12):627–35. https://doi.org/10.1089/omi.2013.0031.
VanderWeele TJ, Robinson WR. On causal interpretation of race in regressions adjusting for confounding and mediating variables. Epidemiology. 2014;25(4):473–84. https://doi.org/10.1097/EDE.0000000000000105.
VanderWeele TJ. Invited commentary: counterfactuals in social epidemiology—thinking outside of “the box.” Am J Epidemiol. 2020;189(3):175–8. https://doi.org/10.1093/aje/kwz198.
Williams DR, Sternthal M. Understanding racial/ethnic disparities in health: sociological contributions. J Health Soc Behav. 2010;51(Suppl):S15–27. https://doi.org/10.1177/0022146510383838.
Mittelstrass K, Ried JS, Yu Z, et al. Discovery of sexual dimorphisms in metabolic and genetic biomarkers. PLoS Genet. 2011. https://doi.org/10.1371/journal.pgen.1002215.
Colditz GA, Hankinson SE. The Nurses’ Health Study: lifestyle and health among women. Nat Rev Cancer. 2005;5(5):388–96. https://doi.org/10.1038/nrc1608.
Hankinson SE, Willett WC, Manson JE, et al. Alcohol, height, and adiposity in relation to estrogen and prolactin levels in postmenopausal women. J Natl Cancer Inst. 1995;87(17):1297–302. https://doi.org/10.1093/jnci/87.17.1297.
Brantley KD, Zeleznik OA, Rosner B, et al. Plasma metabolomics and breast cancer risk over 20 years of follow-up among postmenopausal women in the Nurses’ Health Study. Cancer Epidemiol Biomarkers Prev. 2022;31(4):839–50. https://doi.org/10.1158/1055-9965.EPI-21-1023.
The Women’s Health Initiative Study Group. Design of the Women’s Health Initiative clinical trial and observational study. Control Clin Trials. 1998;19(1):61–109. https://doi.org/10.1016/s0197-2456(97)00078-0.
Rossouw JE, Anderson GL, Prentice RL, et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results From the Women’s Health Initiative randomized controlled trial. JAMA. 2002;288(3):321–33. https://doi.org/10.1001/jama.288.3.321.
Anderson GL, Limacher M, Assaf AR, et al. Effects of conjugated equine estrogen in postmenopausal women with hysterectomy: the Women’s Health Initiative randomized controlled trial. JAMA. 2004;291(14):1701–12. https://doi.org/10.1001/jama.291.14.1701.
Townsend MK, Clish CB, Kraft P, et al. Reproducibility of metabolomic profiles among men and women in 2 large cohort studies. Clin Chem. 2013;59(11):1657–67. https://doi.org/10.1373/clinchem.2012.199133.
Do KT, Wahl S, Raffler J, et al. Characterization of missing values in untargeted MS-based metabolomics data and evaluation of missing data handling strategies. Metabolomics. 2018. https://doi.org/10.1007/s11306-018-1420-2.
Shah JS, Rai SN, DeFilippis AP, Hill BG, Bhatnagar A, Brock GN. Distribution based nearest neighbor imputation for truncated high dimensional data with applications to pre-clinical and clinical metabolomics studies. BMC Bioinform. 2017. https://doi.org/10.1186/s12859-017-1547-6.
Armitage EG, Godzien J, Alonso-Herranz V, López-Gonzálvez Á, Barbas C. Missing value imputation strategies for metabolomics data. Electrophoresis. 2015;36(24):3050–60. https://doi.org/10.1002/elps.201500352.
Hrydziuszko O, Viant MR. Missing values in mass spectrometry based metabolomics: an undervalued step in the data processing pipeline. Metabolomics. 2012;8(1):161–74. https://doi.org/10.1007/s11306-011-0366-4.
Gao X, Starmer J, Martin ER. A multiple testing correction method for genetic association studies using correlated single nucleotide polymorphisms. Genet Epidemiol. 2008;32(4):361–9. https://doi.org/10.1002/gepi.20310.
Subramanian A, Tamayo P, Mootha Vk, et al. Gene set enrichment analysis: a knowledge-based approach for interpreting genome-wide expression profiles. In: Proceedings of the National Academy of Sciences of the United States of America. https://doi.org/10.1073/pnas.0506580102
Rhee EP, Cheng S, Larson MG, et al. Lipid profiling identifies a triacylglycerol signature of insulin resistance and improves diabetes prediction in humans. J Clin Invest. 2011;121(4):1402–11. https://doi.org/10.1172/JCI44442.
Korotkevich G, Sukhov V, Sergushichev A. Fast gene set enrichment analysis. bioRxiv. 2019. https://doi.org/10.1101/060012.
Tchetgen Tchetgen EJ. Inverse odds ratio-weighted estimation for causal mediation analysis. Stat Med. 2013;32(26):4567–80. https://doi.org/10.1002/sim.5864.
Nguyen QC, Osypuk TL, Schmidt NM, Glymour MM, Tchetgen Tchetgen EJ. Practical guidance for conducting mediation analysis with multiple mediators using inverse odds ratio weighting. Am J Epidemiol. 2015;181(5):349–56. https://doi.org/10.1093/aje/kwu278.
Shi B, Choirat C, Coull BA, VanderWeele TJ, Valeri L. CMAverse: a suite of functions for reproducible causal mediation analyses. Epidemiology. 2021;32(5):e20–2. https://doi.org/10.1097/EDE.0000000000001378.
Patil P, Peng RD, Leek JT. What should researchers expect when they replicate studies? A statistical view of replicability in psychological science. Perspect Psychol Sci. 2016;11(4):539–44. https://doi.org/10.1177/1745691616646366.
Spence JR, Stanley DJ. Prediction interval: what to expect when you’re expecting … A replication. PLoS ONE. 2016;11(9): e0162874. https://doi.org/10.1371/journal.pone.0162874.
Knol MJ, VanderWeele TJ. Recommendations for presenting analyses of effect modification and interaction. Int J Epidemiol. 2012;41(2):514–20. https://doi.org/10.1093/ije/dyr218.
VanderWeele TJ, Knol MJ. A tutorial on interaction. Epidemiol Methods. 2014;3(1):33–72. https://doi.org/10.1515/em-2013-0005.
Vanderweele TJ. Surrogate measures and consistent surrogates. Biometrics. 2013;69(3):561–9. https://doi.org/10.1111/biom.12071.
Ward JB, Gartner DR, Keyes KM, Fliss MD, McClure ES, Robinson WR. How do we assess a racial disparity in health? Distribution, interaction, and interpretation in epidemiological studies. Ann Epidemiol. 2019;29:1–7. https://doi.org/10.1016/j.annepidem.2018.09.007.
Brown LL, Cohen B, Tabor D, Zappalà G, Maruvada P, Coates PM. The vitamin D paradox in Black Americans: a systems-based approach to investigating clinical practice, research, and public health—expert panel meeting report. BMC Proc. 2018;12(Suppl 6):6. https://doi.org/10.1186/s12919-018-0102-4.
Zeleznik OA, Wittenbecher C, Deik A, et al. Intrapersonal stability of plasma metabolomic profiles over 10 years among women. Metabolites. 2022;12(5):372. https://doi.org/10.3390/metabo12050372.
Funding
The Nurses’ Health Study analyses were funded by the National Cancer Institute, National Institutes of Health, U.S. Department of Health and Human Services (grants UM1 CA186107, R01 CA49449, and P01 CA87969). Census tract variables were ascertained through funding from the National Institute of Environmental Health Sciences, National Institutes of Health, U.S. Department of Health and Human Services (grants R01 ES017017 and R01 ES028033). The Women’s Health Initiative program is funded by the National Heart, Lung, and Blood Institute, National Institutes of Health, U.S. Department of Health and Human Services through contracts HHSN268201600018C, HHSN268201600001C, HHSN268201600002C, HHSN268201600003C, and HHSN268201600004C. Metabolomic analysis in the Women’s Health Initiative was funded by the National Heart, Lung, and Blood Institute, National Institutes of Health, U.S. Department of Health and Human Services through contract HHSN268201300008C. A list of WHI investigators is available online at https://www.whi.org/researchers/Documents%20%20Write%20a%20Paper/WHI%20Investigator%20Short%20List.pdf. E.E. McGee was supported by funding from the Eric and Wendy Schmidt Center at the Broad Institute of MIT and Harvard. The funders had no role in the design of the study; collection, analysis, or interpretation of data; writing of the report; or decision to submit the manuscript for publication. The content presented here is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or any other sponsors.
Author information
Authors and Affiliations
Contributions
Conceptualization and design of the study: EEM, OAZ, CBC, WCW, KMR, RMT, and AHE. Acquisition of data: CBC, JAP, WCW, KMR, RMT, and AHE. Analysis of data: EEM. Interpretation of data: EEM, OAZ, RB, JH, BAR, JWW, CBC, JAP, WCW, KMR, RMT, and AHE. Drafting of manuscript: EEM. Review and approval of final manuscript: EEM, OAZ, RB, JH, BAR, JWW, CBC, JAP, WCW, KMR, RMT, and AHE. EEM had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interest to disclose.
Ethics approval
The NHS study protocol was approved by the institutional review boards of Brigham and Women's Hospital and Harvard T.H. Chan School of Public Health. Institutional review board approval for the WHI was obtained at each clinical center.
Consent to participate
In the NHS, return of the completed questionnaire was considered to imply informed consent. In the WHI, informed consent was obtained from all participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
McGee, E.E., Zeleznik, O.A., Balasubramanian, R. et al. Differences in metabolomic profiles between Black and White women in the U.S.: Analyses from two prospective cohorts. Eur J Epidemiol (2024). https://doi.org/10.1007/s10654-024-01111-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10654-024-01111-x