Abstract
Purpose
To report novel multimodal imaging features and long-term follow-up of Orthodenticle Homeobox 2 (OTX2)-associated pattern Gdystrophy.
Methods
A 14-year-old boy referred with glaucoma suspect and macular pigmentation underwent fundus autofluorescence imaging, optical coherence tomography, fluorescein and indocyanine green angiography, visual field test, microperimetry and electrophysiology over a ten-year period. Next-generation sequencing panel identified a de novo heterozygous likely pathogenic OTX2 variant, c.259G>A, [p.(Glu87Lys)].
Results
Visual acuity was 20/40 OD and 20/30 OS. Examination showed bilateral enlarged optic nerve heads and increased disc cupping, multiple cilioretinal arteries, a pigmentary maculopathy with stellate-shaped region of hypoautofluorescence, shallow serous macular detachment, subretinal deposits and temporal avascular retina. Angiography showed no source of leakage and absence of retinal neovascularisation despite extensive peripheral non perfusion. Electrophysiological assessments demonstrated mild progressive rod and cone pathway abnormalities, reduced light-adapted b:a ratio, and reduced Arden ratio on electro-oculogram. Ten-year follow-up confirmed a stable disease course despite persistent submacular fluid. There was no associated pituitary structural abnormality or dysfunction.
Conclusions
This case study contributes to further understanding of OTX2-associated pattern dystrophy, highlighting its stability over 10 years. Further investigation into inter-individual and intrafamilial variability is warranted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Orthodenticle Homeobox 2 (OTX2) is a master gene on chromosome 14q22.3 coding for a critical transcription factor involved in the embryonic development of the forebrain and the eye including photoreceptors, bipolar cells, and retinal pigment epithelial (RPE) precursor cells [1, 2]. Detailed multimodal imaging features of OTX2-associated pattern dystrophy and its long-term outcomes are lacking due to its rarity and short observation time in previous studies [3,4,5]. Herein, we report novel phenotypic features of OTX2-associated retinopathy and the 10-year functional and structural outcomes in a 25-year-old male who has undergone multimodal imaging since the age of 14.
Clinical presentation
A 14-year-old boy of Indian origin presented with incidental bilateral macular pigmentary changes whilst being evaluated for suspected glaucoma. He had delayed speech onset at 2 years of age and myopia was noted at age 3. His vision was 20/40 OD and 20/30 OS. Intraocular pressures were 13 mmHg OD and 12 mmHg OS with open angles on gonioscopy. Fundoscopy revealed macular pattern dystrophy, megalopapilla with physiological disc cupping, multiple cilioretinal arteries, and temporal peripheral retinal avascularity bilaterally (Table 1, Fig. 1A and B).
Pseudocolour optic disc photos reveal megalopapillae with physiological disc cupping in both eyes at the initial presentation (A, B). Short-wave fundus autofluorescence displays a central irregular-shaped hypoautofluorescent region with mild perifoveal hyperautofluorescence in both eyes (C, D). Fundus fluorescein angiography (FFA) of the left eye (mid-phase) shows macular stippling (E). Ultrawide-field FFA demonstrates peripheral avascularity (marked by the white star) and retinochoroidal atrophy without neovascularization (F). Indocyanine Green dye test exhibits multifocal hyperfluorescent areas without leakage in the late phase (G, H). Heidelberg spectral-domain optical coherence tomography (OCT) after 10 years of follow-up demonstrates shallow persistent foveal detachment with a thickened ellipsoid zone and subretinal deposits (shown by the white arrow, (I). The ellipsoid zone remains fused with the interdigitation zone, except at the fovea where the latter became more prominent (indicated by three black arrowheads)
Short-wave fundus autofluorescence (AF) showed a central stellate-shaped region of hypoautofluorescence with mild perifoveal hyperautofluorescence in both eyes (Fig. 1C and D). Spectral-domain optical coherence tomography (OCT, Heidelberg Spectralis, Heidelberg Engineering, Heidelberg, Germany) showed shallow neurosensory detachment with ellipsoid and interdigitation zone fusion resulting in apparent thickening of band 2 in the perifoveal area. Interdigitation zone thickening was notable in the foveal region. An ultrawide-field fluorescein angiography (Optos, Dunfermline, Scotland) revealed stippled foveal hyperfluorescence and multiple cilioretinal arteries originating from the nasal and superior discs, together with far-temporal avascular retina (Fig. 1E and F). Indocyanine green angiography showed abnormal macular choroidal vasculature with two intensely hyperfluorescent lesions within the fovea that corresponded to focal thickening of the RPE layer (Fig. 1G and H). There was no angiographic leakage.
Humphrey visual field examinations were within normal limits OU. Baseline microperimetry (Macular Integrity Assessment, MAIA, CenterVue, Padova, Italy) showed focal shallow scotoma across the macular region (Supp. Fig. S1A and S1B, online source 1). Visual electrophysiology (RETIport 3.2, Roland Consult, Brandenburg, Germany) was performed incorporating the 2008 standards as set out by the International Society for Clinical Electrophysiology of Vision (ISCEV) [6]. Electro-oculography performed in accordance to the ISCEV standard [7] revealed an Arden ratio of 1.5 OD and 1.6 OS (normal ≥ 1.7, Fig. 2) in accordance with the ISCEV Standard for Clinical Electro-oculography Full-field ERG showed dark-adapted (DA) responses were within the normal range at baseline (Supp. Table S1, online source 2). Light-adapted (LA) 30 Hz flicker was reduced and delayed. Reduced b-wave amplitude and reduced b:a ratio (2.8 OD, 2.1 OS, normal ≥ 3.0) in the LA3.0 standard flash indicated abnormalities in the inner retinal cone pathway (Fig. 3).
Electroretinogram of patient in 2013, 2014, 2018 against an age-similar control subject. DA 0.01: dark-adapted 0.01 cd s m−2; DA 3.0: dark-adapted 3.0 cd s m−2; DA 10.0: dark-adapted 10.0 cd s m−2; LA 3.0: light-adapted 3.0 cd s m−2 at 30 cd.m−2 background; LA 30 Hz: light-adapted 3.0 cd s m−2 flicker at 30 cd m−2 background; LA On–Off Bipolar: light adapted on–off response
Magnetic resonance imaging and endocrine work up (serum electrolytes, thyroid stimulating hormone, prolactin, insulin-like growth factor 1, cortisol, follicular stimulating hormone and luteinizing hormone) excluded pituitary structural abnormality and dysfunction.
Molecular diagnosis
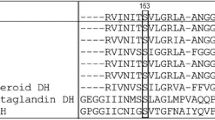
Genetic analysis was performed through the Australian Inherited Retinal Diseases Registry and DNA Bank. Genomic DNA was extracted from peripheral blood as described previously [8]. Next-generation sequencing was performed (Retinal Dystrophy Smart panel, version 8; Casey Eye Institute Molecular Diagnostic laboratory (CEI), Portland, Oregon, USA) targeting all exons and flanking intronic sequences of 244 retinal dystrophy genes [9]. Sanger sequencing was used to confirm candidate variants in the proband and for phase testing in parental DNA (CEI). Genetic analysis of the proband identified a heterozygous OTX2 variant, NM_001270525.1:c.259G>A, [p.(Glu87Lys)], previously reported as a dominant variant published as NM_001270523.1:c.235G>A, [p.(Glu79Lys)] by Vincent et al. [3] phase testing of parental DNA showed neither parent carried the variant. We have assessed this variant as likely pathogenic (PM6_SUPP, PS4_MOD, PM2_SUPP, PP3_STR) according to ACMG standards and guidelines and associated literature (Supp. Table S2, online source 3) [10,11,12,13]. We have not applied the PP5 rule, “reputable source recently reports variant as pathogenic, but the evidence is not available to the laboratory to perform an independent evaluation”, as recommended by Biesecker and Harrison [14].
Follow-up Imaging
Ten years after presentation, the patient reported declining vision in the right eye. At 25, his visual acuities were 20/50 OD and 20/30 OS and IOP was 19 mmHg OD and 20 mmHg OS without topical glaucoma treatment. There was no clinical or OCT progression. Subretinal fluid (SRF) fluctuated over the 10 years with central subfield thickness (CST) ranging from 288 to 368 µm, unresponsive to oral acetazolamide. Some subretinal deposits resolved, whilst others remained. The ellipsoid zone remained fused with the interdigitation zone except at the fovea where the latter remained prominent (Fig. 1I). The most recent MAIA showed a mean sensitivity of 26.6 dB OD and 26.4 dB OS (Supp. Fig. S1C and S1D). At age 20, 5 years after baseline, follow-up electrophysiology showed a further reduction in the Arden ratio (1.4 OD, 1.5 OS, normal ≥ 1.7) whilst full-field ERG showed additional rod pathway abnormality at the photoreceptor level and cone pathway dysfunction at both photoreceptor and post-photoreceptor levels (reduced LA3 b:a ratios of 2.52 OD and 2.94 OS). On–off response showed a reduced b-wave response (24 µV OD, 20 µV OS, normal 28–63 µV) indicating an on-bipolar cell abnormality (Figs. 2 and 3, Supp. Table S1).
Discussion
OTX2-associated eye disease is rare and is known for its association with pituitary abnormalities and diverse ocular phenotypes [2,3,4, 15]. Although 52 variants have been listed in the Leiden Open Variation Database (LOVD), only 30 are considered pathogenic or likely pathogenic. OTX2 disease-causing variants are more commonly known for anophthalmia, microphthalmia, anterior segment dysgenesis, optic nerve dysplasia/hypoplasia and combined pituitary hormone deficiency, with an overall estimated frequency of ocular anomalies as high as 86% [3, 15,16,17,18,19]. The OTX2 variant, c.259G > A, was previously detected by exome sequencing (234 genes) of DNA from 298 probands diagnosed with early-onset high myopia [20]. However, there was no phenotypic data except for the presence of high myopia defined by at least −6.0D or axial length of > 26 mm before the age of seven. Vincent et al. found the same OXT2 variant heterozygously in two families with autosomal dominant pattern dystrophy [3]. They noted optic nerve head dysplasia and microcornea with variable photoreceptor abnormalities on ERG. The detection of anomalous optic nerve head prompted ophthalmic assessment in our case. Interestingly, the presence of megalopapilla, alongside physiologic disc cupping and incidentally elevated IOP, has not been documented previously as presenting features of OTX2-associated eye disease. Up to 51% of individuals with OTX-2-associated eye disease had brain and pituitary abnormalities [21]. However, despite optic nerve head irregularities, our patient showed no associated brain or pituitary changes. This observation is consistent with the previous report by Vincent et al. [3]. The variable brain versus ocular phenotype may be related to unique brain isoform function which is unaffected by the missense variant specific for a pattern dystrophy.
Previous reports of OTX2-related macular pattern dystrophy described shallow retinal elevation on OCT but lacked detailed multimodal imaging or long-term follow-up [3, 4, 19]. We noted an irregular geographic region of poorly defined macular hypoautofluorescence with pericentral hyperautofluorescence. These changes were symmetrical with normal peripheral retinal AF signals in both eyes. In our case, we noted shallow SRF accompanied by subretinal hyperreflective deposits. Despite oral acetazolamide treatment, the SRF exhibited mild fluctuations and remained unresponsive. While certain subretinal deposits resolved, others remained stable. Additionally, fusion of the ellipsoid and interdigitation zones resulted in a distinctive thickened second band on OCT, characteristic of PRPH2-associated retinopathy [22]. An atypical feature in this case is the separation of the interdigitation zone from band 2 and thickening of band 3 in the fovea. These separations could be attributed to the role of OTX2 in preserving the contact between photoreceptors and the RPE over time, a phenomenon that has also been demonstrated in a knockout mouse model [23]. Indocyanine green angiography revealed multifocal staining during the mid-phase co-localized with subretinal deposits. However, there was no obvious leak during transit to reveal the source of SRF. One may hypothesize that SRF is a sign of RPE pump insufficiency resulting from an OTX2-related developmental anomaly. Further unique findings included peripheral avascularity resembling familial exudative vitreoretinopathy and retinopathy of prematurity without vessel straightening, macular traction, retinal neovascularization, or a history of prematurity. Incomplete vascularisation of the peripheral retina has been reported in the microphthalmia eyes of a 25-month-old female harbouring the OTX2 variant, c.135dupA, [p.(Thr46AsnfsTer84)]. There was no evidence of retinal neovascularisation at 10-years of follow-up even without laser photocoagulation to areas of avascularity.
Detailed electrophysiological assessment demonstrated a progressive RPE dysfunction over a 5-year interval as shown by the declining Arden ratio (Fig. 2). This trend aligns with cross sectional findings of marginal EOG parameter in young children and significantly lower values in young adults [3]. The progressive reduction in EOG values may be linked to the role of OTX2 in RPE function as evidenced by a knockout mice model [3, 23]. Studies have previously found rod and cone photoreceptor pathway abnormalities including On- and Off-bipolar pathway alterations and S-cone pathway preservation [3, 5]. We observed progressive rod and cone photoreceptor abnormalities with additional post-photoreceptor dysfunction in the cone pathway (Supp. Table S1). Profound inner retinal dysfunction has been reported previously in a 7-year-old male with infantile onset retinal dystrophy resulting from the heterozygous OTX2 variant, c.413C>G, [p.(Ser138Ter)] [5]. These findings are consistent with the known role of OTX2 in photoreceptor and bipolar cell development and terminal differentiation [24, 25]. The declining LA3.0 a-wave amplitude may be related photoreceptor degeneration due to the chronic shallow submacular fluid secondary to RPE dysfunction. However, there was no multimodal imaging changes to indicate rod photoreceptor loss as suggested by the declining DA3.0 a-wave amplitude.
In conclusion, we present a case of OTX2-associated macular pattern dystrophy with megalopapilla, retinal vascular anomalies and relatively stable disease course. Despite persistent shallow subretinal fluid, there was no RPE atrophy or macular sensitivity decline. Progressive generalised rod and cone system, and RPE dysfunction was evident despite SRF being limited to the macula and preserved peripheral fundus autofluorescence signal. Further long-term follow-up studies are warranted to determine the mechanism for functional decline in the absence of structural change.
References
Kastury K, Druck T, Huebner K et al (1994) Chromosome locations of human EMX and OTX genes. Genomics 22(1):41–45. https://doi.org/10.1006/geno.1994.1343
Diacou R, Zhao Y, Zheng D, Cvekl A, Liu W (2018) Six3 and Six6 are jointly required for the maintenance of multipotent retinal progenitors through both positive and negative regulation. Cell Rep 25(9):2510–2523. https://doi.org/10.1016/j.celrep.2018.10.106
Vincent A, Forster N, Maynes JT et al (2014) OTX2 mutations cause autosomal dominant pattern dystrophy of the retinal pigment epithelium. J Med Genet 51(12):797–805. https://doi.org/10.1136/jmedgenet-2014-102620
Wangding S, Colaiacovo S, Makar I, Saleh M (2022) OTX2 mutation associated with severe myopia in a Canadian family. Ophthalmic Genet 43(3):389–391. https://doi.org/10.1080/13816810.2021.2015791
Henderson RH, Williamson KA, Kennedy JS et al (2009) A rare de novo nonsense mutation in OTX2 causes early onset retinal dystrophy and pituitary dysfunction. Mol Vis 15:2442–2447
Marmor MF, Fulton AB, Holder GE, Miyake Y, Brigell M, Bach M (2009) ISCEV Standard for full-field clinical electroretinography (2008 update). Doc Ophthalmol 118(1):69–77. https://doi.org/10.1007/s10633-008-9155-4
Constable PA, Bach M, Frishman LJ, Jeffrey BG, Robson AG (2017) ISCEV Standard for clinical electro-oculography (2017 update). Doc Ophthalmol 134(1):1–9. https://doi.org/10.1007/s10633-017-9573-2
De Roach JN, McLaren TL, Paterson RL et al (2013) Establishment and evolution of the Australian inherited retinal disease register and DNA bank. Clin Exp Ophthalmol 41(5):476–483. https://doi.org/10.1111/ceo.12020
Chiang J, Lamey T, McLaren T, Thompson JA, Montgomery H, De Roach J (2015) Progress and prospects of next-generation sequencing testing for inherited retinal dystrophy. Expert Rev Mol Diagn 15(10):1269–1275. https://doi.org/10.1586/14737159.2015.1081057
Richards S, Aziz N, Bale S et al (2015) Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American college of medical genetics and genomics and the association for molecular pathology. Genet Med 17(5):405–424. https://doi.org/10.1038/gim.2015.30
Pejaver V, Byrne AB, Feng BJ et al (2022) Calibration of computational tools for missense variant pathogenicity classification and ClinGen recommendations for PP3/BP4 criteria. Am J Hum Genet 109(12):2163–2177. https://doi.org/10.1016/j.ajhg.2022.10.013
Durkie MCE, Berry I, Owens M, Turnbull C, Scott RH, Taylor RW, Deans ZC, Ellard S, Baple EL, McMullen DJ (2024) Best Practice Guidelines: The Association for Clinical Genomic Science (acgs.uk.com). ACGS Best practice guidelines for variant classification in rare disease secondary ACGS best practice guidelines for variant classification in rare disease
Zhang J, Yao Y, He H, Shen J (2020) Clinical interpretation of sequence variants. Curr Protoc Hum Genet 106(1):e98. https://doi.org/10.1002/cphg.98
Biesecker LG, Harrison SM (2018) The ACMG/AMP reputable source criteria for the interpretation of sequence variants. Genet Med 20(12):1687–1688. https://doi.org/10.1038/gim.2018.42
Mauri L, Franzoni A, Scarcello M et al (2015) SOX2, OTX2 and PAX6 analysis in subjects with anophthalmia and microphthalmia. Eur J Med Genet 58(2):66–70. https://doi.org/10.1016/j.ejmg.2014.12.005
Deml B, Reis LM, Lemyre E, Clark RD, Kariminejad A, Semina EV (2016) Novel mutations in PAX6, OTX2 and NDP in anophthalmia, microphthalmia and coloboma. Eur J Hum Genet 24(4):535–541. https://doi.org/10.1038/ejhg.2015.155
Gregory LC, Gergics P, Nakaguma M et al (2021) The phenotypic spectrum associated with OTX2 mutations in humans. Eur J Endocrinol 185(1):121–135. https://doi.org/10.1530/eje-20-1453
Miesfeld JB, Brown NL (2019) Eye organogenesis: a hierarchical view of ocular development. Curr Top Dev Biol 132:351–393. https://doi.org/10.1016/bs.ctdb.2018.12.008
Forgacs J, Bozin I (1966) Familial manifestations of grouped pigmentation in macular region. Ophthalmologica 152(5):364–368. https://doi.org/10.1159/000304992
Sun W, Huang L, Xu Y et al (2015) Exome sequencing on 298 probands with early-onset high myopia: approximately one-fourth show potential pathogenic mutations in RetNet genes. Investig Ophthalmol Visual Sci 56(13):8365–8372. https://doi.org/10.1167/iovs.15-17555
Schilter KF, Schneider A, Bardakjian T et al (2011) OTX2 microphthalmia syndrome: four novel mutations and delineation of a phenotype. Clin Genet 79(2):158–168. https://doi.org/10.1111/j.1399-0004.2010.01450.x
Heath Jeffery RC, Lo J, Thompson JA et al (2023) Analysis of the outer retinal bands in ABCA4 and PRPH2-associated retinopathy using OCT. Ophthalmol Retina. https://doi.org/10.1016/j.oret.2023.05.010
Béby F, Housset M, Fossat N et al (2010) Otx2 gene deletion in adult mouse retina induces rapid RPE dystrophy and slow photoreceptor degeneration. PLoS ONE 5(7):e11673. https://doi.org/10.1371/journal.pone.0011673
Larsen KB, Lutterodt M, Rath MF, Møller M (2009) Expression of the homeobox genes PAX6, OTX2, and OTX1 in the early human fetal retina. Int J Dev Neurosci 27(5):485–492. https://doi.org/10.1016/j.ijdevneu.2009.04.004
Kim DS, Matsuda T, Cepko CL (2008) A core paired-type and POU homeodomain-containing transcription factor program drives retinal bipolar cell gene expression. J Neurosci 28(31):7748–7764. https://doi.org/10.1523/jneurosci.0397-08.2008
Acknowledgements
We are grateful to Terri L. McLaren, BSc and Enid Chelva, BSc for their collaboration and helpful discussions.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. FKC received funding from: Future Health Research and Innovation Fund, the McCusker Charitable Foundation, Channel 7 Telethon Trust, Retina Australia, National Health & Medical Research Council of Australia (project and fellowship grant no.: GNT1116360, GNT1188694, GNT1054712 and MRF1142962).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
The patient gave informed consent for participation in a natural history study of inherited retinal disease (The University of Western Australia, Human Research Ethics Committee: 2021/ET000151).
Statement of human rights
Genotyping was performed on patient after consent: The patient gave consent for participation in genotyping through the Registry (Sir Charles Gardner Hospital Human Research Ethics Committee: 19/1443H).
Statement on the welfare of animals
No animal was used in this study.
Consent for publication
The participant has given consent as part of the WARD study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ramakrishnan, P., Kenworthy, M.K., Alexis, J.A. et al. Non-syndromic OTX2-associated pattern dystrophy: a 10-year multimodal imaging study. Doc Ophthalmol (2024). https://doi.org/10.1007/s10633-024-09983-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10633-024-09983-w