Abstract
Purpose
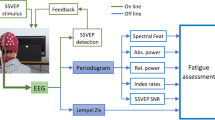
There are several stimulus paradigms used in objective visual acuity assessment based on steady-state visual evoked potentials (SSVEPs). The aim of this study was to explore the difference and performance of common used six stimulus paradigms (reverse vertical sinusoidal gratings, reverse horizontal sinusoidal gratings, reverse vertical square-wave gratings, brief-onset vertical sinusoidal gratings, reversal checkerboards and oscillating expansion–contraction concentric-rings) of SSVEP acuity assessment.
Methods
We tested subjective visual acuity both by tumbling E and Freiburg Visual Acuity and Contrast Test (FrACT) in 11 subjects. SSVEPs were induced by 11 spatial frequencies for each paradigm, and then a threshold determination criterion was used to define the objective SSVEP visual acuity.
Results
After SSVEP signal analysis, we found there was difference in SSVEP response of harmonic components and no difference in sensitive electrode placement for the six paradigms. We selected six electrodes (PO3, POz, PO4, O1, Oz and O2) as the sensitive electrodes to use in data processing for each paradigm. The results showed that except for brief-onset vertical sinusoidal gratings, the correlation and agreement between objective SSVEP and subjective FrACT acuity were all quite good, demonstrating good performance in acuity detection for the rest five paradigms.
Conclusion
Except for brief-onset vertical sinusoidal gratings, all the five stimulus paradigms of reverse vertical sinusoidal gratings, reverse horizontal sinusoidal gratings, reverse vertical square-wave gratings, reversal checkerboards and oscillating expansion–contraction concentric-rings performed quite well in objective SSVEP visual acuity assessment.









Similar content being viewed by others
References
World Health Organization (2018) Blindness and visual impairment. https://www.who.int/news-room/fact-sheets/detail/blindness-and-visual-impairment. Accessed October 11 2018
Bourne RRA, Flaxman SR, Braithwaite T, Cicinelli MV, Das A, Jonas JB, Keeffe J, Kempen JH, Leasher J, Limburg H, Naidoo K, Pesudovs K, Resnikoff S, Silvester A, Stevens GA, Tahhan N, Wong TY, Taylor HR, Vision Loss Expert G (2017) Magnitude, temporal trends, and projections of the global prevalence of blindness and distance and near vision impairment: a systematic review and meta-analysis. Lancet Glob Health 5(9):e888–e897. https://doi.org/10.1016/S2214-109X(17)30293-0
Fricke TR, Tahhan N, Resnikoff S, Papas E, Burnett A, Ho SM, Naduvilath T, Naidoo KS (2018) Global prevalence of presbyopia and vision impairment from uncorrected presbyopia: systematic review, meta-analysis, and modelling. Ophthalmology 125(10):1492–1499. https://doi.org/10.1016/j.ophtha.2018.04.013
Bach M (1996) The Freiburg Visual Acuity test - Automatic measurement of visual acuity. Optometry Vision Sci 73(1):49–53. https://doi.org/10.1097/00006324-199601000-00008
Incesu AI, Sobaci G (2011) Malingering or simulation in ophthalmology-visual acuity. Int J Ophthalmol 4(5):558–566. https://doi.org/10.3980/j.issn.2222-3959.2011.05.19
Fahad A, Leat SJ, Elizabeth I (2010) The technique, validity and clinical use of the sweep VEP. Ophthal Physl Opt 28(5):393–403. https://doi.org/10.1111/j.1475-1313.2008.00591.x
Norcia AM, Appelbaum LG, Ales JM, Cottereau BR, Rossion B (2015) The steady-state visual evoked potential in vision research: a review. J Vis 15(6):4. https://doi.org/10.1167/15.6.4
Anne K, Hana L, Andre M, Eberhart Z, Herbert JG (2013) A comparison of the performance of three visual evoked potential-based methods to estimate visual acuity. Doc Ophthalmol 126(1):45–56. https://doi.org/10.1007/s10633-012-9359-5
Mackay AM, Bradnam MS, Hamilton R, Elliot AT, Dutton GN (2008) Real-time rapid acuity assessment using VEPs: development and validation of the step VEP technique. Invest Ophthalmol Vis Sci 49(1):438–441. https://doi.org/10.1167/iovs.06-0944
Almoqbel FM, Yadav NK, Leat SJ, Head LM, Irving EL (2011) Effects of sweep VEP parameters on visual acuity and contrast thresholds in children and adults. Graefes Arch Clin Exp Ophthalmol 249(4):613–623. https://doi.org/10.1007/s00417-010-1469-8
Strasser T, Nasser F, Langrova H, Zobor D, Lisowski L, Hillerkuss D, Sailer C, Kurtenbach A, Zrenner E (2019) Objective assessment of visual acuity: a refined model for analyzing the sweep VEP. Doc Ophthalmol 138(2):97–116. https://doi.org/10.1007/s10633-019-09672-z
Zheng X, Xu G, Wang Y, Han C, Du C, Yan W, Zhang S, Liang R (2019) Objective and quantitative assessment of visual acuity and contrast sensitivity based on steady-state motion visual evoked potentials using concentric-ring paradigm. Doc Ophthalmol 139(2):123–136. https://doi.org/10.1007/s10633-019-09702-w
Hemptinne C, Liu-Shuang J, Yuksel D, Rossion B (2018) Rapid objective assessment of contrast sensitivity and visual acuity with sweep visual evoked potentials and an extended electrode array. Invest Ophthalmol Vis Sci 59(2):1144–1157. https://doi.org/10.1167/iovs.17-23248
Tyler CW, Apkarian P, Levi DM, Nakayama K (1979) Rapid assessment of visual function: an electronic sweep technique for the pattern visual evoked potential. Invest Ophthalmol Vis Sci 18(7):703–713
Norcia AM, Tyler CW (1985) Spatial frequency sweep VEP: visual acuity during the first year of life. Vision Res 25(10):1399–1408. https://doi.org/10.1016/0042-6989(85)90217-2
Arai M, Katsumi O, Paranhos FRL, DeFaria JML, Hirose T (1997) Comparison of Snellen acuity and objective assessment using the spatial frequency sweep PVER. Graef Arch Clin Exp 235(7):442–447. https://doi.org/10.1007/Bf00947064
Zhou P, Zhao MW, Li XX, Hu XF, Wu X, Niu LJ, Yu WZ, Xu XL (2008) A new method of extrapolating the sweep pattern visual evoked potential acuity. Doc Ophthalmol 117(2):85–91. https://doi.org/10.1007/s10633-007-9095-4
Bach M, Maurer JP, Wolf ME (2008) Visual evoked potential-based acuity assessment in normal vision, artificially degraded vision, and in patients. Br J Ophthalmol 92(3):396–403. https://doi.org/10.1136/bjo.2007.130245
Hamilton R, Bradnam MS, Dutton GN, Lai Chooi Yan AL, Lavy TE, Livingstone I, Mackay AM, Mackinnon JR (2013) Sensitivity and specificity of the step VEP in suspected functional visual acuity loss. Doc Ophthalmol 126(2):99–104. https://doi.org/10.1007/s10633-012-9362-x
Vesely P (2015) Contribution of sVEP visual acuity testing in comparison with subjective visual acuity. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub 159(4):616–621. https://doi.org/10.5507/bp.2015.002
Hoffmann MB, Brands J, Behrens-Baumann W, Bach M (2017) VEP-based acuity assessment in low vision. Doc Ophthalmol 135(3):209–218. https://doi.org/10.1007/s10633-017-9613-y
Brainard DH (1997) The psychophysics toolbox. Spat Vis 10(4):433–436. https://doi.org/10.1163/156856897X00357
Bearse, Marcus A (2007) Principles and Practice of Clinical Electrophysiology of Vision, 2nd ed. Optometry Vision Sci 84(9):825. http://doi.org/10.1097/opx.0b013e318155a94e
Odom JV, Bach M, Brigell M, Holder GE, McCulloch DL, Mizota A, Tormene AP, International Society for Clinical Electrophysiology of V (2016) ISCEV standard for clinical visual evoked potentials: (2016 update). Doc Ophthalmol 133(1):1–9. https://doi.org/10.1007/s10633-016-9553-y
Di Russo F, Spinelli D (1999) Electrophysiological evidence for an early attentional mechanism in visual processing in humans. Vision Res 39(18):2975–2985. https://doi.org/10.1016/s0042-6989(99)00031-0
Yan W, Xu G, Chen L, Zheng X (2019) Steady-state motion visual evoked potential (SSMVEP) enhancement method based on time-frequency image fusion. Comput Intell Neurosci 2019:9439407. https://doi.org/10.1155/2019/9439407
Han C, Xu G, Xie J, Chen C, Zhang S (2018) Highly interactive brain-computer interface based on flicker-free steady-state motion visual evoked potential. Sci Rep 8(1):5835. https://doi.org/10.1038/s41598-018-24008-8
Martin Bland J, Altman D (1986) Statistical Methods for Assessing Agreement between Two Methods of Clinical Measurement. The Lancet 327(8476):307–310. https://doi.org/10.1016/s0140-6736(86)90837-8
Yan W, Xu G, Xie J, Li M, Dan Z (2018) Four novel motion paradigms based on steady-state motion visual evoked potential. IEEE Trans Biomed Eng 65(8):1696–1704. https://doi.org/10.1109/TBME.2017.2762690
Acknowledgements
Supported by the grants from the National Natural Science Foundation of China (NSFC-51775415) and the Special Guidance Funds for the Construction of World-class Universities (Disciplines) and Characteristic Development in Central Universities (PY3A071).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Statement of human rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Statement on the welfare of animals
No animals were used in this research.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zheng, X., Xu, G., Wu, Y. et al. Comparison of the performance of six stimulus paradigms in visual acuity assessment based on steady-state visual evoked potentials. Doc Ophthalmol 141, 237–251 (2020). https://doi.org/10.1007/s10633-020-09768-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10633-020-09768-x