Abstract
Purpose
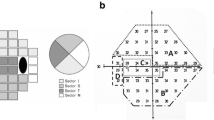
To investigate the possible changes in retinal nerve fiber layer (RNFL) by optic coherence tomography and in the amplitudes and peak times (PTs) in pattern visual evoked potential (pVEP) and to compare them in obstructive sleep apnea syndrome (OSAS).
Methods
This prospective study included patients with mild OSAS (n = 30), severe OSAS (n = 30), and 30 control subjects. All patients were assessed after obtaining the approval from our hospital’s ethics committee.
Results
There was no difference in age and gender between the groups (p = 0.184, p = 0.954). By analysis of variance, there was a significant difference in RNFL values among patients with mild OSAS, severe OSAS, and control for three measures of RNFL (average p = 0.044, nasal p = 0.003, inferior p = 0.027). In severe OSAS group, nasal and inferior quadrants of the RNFL were found to be thinner than the control group (p = 0.008, p = 0.031). We showed that the PT of P100 and N145 was prolonged in severe OSAS compared to the control group (p < 0.001) and that PT of P100 was prolonged in mild OSAS compared to the control group (p < 0.05). The amplitude of N75-P100 was significantly decreased in patients with both severe OSAS and mild OSAS compared to the control group (p < 0.001). Correlation of RNFL and pVEP values showed that the inferior quadrant RNFL thickness is correlated with both P100 and N145 PTs (r = 0.271*, p = 0.036 and r = 0.290*, p = 0.043, respectively) and N75-P100 amplitude (r = 0.378**, p = 0.003) in severe OSAS group.
Conclusions
In mild and severe stages of the disease, edema and inflammation were evident and VEP PT and amplitudes were affected in both groups. Furthermore, thinning in RNFL in the severe stage of the disease might be associated with higher atrophy levels and prolonged exposure to hypoxia.

Similar content being viewed by others
References
Guilleminault C, Tilkian A, Dement WC (1976) The sleep apnea syndromes. Ann Rev Med 27:465–484
Stradling JR, Crosby JH (1991) Predictors and prevalence of obstructive sleep apnoea and snoring in 1001 middle aged men. Thorax 46(2):85–90
Kales A, Cadieux RJ, Bixler EO et al (1985) Severe obstructive sleep apnea—I: onset, clinical course, and characteristics. J Chronic Dis 38(5):419–425
American Academy of Sleep Medicine (1999) Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. The Report of an American Academy of Sleep Medicine Task Force. Sleep 22:667–689
Jordan A, Wellman A, Heinzer R et al (2007) Mechanisms used to restore ventilation after partial upper airway collapse during sleep in humans. Thorax 62:861–867
Lee W, Nagubadi S, Kryger M et al (2008) Epidemiology of obstructive sleep apnea: a population-based perspective. Expert Rev Respir Med 2:349–364
Beebe D, Gozal D (2002) Obstructive sleep apnea and the prefrontal cortex: towards a comprehensive model linking nocturnal upper airway obstruction to daytime cognitive and behavioral deficits. J Sleep Res 11:1–6
Wang W, He M, Huang W (2017) Changes of retinal nerve fiber layer thickness in obstructive sleep apnea syndrome: a systematic review and meta-analysis. Curr Eye Res 42(5):796–802
Sun CL, Zhou LX, Dang Y et al (2016) Decreased retinal nerve fiber layer thickness in patients with obstructive sleep apnea syndrome: a meta-analysis. Med (Baltim) 95(32):e4499
Liguori C, Palmieri MG, Pierantozzi M et al (2016) Optic Nerve dysfunction in obstructive sleep apnea: an electrophysiological study. Sleep 39(1):19–23
Fraser CL (2014) Obstructive sleep apnea and optic neuropathy: is there a link? Curr Neurol Neurosci Rep 14:465
Tsang C, Chong S, Ho C et al (2006) Moderate to severe obstructive sleep apnoea patients is associated with a higher incidence of visual field defect. Eye 20:38–42
Kargi S, Altin R, Koksal M et al (2005) Retinal nerve fibre layer measurements are reduced in patients with obstructive sleep apnoea syndrome. Eye 19:575–579
Leroux les Jardins G, Glacet-Bernard A, Lasry S et al (2009) Retinal vein occlusion and obstructive sleep apnea syndrome. J Fr Ophtalmol 32(420–424):4
Kloos P, Laube I, Thoelen A (2008) Obstructive sleep apnea in patients with central serous chorioretinopathy. Graefes Arch Clin Exp Ophthalmol 246(1225–1228):5
Jain AK, Kaines A, Schwartz S (2010) Bilateral central serous chorioretinopathy resolving rapidly with treatment for obstructive sleep apnea. Graefes Arch Clin Exp Ophthalmol 248:1037–1039
Waller E, Bendel R, Kaplan J (2008) Sleep disorders and the eye. Mayo Clin Proc 83:1251–1261
Blum AS, Rutkove SB (eds) (2007) The clinical neurophysiology primer. Humana Press Inc., Totowa, pp 461–474
American Academy of Sleep Medicine (2014) International classification of sleep disorders, 3rd edn. American Academy of Sleep Medicine, Darien
Kushida CA, Littner MR, Morgenthaler T et al (2005) Practice parameters for the indications for polysomnography and related procedures: an update for 2005. Sleep 28:499–521
Odom JV, Bach M, Brigell M, Holder GE, McCulloch DL, Mizota A, Tormene AP (2016) International Society for Clinical Electrophysiology of Vision. ISCEV standard for clinical visual evoked potentials: (2016 update). Doc Ophthalmol 133(1):1–9. https://doi.org/10.1007/s10633-016-9553-y
Fletcher EC (2003) Sympathetic overactivity in the etiology of hypertension of obstructive sleep apnea. Sleep 26:15–19
Kato M, Roberts-Thomson P, Phillips BG et al (2000) Impairment of endothelium dependent vasodilation of resistance vessels in patients with obstructive sleep apnea. Circulation 102:2607–2610
Priou P, Gagnadoux F, Tesse A et al (2010) Endothelial dysfunction and circulating microparticles from patients with obstructive sleep apnea. Am J Pathol 177:974–983
Marzoli SB, Ciasca P, Curone M et al (2013) Neurol Sci. 34(Suppl 1):S143–S155
Lin PW, Friedman M, Lin HC et al (2011) Decreased retinal nerve fiber layer thickness in patients with obstructive sleep apnea/hypopnea syndrome. Graefes Arch Clin Exp Ophthalmol 249(4):585–593
Casas P, Ascaso FJ, Vicente E et al (2013) Retinal and optic nerve evaluation by optical coherence tomography in adults with obstructive sleep apnea-hypopnea syndrome (OSAS). Graefes Arch Clin Exp Ophthalmol 251(6):1625–1634
Moghimi S, Ahmadraji A, Sotoodeh H et al (2013) Retinal nerve fiber thickness is reduced in sleep apnea syndrome. Sleep Med 14:53–57
Sagiv O, Fishelson-Arev T, Buckman G et al (2014) Retinal nerve fiber layer thickness measurements by optical coherence tomography in patients with sleep apnea syndrome. Clin Exp Ophthalmol 42:132–138
Huseyinoglu N, Ekinci M, Ozben S et al (2014) Optic disc and retinal nerve fiber layer parameters as indicators of neurodegenerative brain changes in patients with obstructive sleep apnea syndrome. Sleep Breath 18:95–102
Shiba T, Takahashi M, Sato Y et al (2014) Relationship between severity of obstructive sleep apnea syndrome and retinal nerve fiber layer thickness. Am J Ophthalmol 157:1202–1208
Calvo P, Ferrandez B, Ferreras A et al (2012) Retinal nerve fiber layer thickness alterations in patients with obstructive sleep apnea. Arch Soc Esp Oftalmol 87:1–2
Ferrandez B, Ferreras A, Calvo P et al (2014) Retinal sensitivity is reduced in patients with obstructive sleep apnea. Invest Ophthalmol Vis Sci 55:7119–7125
Salzgeber R, Iliev ME, Mathis J (2014) Do optic nerve head and visual field parameters in patients with obstructive sleep apnea syndrome differ from those in control individuals? Klin Monbl Augenheilkd 231:340–343
Zengin MO, Tuncer I, Karahan E (2014) Retinal nerve fiber layer thickness changes in obstructive sleep apnea syndrome: one year follow-up results. Int J Ophthalmol 7(4):704–708
Bayhan HA, Bayhan AS (2014) Choroidal thickness alterations in obstructive sleep apnea-hypopnea syndrome (OSAS). Eye (Lond) 28(11):1387
Kalesnykas G, Tuulos T, Uusitalo H et al (2008) Neurodegeneration and cellular stress in the retina and optic nerve in rat cerebral ischemia and hypoperfusion models. Neuroscience 155(3):937–947
LoPachin RM Jr, Stys PK (1995) Elemental composition and water content of rat optic nerve myelinated axons and glial cells: effects of in vitro anoxia and reoxygenation. J Neuroscience 15(10):6735–6746
Walsh P, Kane N, Butler S (2005) The clinical role of evoked potentials. J Neurol Neurosurg Psychiatry 76(Suppl 2):ii16–ii22
Holder GE (2004) Electrophysiological assessment of optic nerve disease. Eye (Lond) 18:1133–1143
Kerr CC, Rennie CJ, Robinson PA (2009) Deconvolution analysis of target evoked potentials. J Neurosci Methods 179:101–110
Alshowaeir D, Yannikas C, Garrick R et al (2015) Multifocal VEP assessment of optic neuritis evolution. Clin Neurophysiol 126:1617–1623
Nadeem R, Molnar J, Madbouly EM et al (2013) Serum inflammatory markers in obstructive sleep apnea: a meta-analysis. J Clin Sleep Med 9:1003–1012
Chen HL, Lin HC, Lu CH et al (2017) Systemic inflammation and alterations cerebral blood flow in obstructive sleep apnea. J Sleep Res 26(6):789–798
Sohmer H, Freeman S, Malachi S (1986) Multi-modality evoked potentials in hypoxaemia. Electroencephalogr Clin Neurophysiol 64:328–333
Huang H, Shen H, Qin Z et al (2016) The analysis of pattern visual evoked potential in obstructive sleep apnea syndrome. Zhonghua Jie He He Hu Xi Za Zhi 39(9):709–713
Liguori C, Placidi F, Palmieri MG et al (2018) Continuous positive airway pressure treatment may improve optic nerve function in obstructive sleep apnea: an electrophysiological study. J Clin Sleep Med 14(6):953–958
Rodarte C, Hood DC, Yang EB et al (2006) The effects of glaucoma on the latency of the multifocal visual evoked potential. Br J Ophthalmol 90(9):1132–1136
Funding
This study was supported by Scientific Researches Project of Celal Bayar University (2018-105).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Ass. Prof. Ayşın Kısabay Ak declares that she has no conflict of interest. Dr.Melike Batum declares that she has no conflict of interest. Ass. Prof. Tuğba Göktalay declares that she has no conflict of interest. Dr. Hüseyin Mayalı declares that he has no conflict of interest. Prof. Dr. Deniz Selçuki declares that she has no conflict of interest. Prof. Dr. Emin Kurt declares that he has no conflict of interest. Prof. Dr. Hikmet Yılmaz declares that he has no conflict of interest.
Ethical approval
All procedures performed in the studies involving human participants were in accordance with the ethical standards of the Celal Bayar University Medical Faculty Ethics Committee (Approval Date: 14 March 2018, Approval Number: 20.478.486) and with Helsinki Declaration (1964) and its later amendments or comparable ethical standards.
Statement of human rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Celal Bayar University Medicine Faculty and with the 1964 Helsinki Declaration and its later amendments.
Statement on the welfare of animals
This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kısabay Ak, A., Batum, M., Göktalay, T. et al. Evaluation of retinal fiber thickness and visual pathways with optic coherence tomography and pattern visual evoked potential in different clinical stages of obstructive sleep apnea syndrome. Doc Ophthalmol 141, 33–43 (2020). https://doi.org/10.1007/s10633-020-09749-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10633-020-09749-0