Abstract
Purpose
To report a case of a child with strabismus and delayed discovery of a metallic intraocular foreign body with good recovery of visual acuity and stereopsis with 36-month follow-up.
Methods
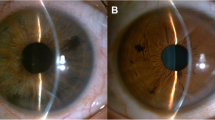
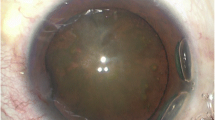
A 4-year-old girl was evaluated due to exotropia of right eye initiated 9 months before with progressive worsening. Visual acuity was 1.00 logMAR (20/200) in the right eye and 0.00 logMAR (20/20) in the left eye. Anterior segment evidenced a small paracentral corneal leukoma, posterior synechia and mild lens opacity in the temporal quadrant only in the right eye. Fundus examination in the right eye identified the presence of an intraocular foreign body, with appearance of metallic components surrounded by retinal pigmented endothelial cells atrophy. Full-field electroretinography (ERG) showed reduced amplitudes and delayed implicit times for both rods and cones in the affected eye. All tests were normal in the fellow eye.
Results
Pars plana vitrectomy was promptly performed in the right eye, followed by phacoemulsification with intraocular lens implantation 4 months later due to worsening of the lens opacification. The full-field ERG was repeated after the surgical procedures. The ERG showed mild worsening of all responses in the right eye. After 36 months of follow-up, visual acuity was 0.20 logMAR (20/32) with improvement of the ocular misalignment and with 60 s of arc stereopsis with ERG responses unchanged.
Conclusion
In this young girl perforating ocular trauma with metallic material was lately diagnosed with strabismus as a sign of alert. Prompt surgical intervention and proper management were essential to provide reasonable visual function including some degree of stereopsis, even though retinal dysfunction characterized by ERG was persistent.







Similar content being viewed by others
References
Li X, Zarbin MA, Bhagat N (2015) Pediatric open globe injury: a review of the literature. J Emerg Trauma Shock 8(4):216–223
Cao H, Li L, Zhang M, Li H (2013) Epidemiology of pediatric ocular trauma in the Chaoshan Region, China, 2001–2010. PLoS One. https://doi.org/10.1371/journal.pone.0060844
Loporchio D, Mukkamala L, Gorukanti K, Zarbin M, Langer P, Bhagat N (2016) Intraocular foreign bodies: a review. Surv Ophthalmol 61(5):582–596
Mostafavi D, Olumba K, Shrier EM (2014) Fiberglass intraocular foreign body with no initial ocular symptoms. Retin Cases Brief Rep 8(1):10–12
Yang X, Liu C, Liu L, Zhang L (2017) A missed diagnosis of multiple intraocular foreign bodies for 21 years. Contact Lens Anterior Eye 40(6):432–435
Marmor MF, Fulton AB, Holder GE, Miyake Y, Brigell M, Bach M et al (2009) ISCEV standard for full-field clinical electroretinography (2008 update). Doc Ophthalmol 118(1):69–77
Minkowski JS, Palese M, Guyton DL (1983) Potential acuity meter using a minute serial pinhole aperture. Ophthalmology 90:1360–1368
Brophy M, Sinclair SA, Hostetler SG, Pediatric XH (2006) Eye injury-related hospitalizations in the United States. Pediatrics 117:1263–1271
Minderhoud J, van Nispen RM, Heijthuijsen AAAM (2016) Epidemiology and etiology of childhood ocular trauma in the Republic of Suriname. Acta Ophthalmol 94:479–484
Liu CCH, Tong JMK, Li PSH, Li KK (2017) Epidemiology and clinical outcome of intraocular foreign bodies in Hong Kong: a 13-year review. Int Ophthalmol 37(1):55–61
Meier P (2010) Combined anterior and posterior segment injuries in children: a review. Graefes Arch Clin Exp Ophthalmol 248:1207–1219
Faure C, Gocho K, Le Mer Y, Sahel JA, Paques M, Audo I (2014) Functional and high resolution retinal imaging assessment in a case of ocular siderosis. Doc Ophthalmol 128(1):69–75
Kannan NB, Adenuga OO, Rajan RP, Ramasamy K (2016) Management of ocular siderosis: visual outcome and electroretinographic changes. J Ophthalmol. https://doi.org/10.1155/2016/7272465
Hope-Ross M, Mahon GJ, Johnston PB (1993) Ocular siderosis. Eye 7:419–425
Sneed RS, Weingeist TA (1990) Management of siderosis bulbi due to a retained iron containg intraocular foreign body. Ophthalmology 97:375–379
Fuente Garcia C, Gonzalez-Lopez JJ, Munoz-Negrete FJ, Rebolleda G (2018) The diagnostic usefulness of the negative electroretinogram. Arch Soc Esp Oftalmol 93(3):126–135
Gelfand BD, Wright CB, Kim Y et al (2015) Iron toxicity in the retina requires Alu RNA and the NLRP3 inflammasome. Cell Rep 11(11):1686–1693
Declercq SS, Meredith PC, Rosenthal AR (1977) Experimental siderosis in the rabbit: correlation between electroretinography and histopathology. Arch Ophthalmol 95(6):1051–1058
Tawara A (1986) Transformation and cytotoxicity of iron in siderosis bulbi. Invest Ophthalmol Vis Sci 27(2):226–236
Acknowledgements
Vinicius Bergamo, Mariana Wisnesky.
Author information
Authors and Affiliations
Contributions
FP was involved in writing the article, analysis and interpretation. LM was involved in surgical expertise, analysis and interpretation, final approval of the article. Paula Yuri Sacai involved in electrophysiological testing, analysis and interpretation, final approval of the article. SRS was involved in analysis and interpretation, final approval of the article. LSJ involved in surgical expertise, final approval of the article. AB was involved in electrophysiological testing, analysis and interpretation, final approval of the article.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Ethical approval
This study was approved by the Research Ethics Committee of the Federal University of Sao Paulo and adhered to the tenets of the Declaration of Helsinki.
Informed consent
The parents have given their written informed consent.
Statement of human rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Statement on the welfare of animals
This article does not contain any studies with animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pereira, F., Matieli, L., Sacai, P.Y. et al. Electrophysiological findings in delayed discovery of a metallic intraocular foreign body in a child: case report. Doc Ophthalmol 139, 227–234 (2019). https://doi.org/10.1007/s10633-019-09708-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10633-019-09708-4