Abstract
Background
Gliclazide is a potential anti-cancer drug candidate for preventing carcinogenesis. However, the effect of gliclazide on colitis-associated colorectal cancer remains unknown.
Aims
We aimed to evaluate whether gliclazide plays a protective role in colitis-associated colorectal cancer and the underlying molecular mechanism.
Methods
The administration of azoxymethane (AOM) followed by dextran sulfate sodium (DSS) aimed to induce colitis-associated colorectal cancer in mice. C57BL mice were gavaged with gliclazide (6 mg/kg by gavage 5 days a week) for 12 weeks immediately following AOM administration. After sacrificing the mice, colon tissues were measured for tumor number and tumor burden. The proliferation- and inflammation-related molecular mechanisms were explored.
Results
The administration of gliclazide significantly reduced the tumor number and tumor burden in mice. Cell proliferation decreased in the gliclazide group compared with the control group, as indicated by reduced Ki-67 expression. Furthermore, gliclazide alleviated colonic inflammation, significantly decreased pro-inflammatory factor TNF-α levels and increased anti-inflammatory factor IL-10 levels in vivo. In vivo and vitro, it was shown that gliclazide increased the level of phospho-AMPK (p-AMPK) and inhibited NF-κB activity. Further studies demonstrated that the inhibition of NF-κB activity induced by gliclazide was mediated by p-AMPK in vitro.
Conclusions
Gliclazide effectively alleviated colonic inflammation and prevented colonic carcinogenesis in an AOM–DSS mouse model by modulating the AMPK-NF-κB signaling pathway. Thus, gliclazide holds potential as a chemopreventive agent for colitis-associated colorectal cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Inflammatory bowel disease (IBD) is a chronic relapsing inflammatory disorder of the gastrointestinal tract, which mainly includes ulcerative colitis (UC) and Crohn’s disease (CD). The risk of colorectal cancer in patients with IBD is greatly increased compared to that in the general population. This specific form of cancer is commonly referred to as colitis-associated colorectal cancer (CAC). The median time of malignant transformation is approximately 15–20 years [1]. Therefore, chemopreventive interventions are important for the long-term management of this cancer. It is well known that glucocorticoid, mesalazine, and immunosuppressive agents can be effective to induce or maintain inflammation remission [2]. However, there is still ongoing debate regarding the effectiveness of various agents in preventing the transformation of colonic inflammation into cancer. Currently, the availability of well-established and safe agents for the prevention of CAC remains quite limited.
Gliclazide is a second-generation sulfonylurea that is widely used as a therapeutic drug for diabetes. Interestingly, several recent studies have suggested that gliclazide can reduce colorectal cancer risk and mortality in patients with type 2 diabetes [3, 4]. It was reported that gliclazide decreased colorectal cancer incidence in patients with type 2 diabetes, while other sulfonylureas increased the colorectal cancer incidence [3]. Moreover, it was reported that cancer mortality was markedly reduced in diabetic patients receiving gliclazide treatment compared with glibenclamide users, and none of the patients treated with gliclazide monotherapy died from cancer during the follow-up [4]. These results highlight the additional benefits of gliclazide beyond its primary role in reducing glucose levels. However, the effect of gliclazide on colonic inflammation-cancer transformation remains unknown. In the current study, we demonstrated that gliclazide significantly prevented CAC in mice by alleviating colonic inflammation and modulating the AMPK-NF-κB signaling pathway.
Materials and Methods
Mouse Model, Gliclazide Intervention Protocol, and Reagents
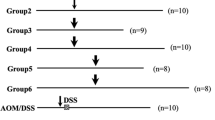
Colitis-associated carcinogenesis was established using an azoxymethane (AOM)-dextran sulfate sodium (DSS) mouse model. Male C57BL/6 mice (6 to 8-weeks-old) were injected intraperitoneally with 12.5 mg/kg AOM (Sigma, A2853) at the beginning of the experiment. One week later, 2.5% (w/v) DSS (MP Biomedicals, 160,110) was administered in drinking water for five consecutive days. To evaluate the chemopreventive effect of gliclazide (MCE, S1702), the mice were divided into four groups for the study. Groups 1 and 2 served as controls, while groups 3 and 4 were used to induce CAC using AOM and DSS treatment. Immediately after AOM administration (0 week), the mice in groups 2 and 4 started to receive gliclazide at 6 mg/kg by gavage 5 days a week for 12 weeks. On the other hand, the mice in groups 1 and 3 received the same amount of olive oil which is the vehicle for gliclazide (Fig. 1A). The mice were sacrificed at the end of week 12. The colons (from the ileocecal junction to the anal verge) and serum were collected and stored for subsequent assays. The number and size of the colonic neoplasias were recorded.
Gliclazide inhibited colon carcinogenesis in an AOM–DSS mouse model. A Experimental protocol and intervention schedule of gliclazide in the CAC mouse model as detailed in “Materials and Methods” section. The mice in groups 2 and 4 were gavaged with gliclazide immediately following AOM treatment until the mice were sacrificed, while the mice in groups 1 and 3 were gavaged with the same amount of olive oil. B Representative pictures of H&E staining of the mouse colon from the control and AOM–DSS groups. Scale bars represent 100 μm. C Representative macroscopic view of the mouse colon in each group. The formation of colonic tumor was evaluated as D tumor number and E tumor burden in each group. Data were presented as mean ± SD (n = 6–8). *P < 0.05
Colitis was established using the DSS mouse model. The male C57BL/6 mice (6 to 8-weeks-old) were administered 2.5% DSS in drinking water for five consecutive days. The mice were divided into three groups. Colitis was induced in groups 2 and 3 by DSS treatment, but not for group 1, which served as a control. At the beginning of the experiment (day 0), the mice in group 3 were treated with 4.29 mg/kg gliclazide by gavage for 7 days to evaluate the anti-inflammatory effect of gliclazide, while the mice in groups 1 and 2 received the same amount of olive oil (Fig. 2A). The mice were sacrificed on day 7. The colons (from the ileocecal junction to the anal verge) and serum were collected and stored for subsequent assays. Histological inflammation was analyzed and scored by an experienced pathologist who was blinded to the animal groups. This study was approved by the Experimental Animal Ethics Committee of the Second Hospital of Shandong University.
Effect of gliclazide administration on inflammation after DSS induction. A Experimental protocol and intervention schedule of short-term gliclazide in DSS mouse model as detailed in “Materials and Methods” section. B Representative pictures of H&E staining of the mouse colon from colitis and colitis/gliclazide group. Scale bars represent 100 μm. C Histological inflammation scores of colon tissue were assessed in colitis and colitis/gliclazide groups. D The expressions of TNF-α, IL-1β, IL-10, and COX-2 mRNA in the mouse colon were detected with real-time polymerase chain reaction. E The levels of pro-inflammatory cytokines (CCL20 and TNF-α) in mouse colon tissues were measured by ELISA. F The levels of anti-inflammatory cytokines (IL-10 and IL-13) in mouse colon tissues were measured by ELISA. Data were presented as mean ± SD (n = 5–8). *P < 0.05 and **P < 0.01
AOM and mouse monoclonal antibodies against β-actin were purchased from Sigma-Aldrich Corporation (St. Louis, MO, USA). DSS (molecular weight 36–50 kDa) was purchased from MP Biomedicals (Santa Ana, CA, USA). Rabbit polyclonal antibody against Ki-67 was obtained from Abcam Co. Ltd (Cambridge, UK), rabbit polyclonal antibody against phospho-AMPK (p-AMPK) (Thr172) was obtained from Affinity Biosciences (Cincinnati, OH, USA), and rabbit polyclonal antibody against AMPK was obtained from Abclonal Technology (Woburn, MA, USA). Gliclazide was provided by MedChemExpress (MCE, NJ, USA). Compound C, a specific AMPK blocker, was provided by Calbiochem (Ka Jolla, CA, USA).
Cell Culture
The human colon cancer cell lines SW480 was obtained from the American Type Culture Collection (ATCC). SW480 cells were cultured in Dulbecco’s modified Eagle’s medium/F12 (Hyclone) supplemented with 10% fetal bovine serum (Hyclone) and 1% penicillin–streptomycin solution (Hyclone). Cells were maintained at 37 °C, 95% humidity, and 5% carbon dioxide. The cells were seeded and incubated for 24 h for attachment. After the treatment with 1000 nM gliclazide (MCE, S1702) or control for 24 h or 48 h, the cells were collected for subsequent experiments.
Cell Proliferation Assay
Cell proliferation was evaluated using the Cell counting kit-8 (CCK8) assay following the manufacturer’s instructions. A total of 104 cells were seeded into each well of 96-well plates. After 24 h, the medium was replaced with fresh medium containing serial dilutions of gliclazide (10–1000 nM). The cells were incubated at 37 °C for an additional 48 h. For the CCK8 assay, 10 μl of CCK8 (MCE, NJ, USA) solution was added per well. After 2 h, the absorbance was detected at 450 nm using a microplate reader.
RNA Isolation, Reverse Transcription, and Real-Time PCR
Total RNA was isolated from mouse colon tissues or cells using Trizol reagent (Invitrogen). After treatment with DNase I, RNA was reverse transcribed into cDNA using the Thermo Scientific Maxima First Strand cDNA Synthesis Kit. Real-time quantitative PCR was performed using a Bio-Rad PCR System. The relative levels of mRNA transcripts were normalized to GAPDH (glyceraldehyde-3-phosphate dehydrogenase) expression. Primers for the mice were as follows: TNF-α forward, 5′-CCCTCACACTCAGATCATCTTCT-3′ and reverse, 5′-GCTACGACGTGGGCTACAG-3′. IL-1β forward, 5′-GCAACTGTTCCTGAACTCAACT-3′ and reverse, 5′-ATCTTTTGGGGTCCGTCAACT-3′. IL-10 forward, 5′-GCTCTTACTGACTGGCATGAG-3′ and reverse, 5′-CGCAGCTCTAGGAGCATGTG-3′. COX-2 forward, 5′-TTCAACACACTCTATCACTGGC-3′ and reverse, 5′-AGAAGCGTTTGCGGTACTCAT-3′. Ki-67 forward, 5′-ATCATTGACCGCTCCTTTAGGT-3′ and reverse, 5′-GCTCGCCTTGATGGTTCCT-3′. AMPK forward, 5′-GTCAAAGCCGACCCAATGATA-3′ and reverse, 5′-CGTACACGCAAATAATAGGGGTT-3′. GAPDH forward, 5′-AACTTTGGCATTGTGGAAGG-3′ and reverse, 5′-ACACATTGGGGGTAGGAACA-3′. Primers for humans were as follows: AMPK forward, 5′-TTGAAACCTGAAAATGTCCTGCT-3′ and reverse, 5′-GGTGAGCCACAACTTGTTCTT-3′. GAPDH forward, 5′-AGCCACATCGCTCAGACAC-3′ and reverse, 5′-GCCCAATACGACCAAATCC-3′.
Western Blot
First, cells were lysed in ice-cold lysis buffer supplemented with protease inhibitor cocktail and protein phosphatase inhibitor to extract total proteins. Protein concentration was determined using a bicinchoninic acid assay kit (Applygen, Beijing, China), and the protein was boiled in 1 × SDS loading buffer. Lysates were separated by 10% sodium dodecylsulfate-polyacrylamide gel electrophoresis (SDS-PAGE) and transferred to polyvinylidene difluoride (PVDF) membranes. The membranes were blocked with 5% non-fat dry milk for 1 h and then incubated overnight at 4 °C with primary antibodies against phospho-AMPK (p-AMPK) (Thr172) (Affinity Biosciences, 1:500), AMPK (ABclonal, 1:500), or β-actin (Sigma, 1:10,000). After three washes for 10 min, the membranes were incubated with a horseradish peroxidase-linked secondary antibody (Cell Signaling Technology) for 1 h. The signal was visualized with ECL (Millipore).
Transient Transfection
SW480 cells in 6-well plates were transfected with siAMPK using 5 μl of Lipofectamine 2000 (Invitrogen) according to the manufacturer’s instructions. The siRNA targeting human AMPK and control siRNA were synthesized by GenePharma (Suzhou, Jiangsu, China). Following transfection, the cells were collected for RT-PCR and Western blotting as mentioned above, to ensure knockdown efficiency.
Luciferase Assay
SW480 cells in 24-well plates were transfected with wild-type NF-κB luciferase reporter (200 ng) and pRL-TK (2 ng). The transfection agent, Lipofectamine 2000 (Invitrogen), was incubated in serum-free medium for 20 min before being added to the cells and then incubated for an additional 6 h. Following treatment with 1000 nM gliclazide for 24 h or 48 h, cellular lysates were collected for luciferase activity measurement using a Dual-Luciferase assay kit (Promega). All data were normalized using pRL-TK.
NF-κB p65 Activity Assay
Colon tissues were subjected to nuclear-cytoplasmic fractionation using a nuclear extraction kit (Cayman Chemical, Ann Arbor, Michigan, USA). Isolated nuclear protein fractions were then used to assess the DNA-binding activity of NF-κB using a NF-κB (p65) transcription factor assay kit (Cayman Chemical) according to the manufacturer’s instructions.
Hematoxylin–Eosin (H&E) Staining and Immunohistochemistry
Mouse colon tissues were fixed in neutral buffered formalin for 24 h and then embedded in paraffin. Three-micron-thick tissue sections were cut and stained with H&E. Colon tissue sections were dewaxed and rehydrated in xylene and graded concentrations of ethanol solutions, followed by antigen retrieval and endogenous peroxidase activity block. The sections were incubated with primary antibodies, followed by incubation with the appropriate secondary antibodies. Anti-Ki-67 (Abcam, 1:1000) and anti-p-AMPK (Thr172) (Affinity Biosciences, 1:1000) antibodies were used as the primary antibodies. The sections were detected using Polymer Detection System reagents (ZSGB-BIO Company, Beijing, China) and DAB (ZLI-9019).
ELISA
ELISA (RayBiotech) was performed on the interstitial fluid of the colon to determine CCL20, TNF-α, IL-10, and IL-13 levels according to the manufacturer’s recommendations. Relative levels of CCL20, TNF-α, IL-10, and IL-13 were determined by calculating their values based on the standard curve and subtracting the negative control signal.
Statistics Analysis
Statistical analysis was done with the GraphPad Prism statistical program. Data were analyzed by unpaired Student’s t test between the two groups. Values are expressed as mean ± SD. Statistical significance was set at P < 0.05.
Results
Gliclazide Prevents Colon Carcinogenesis in AOM–DSS Mouse Model
To study the effect of gliclazide on CAC, an AOM–DSS mouse model was established (Fig. 1A). H&E staining revealed that the majority of lesions observed in the mouse colon from the AOM–DSS and AOM–DSS/gliclazide groups were consistent with adenoma, high-grade intraepithelial neoplasia, or carcinoma in situ (Fig. 1B). In contrast, no abnormal findings were observed in the control and gliclazide groups. There was no difference at the histological level between the AOM–DSS and AOM–DSS/gliclazide groups, or between the control and gliclazide groups. Colonic neoplasm was observed in the colon of all mice in the AOM–DSS and AOM–DSS/gliclazide groups, whereas no colonic neoplasm was found in the control and gliclazide groups (Fig. 1C). It was identified that the tumor number and the tumor burden were significantly reduced in the AOM–DSS/gliclazide group compared with the AOM–DSS group (Fig. 1D, E). Thus, the data indicated that the administration of gliclazide significantly reduced tumor formation induced by AOM–DSS in mice.
Gliclazide Alleviates DSS-Induced Colitis and Decreases Pro-inflammatory Factors Levels In Vivo
An increasing number of studies have shown that multiple sulfonylureas including gliclazide, glipizide, and glibenclamide play a role in anti-carcinogenesis by inhibiting inflammation, proliferation, and angiogenesis [5, 6]. To explore the effect of gliclazide on the stage of acute colitis, a DSS mouse model was first established, and then the mice were sacrificed 7 days following the initiation of gliclazide treatment (Fig. 2A). H&E staining highlighted several lesions in the colitis group, including severe damage and necrosis of the intestinal glands, and congested blood vessels with diffuse inflammatory cell infiltration. Furthermore, gliclazide administration significantly improved the histopathological presentation, characterized by intact lining of epithelial layers, mild submucosal edema, and mild inflammatory cell infiltration (Fig. 2B). In the control group, colon sections revealed a normal histopathological structure. The histological inflammation score of the colitis/gliclazide group was significantly lower than that of the colitis group (Fig. 2C). Both pro-inflammatory and anti-inflammatory factor levels were determined to elucidate the mechanism by which gliclazide protects against DSS-induced colon injury. In our study, we detected inflammatory factors (TNF-α, IL-1β, IL-10, CCL20, and IL-13) and COX-2 levels in colon tissues through Real-time PCR and ELISA, which have been reported to be closely associated with the anti-inflammatory effect of gliclazide [7, 8]. We observed a decrease in mRNA and protein levels of the pro-inflammatory cytokine TNF-α, and an increase in levels of the anti-inflammatory cytokine IL-10 in colon tissue in the colitis/gliclazide group compared to the colitis group. However, there were no significant differences between the expression of IL-1β and COX-2 at the mRNA level and the expression of CCL20 and IL-13 at the protein level (Fig. 2D–F). These results suggest that gliclazide has an anti-inflammatory effect in a DSS mouse model in vivo.
Gliclazide Reduces Cell Proliferation in AOM–DSS Mouse Model
To evaluate the effect of gliclazide on cell proliferation, we measured the Ki-67 mRNA expression level, a marker indicative of proliferating cells. Gliclazide reduced the mRNA expression of Ki-67 in the mouse colon tissues (Fig. 3A). Ki-67 staining was also performed. We observed a significant decrease in the Ki-67-posivtive rate within the adenoma region of the AOM–DSS/gliclazide group compared to the AOM–DSS group. However, no significant difference was observed in the non-adenoma region (Fig. 3B). In vitro, treatment with gliclazide (10–1000 nM) for 48 h in SW480 cells resulted in a dose-dependent decrease in cell growth, as measured by the CCK8 assay (Fig. 3C). These data suggest that gliclazide inhibits the proliferation of colitis-associated colon cancer cell.
Effect of gliclazide on cell proliferation of colonic epithelium in the AOM–DSS mouse model. A The expression of Ki-67 mRNA in colon tissues was measured with real-time PCR. B Ki-67 staining in colon tissues was performed with IHC analysis. Scale bars represent 100 μm. C SW480 cells were stimulated with gliclazide (10–1000 nM) for 48 h. CCK8 assay was performed to detect cell proliferation. Data were presented as mean ± SD (n = 5–8). *P < 0.05 and **P < 0.01
Gliclazide Regulates AMPK-NF-κB Signaling Pathway In Vitro
Gliclazide induces AMPK activation and inhibits vascular smooth muscle cell proliferation in a dose- and time-dependent manner [9]. AMPK-NF-κB signaling participates in the pathogenesis of non-alcoholic fatty liver disease, non-alcoholic steatohepatitis, and hepatocellular carcinoma by regulating proliferation, migration, and invasion [10, 11]. However, it is unknown whether gliclazide regulates AMPK-NF-κB signaling in CAC. We observed that the level of p-AMPK was increased following the treatment with gliclazide for 24 h or 48 h in SW480 cells, whereas the total level of AMPK remained unchanged (Fig. 4A). Meanwhile, treatment with gliclazide effectively inhibited p65 NF-κB transcriptional activity in SW480 cells (Fig. 4B). Moreover, AMPK knockdown successfully rescued the inhibitory effect of gliclazide on p65 NF-κB transcriptional activity in SW480 cells (Fig. 4C–E). Compound C, a specific blocker of AMPK, was used to suppress AMPK kinase activity. Treatment of SW480 cells with 10 μM compound C inhibited AMPK phosphorylation, thereby blocking AMPK activation, and rescued the inhibitory effect of gliclazide on p65 NF-κB transcriptional activity (Fig. 4F, G). This further supports that gliclazide regulates the AMPK-NF-κB signaling pathway in vitro.
Gliclazide regulated AMPK-NF-κB signaling pathway in vitro. After stimulation with 1000 nM gliclazide for 24 h or 48 h, the expressions of p-AMPK and AMPK at protein levels (A) and NF-κB luciferase activity (B) were, respectively, measured with Western blot and luciferase assay. C SW480 cells were transfected with siAMPK, which successfully knocked down AMPK expression measured with RT-PCR and Western blot. SW480 cells were transfected with siAMPK, and then the expressions of p-AMPK and AMPK at protein levels (D) and NF-κB luciferase activity (E) were, respectively, measured after stimulation with 1000 nM gliclazide for 48 h. SW480 cells were treated with 10 μM compound C, and then the expressions of p-AMPK and AMPK at protein levels (F) and NF-κB luciferase activity (G) were, respectively, measured after stimulation with 1000 nM gliclazide for 48 h. *P < 0.05
Gliclazide Induces AMPK Phosphorylation and Inhibits NF-κB Activity In Vivo
To confirm whether gliclazide activates AMPK and inhibits NF-κB in vivo, we assessed the mRNA level of AMPK using real-time PCR, protein levels of p-AMPK using immunohistochemistry (IHC), and NF-κB activity using an NF-κB activity assay in colon tissues. No significant difference was observed in the mRNA levels of AMPK between the AOM–DSS and AOM–DSS/gliclazide groups (Fig. 5A). However, IHC analysis demonstrated that gliclazide notably increased p-AMPK levels in vivo (Fig. 5B). NF-κB activity significantly decreased in the AOM–DSS/gliclazide group compared with the AOM–DSS group (Fig. 5C). These findings suggest that gliclazide prevented colitis-associated colon carcinogenesis by inducing phosphorylation of AMPK and inhibiting NF-κB activity in vivo.
Gliclazide induced AMPK phosphorylation and inhibited NF-κB activity in the AOM–DSS mouse model. A The relative mRNA level of AMPK was measured with RT-PCR in mouse colon tissues. B IHC analysis of p-AMPK expression in mouse colon tissues was performed. Scale bars 100 μm. C NF-κB activity in the mouse colon was detected by the NF-κB p65 activity assay. Data were presented as mean ± SD (n = 5–8). *P < 0.05
Discussion
IBD patients carry an increased risk for the development of colorectal cancer (CRC), especially those with a greater duration and those with extensive amounts of inflammation. Pro-inflammatory effects play a crucial role in the transformation of colonic inflammation into cancer. As shown in an animal mouse model, the inhibition of COX-2 and NF-κB signaling contributed to the prevention of CAC [12]. It has been reported that gliclazide inhibited tumor necrosis factor (TNF) production and inhibited TNF bioactivity and immunoreactivity in mouse serum [13]. Furthermore, gliclazide prevents 5-FU-induced oral mucositis by inhibiting NF-κB signaling and decreasing the levels of TNF-α and IL-1β [7]. For the first time, we found that gliclazide significantly decreased tumor number and tumor burden in an AOM–DSS mouse model, suggesting that gliclazide may have a preventive effect on colitis-associated colon cancer initiation. In our study, we also found that supplemental gliclazide alleviated colonic inflammation, decreased levels of the pro-inflammatory mediator TNF-α, and increased levels of the anti-inflammatory mediator IL-10 level in an acute colitis mouse model. It is well accepted that the severity of colitis correlates with the risk of colon cancer. Thus, it is likely that the reduction in colitis severity leads to a decrease in both tumor number and tumor burden.
An expanding body of epidemiological and preclinical studies provides evidence that gliclazide exerts anti-cancer effects in various cancers such as colon cancer, lung adenocarcinoma, and pancreatic carcinoma [14, 15]. Recently, it was reported that gliclazide induces cell cycle arrest and inhibits proliferation in lung adenocarcinoma, possibly by targeting specific genes [16]. However, it remains unknown whether gliclazide has a role in inhibiting the proliferation of colitis-associated colon cancer cells. In our study, we demonstrated that gliclazide significantly decreased the expression of Ki-67 in an AOM–DSS mouse model and in vitro. These results suggest that gliclazide may inhibit the proliferation of colitis-associated colon cancer cells.
AMPK is a critical regulator of cellular energy and is closely associated with colon cancer cell initiation and proliferation [17, 18]. It was reported that AMPK was highly expressed in CRC samples using IHC [19]. Furthermore, activated AMPK inhibited colon cancer cell proliferation and tumor growth in a xenograft tumor model and in vitro [18, 20]. Currently, the molecular mechanisms by which gliclazide plays a protective role in colon cancer remain poorly understood. In the current study, our novel finding was that gliclazide significantly increased p-AMPK levels in the AOM–DSS mouse model and colon cancer cells, suggesting that gliclazide could activate AMPK signaling. It has been reported that LKB1 or CaMKKβ mediated the gliclazide-induced activation of AMPK signaling which was associated with cell proliferation [9]. However, it remains unknown whether LKB1 or CaMKKβ mediates gliclazide-induced activation of AMPK signaling in preventing colonic inflammation-cancer transformation, and it requires further investigation. It is well known that NF-κB signaling participates in colonic inflammation-cancer transformation and has a major role in proliferation, invasion, and metastasis in cancer cells [21, 22]. NF-κB can be inactivated by AMPK, both directly and indirectly [23, 24]. It has been showed that AMPK/NF-κB signaling had a major role in curcumin suppressing colon cancer cell proliferation and invasion [25]. Here, we found that gliclazide treatment decreased NF-κB activity in an AOM–DSS mouse model and in vitro. Importantly, we further demonstrated in vitro that p-AMPK mediated gliclazide-induced inhibition of NF-κB activity. Based on these data, we propose that gliclazide inhibits p-AMPK-mediated NF-κB activation, possibly resulting in the suppression of colitis-associated colon cancer cell proliferation. However, due to AMPK-NF-κB signaling pathway is detected within the formed tumors, it does not really explain what gliclazide may be doing at the time of colitis-associated colon cancer initiation.
In summary, gliclazide was shown to be a chemoprophylactic agent against CAC via AMPK-mediated inhibition of NF-κB in colon cancer cells. The upregulation of p-AMPK plays a significant role in the inhibitory effect of gliclazide on NF-κB in both in vivo and in vitro settings. However, the mechanism by which gliclazide prevents CAC requires further investigation. Moreover, gliclazide as an anti-cancer drug candidate still needs to be explored in prospective intervention studies.
References
Cremer A, Demetter P, De Vos M et al. Risk of development of more-advanced lesions in patients with inflammatory bowel diseases and dysplasia. Clin Gastroenterol Hepatol 2020;18:1528–1536.
Agrawal M, Spencer EA, Colombel JF et al. Approach to the management of recently diagnosed inflammatory bowel disease patients: a user’s guide for adult and pediatric gastroenterologists. Gastroenterology 2021;161:47–65.
Shin CM, Kim N, Han K et al. Anti-diabetic medications and the risk for colorectal cancer: a population-based nested case–control study. Cancer Epidemiol 2020;64:101658.
Bo S, Castiglione A, Ghigo E et al. Mortality outcomes of different sulphonylurea drugs: the results of a 14-year cohort study of type 2 diabetic patients. Eur J Endocrinol 2013;169:117–126.
Hendriks AM, Schrijnders D, Kleefstra N et al. Sulfonylurea derivatives and cancer, friend or foe? Eur J Pharmacol 2019;861:172598.
Qi C, Bin L, Yang Y et al. Glipizide suppresses prostate cancer progression in the TRAMP model by inhibiting angiogenesis. Sci Rep 2016;6:27819.
Mafra CADCC, Vasconcelos RC, de Medeiros CACX, et al. Gliclazide prevents 5-FU-induced oral mucositis by reducing oxidative stress, inflammation, and P-selectin adhesion molecules. Front Physiol 2019;10:327.
Jahan H, Choudhary MI. Gliclazide alters macrophages polarization state in diabetic atherosclerosis in vitro via blocking AGE-RAGE/TLR4-reactive oxygen species-activated NF-κB nexus. Eur J Pharmacol 2021;894:173874.
Lee KY, Kim JR, Choi HC et al. Gliclazide, a K channel blocker, inhibits vascular smooth muscle cell proliferation through the CaMKKβ-AMPK pathway. Vasc Pharmacol 2018;102:21–28.
Liang H, Chen Z, Yang R et al. Methyl gallate suppresses the migration, invasion, and epithelial–mesenchymal transition of hepatocellular carcinoma cells via the AMPK/NF-κB signaling pathway in vitro and in vivo. Front Pharmacol 2022;13:894285.
Yang B, Lu L, Zhou D et al. Regulatory network and interplay of hepatokines, stellakines, myokines and adipokines in nonalcoholic fatty liver diseases and nonalcoholic steatohepatitis. Front Endocrinol (Lausanne) 2022;13:1007944.
Lee JS, Kim HS, Hahm KB et al. Effects of genetic and pharmacologic inhibition of COX-2 on colitis-associated carcinogenesis in mice. J Cancer Prev 2020;25:27–37.
Desfaits AC, Serri O, Renier G. Normalization of plasma lipid peroxides, monocyte adhesion, and tumor necrosis factor-alpha production in NIDDM patients after gliclazide treatment. Diabetes Care 1998;21:487–493.
Sliwinska A, Rogalska A, Szwed M et al. Gliclazide may have an antiapoptotic effect related to its antioxidant properties in human normal and cancer cells. Mol Biol Rep 2012;39:5253–5267.
Yang X, So WY, Ma RC et al. Use of sulphonylurea and cancer in type 2 diabetes-The Hong Kong Diabetes Registry. Diabetes Res Clin Pract 2010;90:343–351.
Cheng Y, Hou K, Wang Y et al. Identification of prognostic signature and gliclazide as candidate drugs in lung adenocarcinoma. Front Oncol 2021;11:665276.
Laudato JA, Tice AL, Johnson BR et al. Impact of prior alcohol use on the subsequent development of cancer cachexia in male and female mice. Alcohol (Hanover) 2023;47:1271–1282.
Ding J, Gou Q, Jia X et al. AMPK phosphorylates PPARδ to mediate its stabilization, inhibit glucose and glutamine uptake and colon tumor growth. J Biol Chem 2021;297:100954.
Kang DH, Jeong DJ, Ahn TS et al. Expression of AMP-activated protein kinase/ten-eleven translocation 2 and their clinical relevance in colorectal cancer. Oncol Lett 2021;21:164.
Liu J, Long S, Wang H et al. Blocking AMPK/ULK1-dependent autophagy promoted apoptosis and suppressed colon cancer growth. Cancer Cell Int 2019;19:336.
Lu Y, Huang R, Ying J et al. RING finger 138 deregulation distorts NF-кB signaling and facilities colitis switch to aggressive malignancy. Signal Transduct Target Ther 2022;7:185.
Eskandani R, Kazempour M, Farahzadi R et al. Engineered nanoparticles as emerging gene/drug delivery systems targeting the nuclear factor-κB protein and related signaling pathways in cancer. Biomed Pharmacother 2022;156:113932.
Chen Y, Li Y, Li C et al. Dexmedetomidine alleviates pain in MPTP-treated mice by activating the AMPK/mTOR/NF-κB pathways in astrocytes. Neurosci Lett 2022;791:136933.
Hou Y, Wei D, Bossila EA et al. FABP5 deficiency impaired macrophage inflammation by regulating AMPK/NF-κB signaling pathway. J Immunol 2022;209:2181–2191.
Tong W, Wang Q, Sun D et al. Curcumin suppresses colon cancer cell invasion via AMPK-induced inhibition of NF-κB, uPA activator and MMP9. Oncol Lett 2016;12:4139–4146.
Funding
This work was supported by the Special Foundation for the Natural Science Foundation of Shandong Province (ZR2019PH081).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors confirm that this article has no conflicts of interest.
Ethical approval
The study was approved by the Experimental Animal Ethics Committee of the Second Hospital of Shandong University.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Li, S., Wang, Y., Zhang, D. et al. Gliclazide Reduces Colitis-Associated Colorectal Cancer Formation by Deceasing Colonic Inflammation and Regulating AMPK-NF-κB Signaling Pathway. Dig Dis Sci 69, 453–462 (2024). https://doi.org/10.1007/s10620-023-08211-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-023-08211-w