Abstract
Background
The accurate evaluation of liver fibrosis is crucial for the treatment and follow up of chronic hepatitis B (CHB) patients.
Aim
We examined the efficiency of serum Mac-2 Binding Protein Glycosylation isomer (M2BPGi) in diagnosing liver fibrosis stages in CHB patients.
Methods
A cross-sectional study was conducted on 177 adult CHB patients visiting the University Medical Center Ho Chi Minh City, Vietnam between October 2019 and December 2021. M2BPGi, ARFI, APRI, and FIB-4 were tested against FibroScan® for sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV). The optimal M2BPGi cut-off values were identified based on the area under the receiver operating characteristic (AUROC) curve.
Results
There was a strong agreement between M2BPGi and FibroScan® (r = 0.77, P < 0.001). The optimal M2BPGi cut-off index (C.O.I) for detecting significant fibrosis (F ≥ 2) was 0.79 with an AUROC of 0.77, 67.3% sensitivity, 70% specificity, 60.6% NPV, and 75.3% PPV. Compared with APRI (61%) and FIB-4 (47%), M2BPGi had the greatest sensitivity for diagnosing F ≥ 2. M2BPGi combined with APRI yielded highest diagnosis performance for F ≥ 2 with an AUROC of 0.87. The optimal cut-off index of M2BPGi for diagnosing cirrhosis (F4) was 1.3 with an AUROC of 0.91, 88% sensitivity, 87.4% specificity, 97% NPV, and 61% PPV. The AUROC of M2BPGi for diagnosing F4 was comparable to that of ARFI (0.93).
Conclusions
With cut-off values of 0.79 C.O.I and 1.3 C.O.I, M2BPGi could be an effective method for diagnosing significant fibrosis and cirrhosis in CHB patients, respectively.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite the availability of effective vaccination, hepatitis B infection (HBV) remains a global public health threat [1]. It is estimated that 316 million people live with chronic hepatitis B (CHB) and 550,000 related deaths worldwide [2]. Treatment of HBV infection including effective management of CHB remains one of the important strategies to achieve the common goal of viral hepatitis elimination by 2030 [1]. It has been well documented that monitoring the severity of liver fibrosis is essential for timely treatment with antiviral therapy and screening of HBV associated complications [3, 4]. Although liver biopsy is considered as the gold standard for assessing fibrosis, it has been rarely utilized in clinical practice because of its invasiveness and related-concerns of sampling error and inter-observer variability [5]. To address this issue, non-invasive tests to assess liver fibrosis have been developed and can be divided into two groups including serum indices and imaging methods [6]. Regarding imaging techniques, transient elastography is the most validated imaging method that can be used as a reference method for liver stiffness assessment in chronic liver diseases [7, 8]. However, significant drawbacks have prevented it from being widely used and include its availability and expense as well as its limited utility in those with severe obesity or ascites [8]. Regarding biomarkers of liver fibrosis, direct markers of extracellular matrix turnover (e.g., Fibrotest®, FibroSpect ll®, and Enhanced Liver Fibrosis score®) and indirect markers (e.g., the aspartate transaminase to platelet ratio index (APRI) and the fibrosis index based on four factors (FIB-4)) have been used [6]. Given that some biomarkers such as APRI are simple, low-cost, and reproducible, they are recommended in the low-resource settings, even though their accuracy is moderate [9]. Recently, Mac-2-binding protein glycosylation isomer (M2BPGi) has been investigated as a potential biomarker for evaluating liver fibrosis in patients with viral hepatitis [10]. Mac-2-binding protein (M2BP) is a secretory glycoprotein which contains seven N-glycans per monomer [11]. In serum, 10–16 monomers of M2BP combine together to form a "doughnut-shaped" polymer that presents 70–112 N-glycans [12]. Although the exact mechanism remains unknown, modifications of M2BP occur in response to the changes in N-glycosylation as liver fibrosis progesses [10]. Wisteria floribunda agglutinin (WFA), a specific lectin that binds the GalNAc residue of N-glycans and O-glycans as well as the clustered LacNAc structure, can accurately capture the altered N-glycans of M2BP [13]. Therefore, this specific glycoprotein has been named as Wisteria floribunda agglutinin-positive Mac-2-binding protein (WFA+-M2BP) or M2BPGi [11]. Several studies have been conducted to appraise the ability to assess liver fibrosis of M2BPGi in various chronic liver diseases, including non-alcoholic fatty liver disease [14], primary biliary cholangitis [15], and autoimmune hepatitis [16]. It has been suggested that the cut-off levels of M2BPGi vary depending on the etiologies of chronic liver disease. [17]
In Vietnam, a recent study has demonstrated that M2BPGi can be a good indicator of early liver disease in patients with different etiologies [18]. However, more in-depth information on the utility of this biomarker in patients with CHB is scare, although Vietnam is a hyper-endemic area of this disease [2]. This study aimed to investigate the role of M2BPGi in diagnosing significant fibrosis and cirrhosis in Vietnamese patients with CHB by comparing its sensitivity (Sens), specificity (Spec), positive predictive value (PPV), and negative predictive value (NPV) with those of the transient elastography as the reference standard. The comparison between M2BPGi and other common markers of liver fibrosis including APRI, FIB-4, and Acoustic Radiation Force Impulse (ARFI) was also performed in this study.
Methods
Study Design and Selection of Study Participants
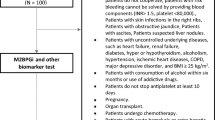
A cross-sectional study was conducted at the Liver Clinic of University Medical Center (UMC) in Ho Chi Minh City in Vietnam between 1st October 2019 and 31st December 2021. The study was approved by the UMC’s Ethics Committee (approval number 36/GCN-HĐĐĐ) and was performed in accordance with the ethical principles of the Declaration of Helsinki. Written informed consent was obtained from all study participants. All patients receiving treatment at this clinic were selected based on pre-defined inclusion and exclusion criteria and invited to participate in the study. Inclusion criteria included patients aged 18 years or older, diagnosed with CHB infection (hepatitis B surface antigen (HBsAg) positive for > 6 months detected by electrochemiluminescence immunoassay), and had not received antiviral treatment. Exclusion criteria included (i) jaundice, ascites, hepatocellular carcinoma (HCC), pregnancy, hepatitis B flare, chronic hepatitis C (CHC) infection, excessive alcohol use (consumption of > 3 drinks/day for men and > 2 drinks/day for women for > 5 years) [19], moderate-to-severe steatohepatitis (Controlled Attenuation Parameter measured by FibroScan® S ≥ S2) [20], (ii) serum alanine aminotransferase (ALT) and aspartate transaminase (AST) levels ≥ 2 × the upper limit of normal [ULN] (based on the local laboratory reference, the ULN of ALT and AST is 40 IU/L for both men and women), and (iii) refusal to participate in the study.
Sample Size and Data Collection
The total sample size was calculated using the formulas for sensitivity and specificity of a diagnostic test [21]. According to a study conducted by Feng et al., the sensitivity of M2BPGi in detecting liver fibrosis stage (F) ≥ 2, and the specificity of M2BPGi in diagnosing F4 were 0.67 and 0.82, respectively. [22] According to another study conducted by Xiao et al., the rates of F ≥ 2 and F4 in CHB patients were 36% and 18%, respectively. [23] Therefore, with the Zα value of 1.96 and a type I error of 0.05, the minimum total sample size was 150.
A questionnaire was used to collect study participants’ information including demography (age, gender, and body mass index (BMI), laboratory tests, and imaging tests. Laboratory tests included biochemistry (M2BPGi, routine blood tests (white blood cell (WBC), hemoglobin (Hb), platelet (PLT) count, aspartate aminotransferase (AST), and alanine aminotransferase (ALT)), and viral tests (HBV surface antigen (HBsAg) and hepatitis C antibody (anti-HCV)). Imaging tests include (FibroScan and ARFI).
FibroScan
FibroScan (Echosens, Paris, France) was used in this study as the gold standard to diagnose liver fibrosis. A FibroScan (FS) session was regarded as successful, and liver stiffness measurements were considered reliable when the obtained shots satisfied the following criteria: (1) at least 10 shots obtained in the FS session were valid; (2) the ratio of the number of valid shots to the total number of shots obtained in the session was greater than 60%; and (3) the interquartile range divided by the median FS value was less than 30% [24]. For each session, the median value of the valid measurements was used as the representative [25]. Fibrosis stages were categorized based on the METAVIR classification [26]. The FS cut-off values used to categorize fibrosis stages included < 7 kPa (F0–1, no-mild liver fibrosis), 7 ≤ 9.5 kPa (F2, moderate liver fibrosis), 9.5 ≤ 11 kPa (F3, severe liver fibrosis), ≥ 11 kPa (F4, liver cirrhosis) [27]. Based on the results of FS measurement, patients were classified into three groups including group 1 (patients with F0 or F1), group 2 (patients with F2 or F3), and group 3 (patients with F4).
Acoustic Radiation Force Impulse (ARFI)
ARFI imaging was performed using ACUSON Juniper Ultrasound System (Siemens Medical Solutions, Erlangen, Germany) with the Virtual Touch Tissue Quantification mode and an abdominal curved transducer. Measurements taken at 2 cm depth from the liver capsule were standardized for measuring shear-wave velocity (SWV). For each ARFI session, measurements obtained from each patient were regarded as reliable when there were at least ten valid measurements, and the ratio of the interquartile range value to the median (IQR/M) < 30% [28]. The median value of all valid measurements was considered the representative ARFI-SWV result.
Laboratory Testing
Blood samples for laboratory testing were taken at the time patients underwent FibroScan and ARFI. Laboratory tests were performed in compliance with the automated procedures of the clinical laboratories. Calculations of APRI and FIB-4 index for liver fibrosis were also performed. [29, 30]
M2BPGi
Serum M2BPGi levels were measured based on a lectin-antibody sandwich immunoassay using a fully automatic HISCL-5000 Immunoanalyzer (Sysmex Corporation, Hyogo, Japan) [10]. Glycosylated M2BP was captured by WFA immobilized on magnetic beads. Subsequently, the bound product was assayed with an antihuman M2BP monoclonal antibody linked to alkaline phosphatase (ALP–αM2BP). The measured values of M2BPGi conjugated to WFA were indexed with the obtained values [31]. The positive control used in this process was as a calibration solution preliminarily standardized to yield a C.O.I value of 1.0. [10]
Statistical Analysis
Data were analyzed by using GraphPad Prism 8.0.2 software. Continuous variables were expressed as median (interquartile range) or mean ± 1 standard deviation (SD) and were compared using Mann–Whitney U test and Kruskal–Wallis test. Categorical variables were presented as an absolute count and percentage and were compared using Fisher's exact test. Pearson’s correlation coefficient was used to examine the association between M2BPGi and other liver fibrosis markers including APRI, FIB-4, ARFI against the reference test—FS. To evaluate the diagnostic performance of M2BPGi and other markers as well as to identify the best cut-off values for predicting significant fibrosis (F ≥ 2) and cirrhosis (F4), the receiver operating characteristic (ROC) curves were developed, and AUROC, sensitivity (Sens), specificity (Spec), PPV, and NPV were calculated. The optimal cut-off values were computed based on the Youden’s index that maximized the sum of sensitivity and specificity [32]. A regression model was developed to examine the association between the use of M2BPGi, APRI and F ≥ 2. The significance level was set at P ≤ 0.05.
Results
Baseline Characteristics of Study Participants
Among 200 hundred cases who were eligible for the study, 13 were excluded due to HBV/HCV co-infection and excessive alcohol use and other 10 were excluded due to moderate-to-severe steatohepatitis. Hence, a total of 177 study participants completed the study (Fig. 1).
The median age was 48 years old and majority of them were male (68.9%). The median M2BPGi level was 0.83 C.O.I (Table 1). Among these 177 patients, the distribution of liver fibrosis stages in the case group included F0–F1 (69/177, 39%), F2–3 (75/177, 42.4%), and F4 (33/177, 18.6%).
Correlation Between M2BPGi Levels and Liver Fibrosis Stages
The median serum M2BPGi levels increased progressively with advanced stages: F0–1 (0.66 C.O.I.), F2–3 (0.865 C.O.I.), and F4 (2.25 C.O.I.) (Fig. 2). There was a statistically significant difference in serum M2BPGi levels between each group with F0–1 and F2–3 (P = 0.041), F2–3 and F4 (P < 0.0001).
Correlation Between Fibroscan and Four Liver Fibrosis Markers Including M2BPGi, ARFI, APRI, and FIB-4
Among four markers, M2BPGi had the highest correlation coefficient (r = 0.77), followed by ARFI (r = 0.71) (Fig. 3). APRI and FIB-4 had moderate correlation (r = 0.57 and r = 0.65, respectively).
Model for the Prediction of Significant Fibrosis (F ≥ 2)
A regression model was developed based on the following formula:
The regression model showed that both M2BPGi (Adjusted odds ratio (AOR) 19.58, 95% CI 5.17–86.34, P < 0.0001) and APRI (AOR 176, 95% CI 12.45–2,791, P < 0.0001) were statistically significant predictors of F ≥ 2 (Table 2).
Diagnostic Accuracy of APRI, FIB-4, ARFI, and M2BPGi Alone or in Combination with APRI for Significant Liver Fibrosis and Cirrhosis
Regarding the diagnosis of F ≥ 2, a combination of M2BPGi and APRI yielded the highest accuracy performance with the AUROC of 0.87, followed by ARFI with an AUROC of 0.85, M2BPGi (0.77), APRI (0.77), and FIB-4 (0.71) (Fig. 4).
Regarding the diagnosis of F4, ARFI yielded the highest AUROC of 0.93, followed by M2BPGi (0.91), APRI (AUROC = 0.91), and FIB-4 (AUROC = 0.88) (Fig. 5).
From the ROC curve of using M2BPGi to predict F ≥ 2, the optimal cut-off of M2BPGi value was calculated as 0.79 C.O.I with a Sens of 67.3%, Spec of 70%, PPV of 75.3%, and NPV of 60.6% (Table 3). The optimal cut-off of APRI was 0.5 with a Sens of 61%, Spec of 90%, PPV of 89.2%, and NPV of 62.5%. The use of a combination of M2BPGi and APRI to predict F ≥ 2 demonstrated a sens of 72.1%, spec of 89.9%, PPV of 85.1%, and NPV of 69.6%. The optimal cut-off of FIB-4 to diagnose F ≥ 2 was 1.8 with a Sens of 46.8%, Spec of 87%, PPV of 83.2%, and NPV of 54.1%. The optimal cut-off of ARFI for identify F ≥ 2 was calculated as 1.4 m/s with a Sens of 89.8%, Spec of 65.2%, PPV of 78.1%, and NPV of 82.3%.
From the ROC curve of using M2BPGi to predict F4, the optimal cut-off of M2BPGi value was calculated as 1.3 C.O.I with a Sens of 88%, Spec of 87.4%, PPV of 61%, and NPV of 97% (Table 3). The optimal cut-off APRI was 0.7 with a Sens of 75%, Spec of 88%, PPV of 58%, and NPV of 94.1%. The optimal cut-off FIB-4 was 1.8 with a Sens of 46.8%, Spec of 87%, PPV of 83.2%, and NPV of 54.1%. The optimal cut-off of ARFI was calculated as 1.6 m/s with a Sens of 94%, Spec of 81.2%, PPV of 52%, and NPV of 98%.
Discussion
Liver fibrosis evaluation, especially detecting early fibrosis stages such as significant fibrosis, is paramount in managing patients with CHB [3, 4]. It has been suggested that an ideal non-invasive fibrosis marker should be accurate, reproducible, accessible, safe, and non-operator dependent [8]. All currently used non-invasive markers such as FibroTest®, APRI, FIB-4 have their own limitations including combined indices containing many variables which are prone to confounding [24]. In addition, elastography methods like FibroScan and ARFI may be incorrect in patients whose ALT levels are higher than five times the upper limit of normal [24]. Recently, there is evidence that M2BPGi appears to overcome these barriers because it requires only a single molecule measurement to estimate liver fibrosis and therefore, reducing the possibility of false positive or false negative results [31]. Furthermore, M2BPGi is measured using a fully automated HSCL-2000i Immunoanalyzer, which produces results in only 17 min, demonstrating its considerably rapid turnaround time [10, 33]. M2BPGi has been shown to be a reliable marker in fibrosis staging in liver diseases with different etiologies such as nonalcoholic fatty liver disease and CHC [33,34,35]. Studies have also been conducted worldwide to examine the role of this biomarker in CHB. A study in West Africa found a significant association between M2BPGi and both CHB associated cirrhosis and hepatocellular carcinoma [36]. In Asia, studies in Hong Kong found that M2BPGi is a reliable marker for diagnosing F ≥ 2, F ≥ 3 and F4 in CHB patients treated with nucleos(t)ide analogues (NAs) [31], as well as there is an association between high levels of M2BPGi and increased risk of persistent advanced fibrosis [37]. Another study in Taiwan documented that M2BPGi is a strong and independent short-term predictor of HCC in CHB patients [38]. The findings of our study further demonstrated that M2BPGi is a useful biomarker for liver fibrosis assessment in Vietnamese patients with CHB.
Our study found a statistically significant difference in the M2BPGi levels between different stages of CHB-associated liver fibrosis including F0–1 vs F2–3 vs F4 group. Our finding is supported by previous studies about M2BPGi in patients with CHB and other etiologies, such as CHC, auto-immune hepatitis, and non-alcoholic fatty liver disease [14, 16, 39,40,41]. It should be noted that from the clinical point of view, distinguishing between F0 and F1 as well as between F2 and F3 is not necessary, provided that there is no difference in management [3, 4]. It is interesting to note that the median M2BPGi levels in F4 group were significantly higher than those of other groups which may indicate that this biomarker has a great potential in diagnosing cirrhosis. Given the high cost and non-availability in small healthcare settings of FibroScan [42], the World Health Organization recommends that APRI should be a preferred non-invasive tool to detect significant fibrosis in developing countries [9]. However, a study conducted by Zou et al. found that the WFA+ -M2BP levels show a better correlation with FibroScan (r = 0.77) than APRI (0.57) [40]. Concurring with this study, we found a strong correlation between M2BPGi and FibroScan. This suggests that M2BPGi can be a reliable alternative for Fibroscan in developing countries. In light of this, we strongly believe that M2BPGi is a reliable marker that can be used to assist in staging liver fibrosis, especially in low-resource settings.
Regarding the ability to detect significant fibrosis, our study found that M2BPGi had a moderate level of accuracy with an AUROC of 0.77 which was similar to that of APRI and FIB-4 (AUROC 0.77 and 0.71, respectively), while ARFI had the highest level of accuracy with an AUROC of 0.85. These findings concur with results of a recent meta-analysis that included nine studies conducted on 1,499 patients with significant fibrosis due to HBV [22]. This meta-analysis has found a comparable pooled AUROC of M2BPGi which is 0.72 (95% confident interval (CI) 0.68–0.76) [22]. Although the cut-off level found in this study is slightly lower than our result (0.97 vs 0.79), the sensitivity and specificity are nearly identical (0.67 and 0.68 vs 0.67 and 0.7) [22]. It should be noted that, in contrast to our study, almost all studies included in the meta-analysis used liver biopsy as a reference, which may have influenced the findings. Since the performance of M2BPGi in detecting significant fibrosis is not better than that of APRI or FIB-4, it has been suggested that studies should be conducted to examine the performance of M2BPGi in combination with other fibrosis markers, such as ARFI, APRI or FIB-4, in order to improve diagnostic accuracy for significant fibrosis. [31] Indeed, given that timely diagnosis of significant fibrosis remains a challenge, necessitating the concurrent use of two or more markers rather than using a single marker has been suggested to increase accuracy [43]. It has been reported that a combination of M2BPGi and FibroScan helps increase both specificity and sensitivity of these markers in diagnosing significant fibrosis [40]. Our study has further found that M2BPGi combined with APRI also yields an optimal AUROC which is comparable to that of ARFI (0.87 vs 0.85).
In our study, M2BPGi had a considerably high AUROC value in identifying cirrhosis which is comparable to that of ARFI (0.93 vs 0.91). Our result is considerably distinct from a meta-analysis of M2BPGi as a diagnostic marker of liver fibrosis by Feng et al. (pooled AUROC: 0.81, 95% CI 0.77–0.86) [22]. Similarly, Wei et al. also reported a lower AUROC value of 0.811 (95% CI 0.735–0.860) regarding the use of M2BPGi as a potential diagnostic tool of cirrhosis in Chinese patients with CHB [44]. Despite using Fibroscan as a standard, the proportion of people with liver fibrosis in Wei's study considerably differs from ours, which could partially explain the discrepancy between the AUROC values documented in the two studies. Simultaneously, compared with the study conducted by Feng et al., we found comparable optimal cut-off points of M2BPGi values (1.3 vs 1.43 C.O.I) together with their specific values (88% vs 82%) [22]. We also found a high NPV of 97% with our cut-off points of M2BPGi values. In view of our results, cirrhosis can be ruled out when serum M2BPGi values are less than 1.3 C.O.I.
This study has some clear limitations. Firstly, FibroScan was used as the reference method in our study instead of liver biopsy to evaluate the degree of liver fibrosis. The different diagnosis performance between FibroScan and liver biopsy may influence our results [45]. Secondly, our case group included CHB patients with normal or nearly normal ALT levels which may limit the generalizability of the study findings. Nevertheless, the strict inclusion criteria for cases with CHB and the selection of controls without any common hepatitis diseases (CHB, CHC, alcohol liver diseases, and non-alcohol fatty liver disease) would help the quantification of an association between M2BPGi values and fibrosis stages in our study reliable and specific to patients with CHB in Vietnam and comparable settings.
In conclusion, given the high level of agreement between M2BPGi and FibroScan, M2BPGi could be a reliable alternative to assess liver fibrosis in patients with CHB, especially in low-resource settings. The M2BPGi cut-off values of 0.79 C.O.I and 1.3 C.O.I are suggested to diagnose significant fibrosis and liver cirrhosis, respectively. M2BPGi combined with APRI can improve the accuracy in detecting significant fibrosis. Future studies are needed to evaluate the role of M2BPGi in monitoring fibrosis in patients with different ALT levels as well as response to antiviral treatment and HCC progression among patients with CHB.
Abbreviations
- ALT:
-
Alanin aminotransferase
- ALP:
-
Alkaline phosphatase
- AOR:
-
Adjusted odds ratio
- APRI:
-
The aspartate transaminase to platelet ratio index
- ARFI:
-
Acoustic radiation force impulse
- AST:
-
Aspartate aminotranferase
- AUROC:
-
The area under the receiver operating characteristic
- BMI:
-
Body mass index
- CHB:
-
Chronic hepatitis B
- CHC:
-
Chronic hepatitis C
- C.O.I:
-
Cut off index
- CI:
-
Confident interval
- FIB-4:
-
The fibrosis index based on four factors
- FS:
-
Fibroscan
- Hb:
-
Hemoglobin
- HbsAg:
-
Hepatitis B surface antigen
- HBV:
-
Hepatitis B virus
- HCC:
-
Hepatocellular carcinoma
- HCV:
-
Hepatitis C virus
- M2BP:
-
Mac-2-binding protein
- M2BPGi:
-
Mac-2-binding protein glycosylation isomer
- NAs:
-
Nucleos(t)ide analogues
- NPV:
-
Negative predictive value
- PLT:
-
Platelet
- PPV:
-
Positive predictive value
- Sens:
-
Sensitivity
- Spec:
-
Specificity
- SWV:
-
Shear-wave velocity
- UMC:
-
University Medical Center
- WBC:
-
White blood cell
- WFA:
-
Wisteria floribunda agglutinin
- WFA+-M2BP:
-
Wisteria floribunda agglutinin-positive Mac-2-binding protein
References
Zhu M, Wang H, Lou T et al. Current treatment of chronic hepatitis B: Clinical aspects and future directions. Frontiers in microbiology. 2022;13:975584.
GBD Hepatitis B Collaborators. Global, regional, and national burden of hepatitis B, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Gastroenterol Hepatol. 2022;7:796–829.
Terrault NA, Lok A, McMahon BJ et al. Update on prevention, diagnosis, and treatment of chronic hepatitis B: AASLD 2018 hepatitis B guidance. Hepatology. 2018;67:1560–1599.
EASL. EASL. Clinical Practice Guidelines on the management of hepatitis B virus infection. J Hepatol. 2017;2017:370–398.
Regev A, Berho M, Jeffers LJ et al. Sampling error and intraobserver variation in liver biopsy in patients with chronic HCV infection. Am J Gastroenterol. 2002;97:2614–2618.
EASL-ALEH Clinical Practice Guidelines. Non-invasive tests for evaluation of liver disease severity and prognosis. J Hepatol. 2015;63:237–264.
Tapper EB, Castera L, Afdhal NH. FibroScan (vibration-controlled transient elastography): where does it stand in the United States practice. Clin Gastroenterol Hepatol. 2015;13:27–36.
EASL. Clinical Practice Guidelines on non-invasive tests for evaluation of liver disease severity and prognosis-2021 update. J Hepatol. 2021;2021:659–689.
Guidelines for the Prevention. Care and Treatment of Persons with Chronic Hepatitis B Infection. Geneva: World Health Organization; 2015.
Kuno A, Ikehara Y, Tanaka Y et al. A serum “sweet-doughnut” protein facilitates fibrosis evaluation and therapy assessment in patients with viral hepatitis. Sci Rep. 2013;3:1065.
Narimatsu H. Development of M2BPGi: a novel fibrosis serum glyco-biomarker for chronic hepatitis/cirrhosis diagnostics. Expert Review of Proteomics. 2015;12:683–693.
Sumida Y, Yoneda M, Seko Y et al. Surveillance of Hepatocellular Carcinoma in Nonalcoholic Fatty Liver Disease. Diagnostics (Basel, Switzerland). 2020;10:579.
Yamasaki K, Tateyama M, Abiru S et al. Elevated serum levels of Wisteria floribunda agglutinin-positive human Mac-2 binding protein predict the development of hepatocellular carcinoma in hepatitis C patients. Hepatology. 2014;60:1563–1570.
Abe M, Miyake T, Kuno A et al. Association between Wisteria floribunda agglutinin-positive Mac-2 binding protein and the fibrosis stage of non-alcoholic fatty liver disease. J Gastroenterol. 2015;50:776–784.
Umemura T, Joshita S, Sekiguchi T et al. Serum Wisteria floribunda Agglutinin-Positive Mac-2-Binding Protein Level Predicts Liver Fibrosis and Prognosis in Primary Biliary Cirrhosis. Am J Gastroenterol. 2015;110:857–864.
Nishikawa H, Enomoto H, Iwata Y et al. Clinical significance of serum Wisteria floribunda agglutinin positive Mac-2-binding protein level and high-sensitivity C-reactive protein concentration in autoimmune hepatitis. Hepatol Res. 2016;46:613–621.
Ito K, Murotani K, Nakade Y et al. Serum Wisteria floribunda agglutinin-positive Mac-2-binding protein levels and liver fibrosis: A meta-analysis. Journal of Gastroenterology and Hepatology 2017;32:1922–1930.
Pham TTT, Ho D, Nguyen T. Usefulness of Mac-2 binding protein glycosylation isomer in non-invasive probing liver disease in the Vietnamese population. World J Hepatol. 2020;12:220–229.
Singal AK, Bataller R, Ahn J et al. ACG Clinical Guideline: Alcoholic Liver Disease. Am J Gastroenterol. 2018;113:175–194.
Sansom SE, Martin J, Adeyeami O et al. Steatosis rates by liver biopsy and transient elastography with controlled attenuation parameter in clinical experience of Hepatitis C Virus (HCV) and Human Immunodeficiency Virus/HCV Coinfection in a Large US Hepatitis Clinic. Open Forum Infect Dis. 2019;6:099.
Buderer NM. Statistical methodology: I. Incorporating the prevalence of disease into the sample size calculation for sensitivity and specificity. Acad Emerg Med. 1996;3:895–900.
Feng S, Wang Z, Zhao Y, Tao C. Wisteria floribunda agglutinin-positive Mac-2-binding protein as a diagnostic biomarker in liver cirrhosis: an updated meta-analysis. Sci Rep. 2020;10:10582.
Xiao G, Yang J, Yan L. Comparison of diagnostic accuracy of aspartate aminotransferase to platelet ratio index and fibrosis-4 index for detecting liver fibrosis in adult patients with chronic hepatitis B virus infection: a systemic review and meta-analysis. Hepatology. 2015;61:292–302.
European Association for Study of Liver Asociacion Latinoamericana para el Estudio del Higado. EASL-ALEH Clinical Practice Guidelines: Non-invasive tests for evaluation of liver disease severity and prognosis. J Hepatol. 2015;63:237–264.
Li C, Li R, Zhang W. Progress in non-invasive detection of liver fibrosis. Cancer Biol Med. 2018;15:124–136.
Bedossa P, Poynard T. An algorithm for the grading of activity in chronic hepatitis C. The METAVIR Cooperative Study Group. Hepatology. 1996;24:289–293.
The Ministry of Health of Vietnam. Guidelines for diagnosis and management of hepatitis B. 2019.
Frulio N, Trillaud H, Perez P et al. Acoustic Radiation Force Impulse (ARFI) and Transient Elastography (TE) for evaluation of liver fibrosis in HIV-HCV co-infected patients. BMC Infect Dis. 2014;14:405.
Wai CT, Greenson J, Fontana RJ et al. A simple noninvasive index can predict both significant fibrosis and cirrhosis in patients with chronic hepatitis C. Hepatology. 2003;38:518–526.
Vallet-Pichard A, Mallet V, Nalpas B et al. FIB-4: an inexpensive and accurate marker of fibrosis in HCV infection. comparison with liver biopsy and fibrotest. Hepatology. 2007;46:32–36.
Mak LY, Wong DK, Cheung KS, Seto WK, Lai CL, Yuen MF. Role of serum M2BPGi levels on diagnosing significant liver fibrosis and cirrhosis in treated patients with chronic hepatitis B virus infection. Clinical and Translational Gastroenterology. 2018;9:163.
Youden WJ. Index for rating diagnostic tests. Cancer. 1950;3:32–35.
Tangvoraphonkchai K, Suttichaimongkol T, Kularbkaew C, Sangaimwibool P, Sukeepaisarnjaroen W. Application of Mac-2 binding protein glycosylation isomer as a non-invasive biomarker for probing liver disease. Scientific Reports. 2022;12:6757.
Cheng Y-M, Wang C-C. Comparison of Mac-2 binding protein glycosylation isomer (M2BPGi) with AST to platelet ratio index (APRI), fibrosis 4 Score (FIB-4), and nonalcoholic fatty liver disease (NAFLD) fibrosis score (NFS) for NAFLD patients.n/a(n/a).
Saleh SA, Salama MM, Alhusseini MM, Mohamed GA. M2BPGi for assessing liver fibrosis in patients with hepatitis C treated with direct-acting antivirals. World journal of gastroenterology. 2020;26:2864–2876.
Vincent JP, Ndow G, Ogawa S et al. Mac-2 binding protein glycosylation isomer (M2BPGi) to evaluate liver fibrosis and cancer in HBV-infected patients in West Africa. Journal of global health. 2022;12:04076.
Mak LY, Wong DK, Cheung KS et al. Role of Serum M2BPGi Levels in Predicting Persistence of Advanced Fibrosis in Chronic Hepatitis B Virus Infection. Digestive diseases and sciences. 2022;67:5127–5136.
Liu J, Hu H-H, Lee M-H et al. Serum Levels of M2BPGi as Short-Term Predictors of Hepatocellular Carcinoma in Untreated Chronic Hepatitis B Patients. Scientific Reports. 2017;7:14352.
Xu H, Kong W, Liu L et al. Accuracy of M2BPGi, compared with Fibro Scan(R), in analysis of liver fibrosis in patients with hepatitis C. BMC Gastroenterol. 2017;17:62.
Zou X, Zhou M, Yu DM et al. Serum WFA(+) -M2BP levels for evaluation of early stages of liver fibrosis in patients with chronic hepatitis B virus infection. Liver Int. 2017;37:35–44.
Ishii A, Nishikawa H, Enomoto H et al. Clinical implications of serum Wisteria floribunda agglutinin-positive Mac-2-binding protein in treatment-naive chronic hepatitis B. Hepatol Res. 2017;47:204–215.
Castéra L, Vergniol J, Foucher J et al. Prospective comparison of transient elastography, Fibrotest, APRI, and liver biopsy for the assessment of fibrosis in chronic hepatitis C. Gastroenterology. 2005;128:343–350.
Papastergiou V, Tsochatzis E, Burroughs AK. Non-invasive assessment of liver fibrosis. Ann Gastroenterol. 2012;25:218–231.
Wei B, Feng S, Chen E et al. M2BPGi as a potential diagnostic tool of cirrhosis in Chinese patients with Hepatitis B virus infection. J Clin Lab Anal. 2018;32:e22261.
Li Y, Huang YS, Wang ZZ et al. Systematic review with meta-analysis: the diagnostic accuracy of transient elastography for the staging of liver fibrosis in patients with chronic hepatitis B. Alimentary pharmacology & therapeutics. 2016;43:458–469.
Acknowledgments
We are grateful to Sysmex Asia Pacific Pte Ltd. and Sysmex Vietnam for providing the HISCL M2BPGi reagent kits and the automatic immunoanalyzer HISCL-5000.
Funding
N/A.
Author information
Authors and Affiliations
Contributions
The trial was designed by Hoang Huu Bui, together with Sang The Phan, Suong Thi-Bang Nguyen, Chuong Dinh Nguyen. Chuong Dinh Nguyen, Khue Minh Nguyen interpreted data for work. All authors wrote and revised the manuscript critically for important intellectual content. All authors meet the authorship criteria and approve the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Authors declare no conflict of interests for this article.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent to publish
Patients signed informed consent regarding publishing their data and photographs.
Clinical trial registration
N/A.
Ethical approval
The study was conducted in accordance with the Declaration of Helsinki and approved by University Medical Center Ho Chi Minh City (approval no.36/GCN-HĐĐĐ).
Permission to reproduce material from other sources
N/A.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Bui, H.H., Nguyen, S.TB., Phan, S.T. et al. Evaluating M2BPGi as a Marker for Liver Fibrosis in Patients with Chronic Hepatitis B. Dig Dis Sci 68, 4407–4417 (2023). https://doi.org/10.1007/s10620-023-08143-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-023-08143-5