Abstract
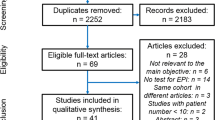
The prevalence of celiac disease (CD) is approximately 1% in the US. Studies have shown possible association between exocrine pancreatic insufficiency (EPI) and CD, with numerous hypothesized biological mechanisms including small bowel mucosal damage causing disruption of enteric-mediated hormonal secretion such as cholecystokinin and loss of enterokinase. The overall prevalence of EPI in CD remains unknown. We performed systematic review and metanalysis and examined the prevalence of EPI in patients who were first diagnosed with CD versus those who had been on treatment with gluten-free diet (GFD). Results Six studies were included in the analysis totaling 446 CD patients (Avg age 44.1 years; 34% Males). One hundred and forty-four patients had newly diagnosed CD, and 302 patients had known CD with at least 9 months treatment with GFD. Four studies examined newly diagnosed CD patients. The individual rates of EPI in new CD patients ranged from 10.5 to 46.5%. The pooled prevalence of EPI in newly diagnosed CD patients was 26.2% (95% CI 8.43–43.92%, Q = 2.24, I2 = 0%). Five studies examined CD patients on GFD. The rate of EPI ranged from 1.9% to 18.2%. The prevalence of EPI in patients treated with GFD is 8% (95% CI 1.52–14.8%, Q = 4.42, I2 = 9.59%). Patients with newly diagnosed CD are significantly more likely to have EPI compared to those patients treated with GFD (p = 0.031). CD patients on GFD with persistent symptoms have a significantly higher rate of EPI (28.4%) compared to CD patients on GFD who are asymptomatic (3%) (p < 0.001).




Similar content being viewed by others
References
Barker JM, Liu E. Celiac disease: pathophysiology, clinical manifestations, and associated autoimmune conditions. Adv Pediatr. 2008;55:349–365.
Gujral N, Freeman HJ, Thomson AB. Celiac disease: prevalence, diagnosis, pathogenesis and treatment. World J Gastroenterol. 2012;18:6036–6059.
King JA, Joeng J, Underwood FE et al. Incidence of Celiac Disease Is Increasing Over Time: A Systematic Review and Meta-analysis. American Journal of Gastroenterology. 2020;115:507–525.
Rubio-Tapia A, Hill ID, Kelly CP, Calderwood AH, Murray JA. American College of Gastroenterology clinical guideline: diagnosis and management of celiac disease. The American journal of gastroenterology. 2013;108:656–676.
Al-Toma A, Volta U, Auricchio R, Castillejo G et al. European Society for the Study of Coeliac Disease (ESsCD) guideline for coeliac disease and other gluten-related disorders. United European Gastroenterol J. 2019;7:583–613.
Leffler DA, Dennis M, Hyett B, Kelly E, Schuppan D, Kelly CP. Etiologies and predictors of diagnosis in nonresponsive celiac disease. Clin Gastroenterol Hepatol. 2007;5:445–450.
Penny HA, Baggus EMR, Rej A, Snowden JA, Sanders DS. Non-Responsive Coeliac Disease: A Comprehensive Review from the NHS England National Centre for Refractory Coeliac Disease. Nutrients. 2020;12:216.
Sadr-Azodi O, Sanders DS, Murray JA, Ludvigsson JF. Patients with celiac disease have an increased risk for pancreatitis. Clin Gastroenterol Hepatol. 2012;10:1136–1142.
Regan PT, DiMagno EP. Exocrine pancreatic insufficiency in celiac sprue: a cause of treatment failure. Gastroenterology. 1980;78:484–487.
Vujasinovic M, Tepes B, Volfand J, Rudolf S. Exocrine pancreatic insufficiency, MRI of the pancreas and serum nutritional markers in patients with coeliac disease. Postgrad Med J. 2015;91:497–500.
Leeds JS, Hopper AD, Hurlstone DP et al. Is exocrine pancreatic insufficiency in adult coeliac disease a cause of persisting symptoms? Aliment Pharmacol Ther. 2007;25:265–271.
Evans KE, Leeds JS, Morley S, Sanders DS. Pancreatic insufficiency in adult celiac disease: do patients require long-term enzyme supplementation? Dig Dis Sci. 2010;55:2999–3004.
Landgren AM, Landgren O, Gridley G, Dores GM, Linet MS, Morton LM. Autoimmune disease and subsequent risk of developing alimentary tract cancers among 45 million US male veterans. Cancer. 2011;117:1163–1171.
Rana S, Dambalkar A, Chhabra P et al. Is pancreatic exocrine insufficiency in celiac disease related to structural alterations in pancreatic parenchyma? Ann of Gastroenterol. 2016;29:363–366.
Efthymakis K, Serio M, Barone E et al. P.12.5 Exocrine pancreatic insufficiency in adult Celiac Disease is associated with symptom severity and readily responds to gluten exclusion. Digestive and Liver Disease. 2016;48:e186.
Ockenga J. Importance of nutritional management in diseases with exocrine pancreatic insufficiency. HPB. 2009;1:11–15.
Novis BH, Bank S, Marks IN. Exocrine pancreatic function in intestinal malabsorption and small bowel disease. Am J Dig Dis. 1972;17:489–494.
Carroccio A, Iacono G, Montalto G et al. Pancreatic insufficiency in celiac disease is not dependent on nutritional status. Dig Dis Sci. 1994;39:2235–2242.
Nousia-Arvanitakis S, Fotoulaki M, Tendzidou K, Vassilaki C, Agguridaki C, Karamouzis M. Subclinical exocrine pancreatic dysfunction resulting from decreased cholecystokinin secretion in the presence of intestinal villous atrophy. J Pediatr Gastroenterol Nutr. 2006;43:307–312.
Lentze MJ, Green JR, Sterchi EE, Nusslé D, Hermier M. Intestinal enteropeptidase deficiency associated with exocrine pancreatic insufficiency. Lancet. 1982;2:504.
Patel RS, Johlin FC Jr, Murray JA. Celiac disease and recurrent pancreatitis. Gastrointest Endosc. 1999;50:823–827.
Carroccio A, Di Prima L, Scalici C et al. Unexplained elevated serum pancreatic enzymes: a reason to suspect celiac disease. Clin Gastroenterol Hepatol. 2006;4:455–459.
Munn Z, Moola S, Lisy K, Riitano D, Tufanaru C. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and incidence data. Int J Evid Based Healthc. 2015;13:147–153.
Neyeloff JL, Fuchs SC, Moreira LB. Meta-analyses and Forest plots using a microsoft excel spreadsheet: step-by-step guide focusing on descriptive data analysis. BMC Res Notes. 2012;5:52.
Fine KD, Meyer RL, Lee EL. The prevalence and causes of chronic diarrhea in patients with celiac sprue treated with a gluten-free diet. Gastroenterology. 1997;112:1830–1838.
Collins BJ, Bell PM, Boyd S, Kerr J, Buchanan KD, Love AH. Endocrine and exocrine pancreatic function in treated coeliac disease. Pancreas. 1986;1:143–147.
Singh VK, Haupt ME, Geller DE, Hall JA, Quintana Diez PM. Less common etiologies of exocrine pancreatic insufficiency. World J Gastroenterol. 2017;23:7059–7076.
Lee SK, Lo W, Memeo L, Rotterdam H, Green PH. Duodenal histology in patients with celiac disease after treatment with a gluten-free diet. Gastrointest Endosc. 2003;57:187–191.
Rubio-Tapia A, Rahim MW, See JA, Lahr BD, Wu TT, Murray JA. Mucosal recovery and mortality in adults with celiac disease after treatment with a gluten-free diet. Am J Gastroenterol. 2010;105:1412–1420.
Wahab PJ, Meijer JW, Mulder CJ. Histologic follow-up of people with celiac disease on a gluten-free diet: slow and incomplete recovery. Am J Clin Pathol. 2002;118:459–463.
Domínguez-Muñoz JE, Iglesias-García J. Oral pancreatic enzyme substitution therapy in chronic pancreatitis: is clinical response an appropriate marker for evaluation of therapeutic efficacy? JOP. 2010;11:158–162.
Carroccio A, Iacono G, Montalto G et al. Pancreatic enzyme therapy in childhood celiac disease. Dig Dis Sci. 1995;40:2555–2560.
Naing L, Winn T, Rusli BN. Practical issues in calculating the sample size for prevalence studies. Archives of orofacial Sciences. 2006;1:9–14.
Vanga RR, Tansel A, Sidiq S, El-Serag HB, Othman MO. Diagnostic Performance of Measurement of Fecal Elastase-1 in Detection of Exocrine Pancreatic Insufficiency: Systematic Review and Meta-analysis. Clin Gastroenterol Hepatol. 2018;16:1220–1228.
Lankisch PG, Schmidt I, König H et al. Faecal elastase 1: not helpful in diagnosing chronic pancreatitis associated with mild to moderate exocrine pancreatic insufficiency. Gut. 1998;42:551–554.
Acknowledgments
We thank Pranusha Atuluru for her contribution to the editing of citations to DDS guidelines.
Author information
Authors and Affiliations
Contributions
CJ contributed to study concept and design, acquisition of data, analysis and interpretation of the data, drafting of the manuscript, and statistical analysis. JAB contributed to drafting of the manuscript and critical revision of the manuscript for important intellectual content. JB contributed to study concept and design, acquisition of the data, drafting of the manuscript, and critical revision of the manuscript for important intellectual content.
Corresponding author
Ethics declarations
Conflict of interest
The authors do not have any competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jiang, C., Barkin, J.A. & Barkin, J.S. Exocrine Pancreatic Insufficiency Is Common in Celiac Disease: A Systematic Review and Meta-Analysis. Dig Dis Sci 68, 3421–3427 (2023). https://doi.org/10.1007/s10620-023-07965-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-023-07965-7