Abstract
Background and Aims
Upper GI bleeding (UGIB) is a common indication for inpatient esophagogastroduodenoscopy (EGD). Guideline adherence improves post-EGD care, including appropriate medication dosing/duration and follow-up procedures that reduce UGIB-related morbidity. We aimed to optimize and standardize post-EGD documentation to improve process and clinical outcomes in UGIB-related care.
Methods
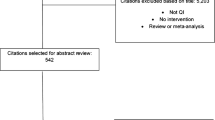
We performed a prospective quality improvement study of inpatient UGIB endoscopies at an academic tertiary referral center during 6/2019–7/2021. Guidelines were used to develop etiology/severity-specific electronic health record note templates. Participants (39 faculty/15 trainees) completed 10-min training in template content/use. We collected pre/post-intervention process data on “Minimal Standard Report” (MSR) documentation including patient disposition, diet, and medications. We also recorded documentation of re-bleed precautions and follow-up procedures. Study outcomes included guideline-based medication prescriptions, ordering of follow-up EGD, and post-discharge re-bleeding. Pre/post-intervention analysis was performed using chi-square tests.
Results
From a pre-intervention baseline of 199 patients to 459 patients post-intervention, compliance improved with inpatient PPI (53.4–77.9%, p < 0.001) and discharge PPI (31.3–61.0%, p < 0.001) prescriptions. There was improvement in MSR completion (28.6–42.5%, p < 0.001). Compliance improved with octreotide prescriptions (75.0–93.6%, p = 0.002) and follow-up EGD order (61.3–87.1%, p < 0.001). There was no change in post-discharge re-bleeding. 82.6% of cases used templates.
Conclusions
Our project leveraged endoscopy software to standardize documentation, resulting in improved clinical care behavior and efficiency. Our intervention required low burden of maintenance, and sustainability with high utilization over 9 months. Similar endoscopy templates can be applied to other health systems and procedures to improve care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Upper GI bleeding (UGIB), is one of the most common indications for hospitalization in the United States [1], costing $5000–$19,000 per admission and $2.5 billion annually [2]. A critical component of inpatient UGIB management is upper endoscopy (EGD). This procedure allows for diagnosis of bleeding source and interventions to stop bleeding/prevent re-bleeding. EGD findings dictate important post-procedure care, including (1) Timing/type of diet [3], (2) Medications to treat/prevent re-bleeding (proton pump inhibitors (PPIs) or octreotide) [3, 4] or minimize complications (antibiotics in cirrhosis) [4], (3) Acuity of inpatient care, and (4) Follow-up EGD as an inpatient (i.e., prevent re-bleeding) [5] or outpatient (i.e., rule out neoplasia and surveillance). The endoscopist is responsible for communicating these important, standard-of-care follow-up recommendations to the consulting service and patient. This communication often occurs through the documented endoscopy report, consultation notes, and verbal communication.
Adherence to guideline-based care in inpatient UGIB can decrease length of stay, reduce costs/patient harms, and improve outcomes [6, 7]. The potential harms associated with antibiotic [8] and PPI overuse [9] are well documented. Overutilization of follow-up endoscopies contributes to cost [10] and underuse raises the risk of re-bleeding and missed high-risk varices [11] or neoplasia [12, 13]. Unfortunately, post-EGD standard-of-care is not uniformly followed, resulting in medical errors of omission and commission. For example, low-risk peptic ulcer disease and esophagitis carry low risk of re-bleeding, thus warrant oral PPI and early discharge [14], but intravenous (IV) PPI overuse is common [15, 16]. Follow-up EGDs are often both over and under recommended [17].
A possible contributor to non-adherence to post-EGD standard-of-care may be inconsistent communication of recommendations. Deficiencies in endoscopist documentation have been observed in several diseases including inflammatory bowel disease, varices, and Barrett’s esophagus [18,19,20]. Professional GI societies have defined “Minimal Standard Terminology” for endoscopic classification of pathology [21], but there are currently few requirements regarding what elements should be in a Minimal Standard Report (MSR) including recommendations and follow-up [22]. Outside of the non-closed loop communications of the endoscopy report/consultation note, the inpatient GI service often provides verbal and/or electronic health record (EHR)-mediated recommendations to consulting services. However, in the era of shift-work [23], these messages and results can be missed during handoffs due to both incomplete documentation and information overload in the EHR [24, 25]. Given that communication failure is one of the leading causes for medication errors and other safety events [26], timely, precise, and comprehensive endoscopic documentation of post-procedure recommendations (diet, medications, acuity of care, follow-up) from endoscopist to consulting teams (primary providers and nursing staff) can serve a critical role in guideline-adherent post-EGD care.
Our quality improvement (QI) study leveraged the EHR as a platform for intervention to address gaps between post-endoscopic communication and clinical care after UGIB. The aim of our study was to streamline and standardize post-EGD documentation of recommendations to improve guideline-adherent care for inpatient UGIB patients.
Methods
Setting and Target Patient Population
This QI project was conducted at a high-volume (703 beds) tertiary academic referral medical center (including liver transplantation) where inpatients with UGIB are cared for by teaching and non-teaching services in the inpatient ward and step-down/intensive care units [27]. All inpatient endoscopic procedures are performed by a teaching gastroenterology consultation or hepatology service. We included patients aged 18 and over who underwent inpatient EGD (including antegrade small bowel enteroscopy) for gastrointestinal bleeding or anemia between June-2019 through July-2021. There were no exclusion criteria. The study was exempt as “Not-Human Subject Research” after review by the Colorado Multiple Institutions Review Board.
Intervention Framework and Development
We used the Standards for Quality Improvement Reporting Excellence (SQUIRE) framework to describe our QI study [28], which standardizes assessment of the domains that impact the viability of a QI project: the project team, existing microsystem, local QI support/capacity, presiding clinical organization, and external environment. We met with our multidisciplinary stakeholder team (gastroenterology and medicine faculty, trainees, and nurses) twice between November-2019 and January-2020 to identify potential targets for intervention. We used a fishbone diagram to organize contributors to our problem such as medical knowledge (i.e., UGIB guidelines), diagnostic reasoning (i.e., re-bleeding mitigation), therapeutic choices (i.e., inconsistent medication prescriptions), materials/machines (i.e., lack of real-time endoscopic documentation and multiple EHR systems), personnel/people (i.e., shift handoffs), and communication (i.e., fragmented multidisciplinary teams) (See Supplementary Digital Content 1, which shows the fishbone diagram) [29]. We used swimlane diagrams to map complex multidisciplinary system processes (See Supplementary Digital Content 2, which shows a sample swimlane diagram) [29].
Based on stakeholder team input, we identified guideline-based, specific communication of recommendations as the top priority to improve post-EGD care. The endoscopy report was identified as the ideal platform to communicate recommendations since it is completed by the providers who are best suited to provide the recommendations (endoscopist) at a time when all of the information for complete recommendations is available (post-procedure). It is also the single document that all team members review post-procedure, is stored in a designated results/procedures area of the EHR (thus unlikely to get obscured among other notes), and is available to primary care providers/patients via online portal.
To optimize delivery of thorough post-procedural recommendations, we developed integrated endoscopy report templates. Because post-procedure recommendations differ based on etiology of bleeding/risk of re-bleeding, we utilized the most widely accepted 2007 American Association for the Study of Liver Diseases guidelines on variceal UGIB [4], 2019 International Consensus Group guidelines on non-variceal UGIB [3], and established 2015 quality measures from the American Society of Gastrointestinal Endoscopy/American College of Gastroenterology Task Force on Quality in Endoscopy[5] to build five etiology- and severity-specific note templates within institutional endoscopy software (Provation, Minneapolis, Minnesota) (Table 1). Guided by stakeholder feedback, we built three core templates in summer 2020 (high-risk non-variceal UGIB, low-risk non-variceal UGIB, variceal UGIB) and two additional templates in February/March 2021 (portal hypertensive gastropathy and obscure overt GI bleeding) (See Supplementary Digital Contents 3–7, which show sample templates). After the templates were pilot-tested among 3 endoscopists over a four-week period, 39 gastroenterology/hepatology faculty, and 15 gastroenterology fellows completed a 10-min training session on template content (i.e., free-text and selectable options for core templates) and use (i.e., workflow to access templates) led by TY.
Data Collection and Outcomes
All eligible upper endoscopies were identified from institutional endoscopy software (Provation). Data collection was performed through a combination of structured EHR data output (Provation) and manual chart review (Epic, Verona, Wisconsin) [30]. Accuracy of data entry was audited by two independent personnel (TY, JE) for 10% of all data entries. All data were collected and managed using Research Electronic Data Capture (REDCap) [31]. Retrospective pre-intervention data on all consecutive patients were collected from December-2019 to January-2020, and one-week blocks were collected from June-2019 to November-2019 using simple randomization to ensure pre-intervention data were representative of rotating provider schedules. Post-intervention data were collected November-2020 through July-2021 after the intervention was implemented in October-2020. We collected patient demographics, American Society of Anesthesiologists (ASA) classification, date/time of procedure, daily endoscopy center procedural volume, provider specialty, trainee involvement, level of care, admission diagnosis, hospital length of stay, readmission within 30 days of discharge for diagnosis of gastrointestinal bleeding or anemia, same-day colonoscopy, endoscopy findings, and interventions.
We collected provider process metrics including completeness (present/absent) of documentation of standard-of-care recommendations (patient disposition, diet, medications, re-bleeding scenarios, repeat endoscopy) and usage of templates. To measure the burden of our intervention on workload, the number of mouse “clicks,” free-text characters, and time required to document a complete endoscopic report was recorded/compared in a testing session with and without the use of each template.
We collected clinical care metrics including standard-of-care medication regimens and appropriate planning for repeat EGD when indicated. Standard-of-care medication regimens were defined as adherence to the regimen recommended in the endoscopy report or guideline-based regimens [3,4,5] based on lesion and intervention success. Inpatient medication regimens were considered compliant if implemented within 24-h post procedure. Outpatient medication regimens were considered compliant if the discharge prescription was for the correct class and dose of medication and if an appropriate stop-date was noted on the discharge prescription. Plans for repeat EGD, if indicated based on culprit lesion or stated recommendation, was considered compliant if a follow-up EGD was scheduled or ordered by the day of discharge from the hospital.
We defined a Minimal Standard Report (MSR) consisting of disposition, diet, and etiology-specific medication recommendations.
Iterative Quality Improvement
After core templates were implemented in October-2020, we utilized stakeholder feedback and Pareto charting (See Supplementary Digital Content 8, which shows a sample Pareto chart) to target areas for high-impact iterative improvements. Pareto charting, based on the principle that 80% of a problem derives from 20% of the causes, tracks the frequency of individual defects (i.e., process/clinical care metrics) and their cumulative impact on non-compliance (i.e., MSR and overall care non-compliance) [32].
Our iterative improvements included refinement of template content, addition of “obscure overt gastrointestinal bleeding” & “portal hypertensive gastropathy” templates, refinement of existing EHR gastroenterology consult notes, and training of new first-year fellow providers at 3, 5, 7, and 9 months after core template implementation (Fig. 1).
A Process metrics over time. B Clinical care metrics over time. (a) Core Template Implementation (b) Template content refinement, (c) Template addition (obscure overt bleeding & portal hypertensive gastropathy), (d) Electronic health record consult note refinement, (e) First year fellow orientation. *Stakeholder interviews
Sample Size and Statistical Analysis
To have 80% power to detect a 20% improvement in inpatient PPI dose/route, discharge PPI dose/frequency and repeat EGD recommendation, assuming a baseline performance of 40%, a minimum of 97 patients in each group pre- and post- intervention were required, respectively.
Means and frequencies were calculated. Chi-square tests were used to compare pre- and post-intervention baseline characteristics, process, and clinical care metrics. Multivariable logistic regression was performed on all significant covariates with p value less than 0.05. All tests were two-sided and evaluated at an alpha of 0.05, unless otherwise specified. R Version 4.0.2 (R Core Team, 2020) was used for all analyses.
Results
Of 658 patients who underwent inpatient EGD for UGIB, 146(22.2%) had varices, 127(19.3%) had portal hypertensive gastropathy, 347(52.7%) had excavated/inflammatory lesions (ulcer/erosion, Cameron lesion, Mallory–Weiss tear, esophagitis, gastritis, or duodenitis), 36(5.5%) had vascular lesions (Dieulafoy lesion, arteriovenous malformation/ectasia, gastric antral vascular ectasia), and 12(1.8%) had malignancy. 462(70.2%) had multiple coexisting lesions (Table 2).
When comparing baseline characteristics of 199 patients pre-intervention versus 459 patients post-intervention, patients in the post-intervention group had more advanced ASA classification (82.6 vs 58.3%, p < 0.001), higher risk lesions (33.3% vs 22.7%, p = 0.007), and more concurrent lesions (73.2% vs 63.3%, p = 0.011). Overall endoscopy center procedural volume (41.3 vs 51.1 procedures/day, p < 0.001) was lower in the post-intervention period. There were otherwise no significant differences in patient, procedural, or lesion characteristics (Table 2).
Process Metrics
Workload was reduced by a mean of 33 “clicks,” 356 free-text characters, and 2 min per report. Template usage remained above 75% after implementation (Fig. 1A) for an aggregate utilization of 82.6%. Inclusion of diet and disposition recommendations in the EGD report significantly improved from 63.3 and 66.8% pre-intervention, to 73.0% and 75.4% post-intervention (p = 0.013 and p = 0.024), respectively. Re-bleeding guidance recommendations also improved from 18.6 to 43.8% (p < 0.001). Other metrics did not significantly change after intervention. Overall fulfillment of MSR criteria significantly improved from 28.6 to 42.5% (p < 0.001) (Table 3).
Clinical Care Metrics
Among those with non-portal hypertensive bleeding, compliance with inpatient and discharge PPI prescriptions improved from 53.4% and 31.3% to 77.9% and 61.0%, respectively, after intervention (p < 0.001). Among those with variceal bleeding, compliance with inpatient octreotide orders improved from 75.0 to 93.6% after intervention (p = 0.002). Planning of repeat EGD, when indicated, improved from 61.3 to 87.1% after intervention (p < 0.001). There was no significant change in antibiotic orders and post-discharge re-bleeding (Table 3).
Although the intervention was implemented in October-2020, iterative improvements were made thereafter. Planning of repeat EGD and compliance with inpatient and discharge PPI prescriptions continued to improve over time (Fig. 1B).
After implementation, among 77 cases of non-variceal bleeding with non-compliant inpatient PPI regimens, 71(92.2%) received overtreatment due to excess IV PPI. Among 136 non-variceal cases with non-compliant discharge PPI prescriptions, 100(73.5%) received overtreatment due to indefinite duration of twice daily oral PPI.
Among 59 cases after implementation where a follow-up EGD was indicated, but not ordered, 20 (33.9%) were for follow-up of varices, 24 (40.7%) for follow-up of Los Angeles classification grade C or D esophagitis to exclude Barrett’s-related neoplasia, 3 (5.1%) for follow-up of gastric ulcers to exclude malignancy, and 12(20.3%) for other indications. 44 (74.6%) reports recommended follow-up EGD but did not have a repeat EGD ordered, while 15 (25.4%) reports did not provide a recommendation for repeat EGD.
Predictors of Compliance with Process and Clinical Care Metrics
Templates were used more often in male patients, patients admitted for gastrointestinal bleeding/anemia, patients with high-risk lesions, cases in the intensive care unit or operating room (versus the endoscopy suite), patients who had EGD only (versus EGD/colonoscopy), procedures done on the weekend and days with lower overall endoscopy volume (See Supplementary Digital Content 9, which shows covariate factors associated with template usage). On multivariable analysis, only single-procedure EGD (compared to simultaneous EGD/colonoscopy) was associated with an increased probability of usage of templates (Odds Ratio 7.07[95% Confidence Interval 3.97–12.58], p < 0.001).
Compliance with inpatient PPI regimen was higher with shorter length of stay (8.5 vs 17.1 days, p < 0.001) and floor-status level of care (80.8% vs 64.5%, p = 0.005). Discharge PPI prescription compliance was higher with fellow involvement (64.4% vs 52.5%, p = 0.040), longer lengths of hospitalization (11.8 vs 8.2 days, p = 0.023), and simultaneous EGD/colonoscopy (75.7% vs 57.3%, p = 0.005). Other factors were not associated with PPI compliance (Table 4). There were no significant factors associated with planning of repeat EGD (Table 5).
Conclusions
Implementation of endoscopy software templates improved adherence to guideline-based care for adults hospitalized with UGIB during their inpatient stay and after a transition out of the hospital. This QI project resulted in increased compliance with medication and follow-up EGD recommendations provided by endoscopists in a large academic teaching hospital. Templates were highly utilized, improved clinical workflows, and enhanced MSR completion facilitating communication of high-quality, comprehensive post-procedure recommendations to multidisciplinary inpatient teams.
Our intervention provided anticipatory guidance to endoscopists and multidisciplinary healthcare providers in a manner that improved efficiency of clinical workflow. While prior QI studies have utilized endoscopy templates to improve documentation [19, 33], our study further demonstrated the positive impact of such an intervention on clinical behavior, such as planning of repeat endoscopy and medication prescriptions. Incorporation of such standardized templates with discrete trackable data can also serve as an infrastructure for quality assurance programs, as done in prior QI studies with colonoscopy [34].
Several factors contributed to the success of our intervention. First, we leveraged the EHR to simultaneously standardize and improve ease of documentation. While clinical decision support and EHR “macro” templates have been implemented elsewhere [35], we optimized choice architecture by limiting the number of templates and minimizing interruption to pre-existing clinical workflow. We intentionally selected the procedure note for template implementation as this is where most inpatient teams looked in their existing workflows for post-procedure recommendations. This decision likely contributed to the uptake of endoscopist recommendations by primary teams. Second, our templates did not require extensive end-user education/training, allowing us to efficiently train faculty and trainees. Third, the anticipatory guidance provided by our templates had the potential to decrease downstream burden of work due to multidisciplinary miscommunication.
There were several interesting findings. First, we observed more high-risk and concurrent culprit lesions for UGIB in sicker patients post-intervention compared to pre-intervention. Given the onset of the coronavirus-19 pandemic after implementation, this may be related to the overall delay in medical care or disparities in the presentation of UGIB observed in other studies although data regarding timing of EGD and coronavirus-19 status were unavailable [36, 37]. It is possible that the higher acuity nature of these patients contributed to the unchanged post-discharge bleeding. Second, during our pre-intervention period from June–October 2019, outpatient PPI compliance decreased. This was largely due to over-prescription of PPIs. While we are uncertain of the cause, this did coincide with initial carcinogenic concerns around ranitidine, perhaps directing patients toward PPIs instead [38]. After implementation, the majority of non-compliant prescriptions were due to overuse.
Our study highlights areas that require additional study. It is unclear why several process metrics (PPI, repeat EGD, antibiotic, and octreotide recommendations) and antibiotic regimen compliance did not significantly improve after intervention. These process metrics may be perceived as less clinically relevant by endoscopists, and indications for antibiotic prophylaxis are often subject to competing comorbidities. Compliance with guideline-adherent inpatient PPI regimens was associated with shorter hospitalizations and lower acuity, while compliance with discharge PPI prescriptions was associated with fellow involvement, longer hospitalizations, and simultaneous EGD/colonoscopy. Hospital length of stay appears to be important in facilitating compliance with medication recommendations in the inpatient and outpatient setting. This is important to continue to examine in future iterations of this work given efforts nationwide to decrease hospital length of stays, ideally within the context of broader QI programs similar to the United Kingdom UGIB clinical care “bundle” [39].
Our study has several limitations. First, the process metrics were limited to the presence/absence of MSR components rather than the quality of such components. This was done to minimize bias in interpretation of written recommendations and allow for deviations from standard-of-care based on endoscopist discretion. Second, our templates were not used in every case of endoscopy for UGIB. While the vast majority of UGIB should follow established guidelines, we recognize a certain subset of complex scenarios may be ill-suited to a standardized workflow. We were unable to assess the impact of template usage on clinical care because only 80 cases (17.4%) did not use templates and the event rates for process/clinical metrics were too low to assess clinical/statistical significance. Third, of reports that did not receive an indicated follow-up EGD, the majority had a recommendation in the report but no order. We recognized this as a barrier in EHR interoperability, which has been recognized as an ongoing global challenge [40]. Fourth, the success of endoscopic template implementation is subject to an institution’s informatics infrastructure [41]. For example, templates were used less frequently after simultaneous EGD/colonoscopy, likely due to fragmented documentation workflow when transitioning between procedures. Finally, we were not powered for an interrupted time series or for measurement of outcomes such as missed neoplasia or adverse medication effects. This was outside the scope of a pre/post-design QI study and should be assessed in larger, potentially multicenter and international, pragmatic randomized controlled trials.
In summary, we leveraged the EHR to standardize, improve, and streamline endoscopic documentation after UGIB with subsequent improvement in clinical care behavior. We were also able to identify factors associated with non-compliance to guide future adaptations of our intervention with the goal of continued quality improvement. Future studies should be done to examine the sustainability of this intervention over time, as well as expand templates to other endoscopic scenarios including colonoscopy or advanced endoscopic procedures for a variety of indications.
Abbreviations
- ASA:
-
American Society of Anesthesiologists
- EGD:
-
Upper endoscopy
- GI:
-
Gastrointestinal
- HER:
-
Electronic health record
- IV:
-
Intravenous
- MSR:
-
Minimal-standard-report
- QI:
-
Quality improvement
- UGIB:
-
Upper gastrointestinal bleeding
References
HCUP Fast Stats - Most Common Diagnoses for Inpatient Stays. site]. Available at www.hcup-us.ahrq.gov/faststats/national/inpatientcommondiagnoses.jsp?year1=2015&characteristic1=44&included1=0&year2=&characteristic2=0&included2=1&expansionInfoState=hide&dataTablesState=hide&definitionsState=hide&exportState=hide.
Mathews SC, Izmailyan S, Brito FA, et al. Prevalence and Financial Burden of Digestive Diseases in a Commercially Insured Population. Clin Gastroenterol Hepatol. 2021.
Barkun AN, Almadi M, Kuipers EJ et al. Management of Nonvariceal Upper Gastrointestinal Bleeding: Guideline Recommendations From the International Consensus Group. Ann Intern Med. 2019;171:805–822.
Garcia-Tsao G, Sanyal AJ, Grace ND et al. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Hepatology. 2007;46:922–938.
Cohen J, Pike IM. Defining and measuring quality in endoscopy. Gastrointest Endosc. 2015;81:1–2.
Campbell HE, Stokes EA, Bargo D et al. Costs and quality of life associated with acute upper gastrointestinal bleeding in the UK: cohort analysis of patients in a cluster randomised trial. BMJ Open. 2015;5:e007230.
Mahmud N, Serper M, Taddei TH, et al. The Association between Proton Pump Inhibitor Exposure and Key Liver-Related Outcomes in Patients with Cirrhosis: A Veterans Affairs Cohort Study. Gastroenterology. 2022.
Shallcross LJ, Davies DS. Antibiotic overuse: a key driver of antimicrobial resistance. Br J Gen Pract. 2014;64:604–605.
Katz PO, Dunbar KB, Schnoll-Sussman FH, et al. ACG Clinical Guideline for the Diagnosis and Management of Gastroesophageal Reflux Disease. Official journal of the American College of Gastroenterology | ACG. 2022:https://doi.org/10.14309/ajg.0000000000001538.
Carroll AE. The High Costs of Unnecessary Care. JAMA. 2017;318:1748–1749.
Arguedas MR, Heudebert GR, Eloubeidi MA et al. Cost-effectiveness of screening, surveillance, and primary prophylaxis strategies for esophageal varices. Am J Gastroenterol. 2002;97:2441–2452.
Committee ASoP, Muthusamy VR, Lightdale JR, et al. The role of endoscopy in the management of GERD. Gastrointest Endosc. 2015;81:1305–1310.
Wan JJ, Fei SJ, Lv SX et al. Role of gastroscopic biopsy of gastric ulcer margins and healed sites in the diagnosis of early gastric cancer: A clinical controlled study of 513 cases. Oncol Lett. 2018;16:4211–4218.
Katzka DA, Pandolfino JE, Kahrilas PJ. Phenotypes of Gastroesophageal Reflux Disease: Where Rome, Lyon, and Montreal Meet. Clin Gastroenterol Hepatol. 2020;18:767–776.
Blackett JW, Faye AS, Phipps M et al. Prevalence and Risk Factors for Inappropriate Continuation of Proton Pump Inhibitors After Discharge From the Intensive Care Unit. Mayo Clin Proc. 2021;96:2550–2560.
Leri F, Ayzenberg M, Voyce SJ et al. Four-year trends of inappropriate proton pump inhibitor use after hospital discharge. South Med J. 2013;106:270–273.
Saini SD, Eisen G, Mattek N et al. Utilization of upper endoscopy for surveillance of gastric ulcers in the United States. Am J Gastroenterol. 2008;103:1920–1925.
de Lange T, Moum BA, Tholfsen JK et al. Standardization and quality of endoscopy text reports in ulcerative colitis. Endoscopy. 2003;35:835–840.
Ha NB, Ge J, Rubin JB, et al. S1223 Automated Endoscopy Template Improves Provider Adherence to Esophageal Varices Surveillance Guidelines. Official journal of the American College of Gastroenterology | ACG. 2020;115:S613-S614.
Westerveld D, Khullar V, Mramba L et al. Adherence to quality indicators and surveillance guidelines in the management of Barrett’s esophagus: a retrospective analysis. Endosc Int Open. 2018;6:E300–E307.
Aabakken L, Rembacken B, LeMoine O, et al. Minimal standard terminology for gastrointestinal endoscopy - MST 3.0. Endoscopy. 2009;41:727–728.
Korman L. Standardization of Endoscopy Reporting: Deja Vu All Over Again? Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association. 2012;10:956–959.
Starmer AJ, Spector ND, Srivastava R et al. Changes in medical errors after implementation of a handoff program. N Engl J Med. 2014;371:1803–1812.
Singh H, Spitzmueller C, Petersen NJ et al. Information Overload and Missed Test Results in Electronic Health Record-Based Settings. JAMA Internal Medicine. 2013;173:702–704.
Madden JM, Lakoma MD, Rusinak D et al. Missing clinical and behavioral health data in a large electronic health record (EHR) system. Journal of the American Medical Informatics Association. 2016;23:1143–1149.
O’Daniel M and Rosenstein A. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville (MD): Agency for Healthcare Research and Quality; 2008.
Tian W. An All-Payer View of Hospital Discharge to Postacute Care, 2013. In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville (MD): Agency for Healthcare Research and Quality (US); 2016:Table 3, Hospital bed size categories.
Ogrinc G, Davies L, Goodman D, et al. SQUIRE 2.0 (Standards for QUality Improvement Reporting Excellence): Revised Publication Guidelines From a Detailed Consensus Process. J Nurs Care Qual. 2016;31:1–8.
Harel Z, Silver SA, McQuillan RF et al. How to Diagnose Solutions to a Quality of Care Problem. Clin J Am Soc Nephrol. 2016;11:901–907.
Weiskopf NG, Cohen AM, Hannan J et al. Towards augmenting structured EHR data: a comparison of manual chart review and patient self-report. AMIA Annu Symp Proc. 2019;2019:903–912.
Harris PA, Taylor R, Thielke R et al. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381.
Harolds J. Quality and Safety in Health Care, Part I: Five Pioneers in Quality. Clin Nucl Med. 2015;40:660–662.
Harris N, Telford J, Yonge J et al. Improvement of Endoscopic Reports with Implementation of a Dictation Template. J Can Assoc Gastroenterol. 2021;4:21–26.
Ladabaum U, Shepard J, Mannalithara A. Developing and Deploying an Automated Quality Reporting System in Your Practice: Learning From the Stanford Colonoscopy Quality Assurance Program. Am J Gastroenterol. 2021;116:1365–1370.
Louissaint J, Grzyb K, Bashaw L, et al. An Electronic Decision Support Intervention Reduces Readmissions for Patients With Cirrhosis. Am J Gastroenterol. 2022.
Mark ÉC, Kristy M, Kristie ENC et al. Delay or avoidance of medical care because of COVID-19-related concerns - United States, June 2020. MMWR Morb Mortal Wkly Rep. 2020;69(36):1250–1257.
Reddy S, Patel B, Baldelli L et al. Decreased Rate of Presentation, but Worsened Racial-Ethnic Disparity in Acute Gastrointestinal Bleeding During Coronavirus 2019 Shutdown: A Retrospective Cohort Study. Clinical and Experimental gastroenterology. 2022;15:67–77.
Wagner JA, Colombo JM. Medicine and Media: The Ranitidine Debate. Clin Transl Sci. 2020;13:649–651.
Siau K, Hearnshaw S, Stanley AJ et al. British Society of Gastroenterology (BSG)-led multisociety consensus care bundle for the early clinical management of acute upper gastrointestinal bleeding. Frontline Gastroenterology. 2020;11:311–323.
Reisman M. EHRs: The Challenge of Making Electronic Data Usable and Interoperable. P T. 2017;42:572–575.
Allen JI, Berry S. Next Generation Academic Gastroenterology. Clin Gastroenterol Hepatol. 2022;20:5–8.
Funding
Open access funding provided by SCELC, Statewide California Electronic Library Consortium. University of Colorado Hospital/School of Medicine Clinical Effective and Patient Safety Small Grants Program for Residents and Fellows (CEPS-RF); NIH/NCRR Colorado CTSI Grant Number UL1 RR025780 (Redcap) (Grant No. 63503482).
Author information
Authors and Affiliations
Contributions
TY (study concept and design; acquisition of data; analysis and interpretation of data; drafting of the manuscript; critical revision of the manuscript for important intellectual content; statistical analysis; obtained funding; administrative, technical, or material support; study supervision), JME (acquisition of data), SS (study concept and design; critical revision of the manuscript for important intellectual content), JP (study concept and design; critical revision of the manuscript for important intellectual content), BJ (critical revision of the manuscript for important intellectual content), AD (critical revision of the manuscript for important intellectual content), SW (critical revision of the manuscript for important intellectual content), FIS (critical revision of the manuscript for important intellectual content), SGP (study concept and design; critical revision of the manuscript for important intellectual content; obtained funding; study supervision).
Corresponding author
Ethics declarations
Disclosures
TY: Supported by University of Colorado Hospital/School of Medicine Clinical Effective and Patient Safety Small Grants Program for Residents and Fellows (CEPS-RF). SS: Research support from the National Palliative Care Research Center. JE, JP, BJ, AD: None. SW: Consultant Boston Scientific, Medtronic, Cernostics, Interpace, Exact Sciences. Research Support from Lucid, CDx, Ambu, Supported by NIH/NIDDK U34DK124174, U01DK129191. FIS: Consultant to Janssen, Merck, and Takeda Pharmaceuticals. He has received research funding from Takeda, Janssen, and the Crohn’s and Colitis Foundation. SGP: Olympus America (research support), ERBE USA (honorarium), Research support from the American Cancer Society. Writing Assistance: None. Guarantor of article: Timothy Yen MD.
Ethical approval
The study was exempt as “Not-Human Subject Research” after review by the Colorado Multiple Institutions Review Board.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Yen, T., Jones, B., Espinoza, J.M. et al. Optimizing Endoscopy Procedure Documentation Improves Guideline-Adherent Care in Upper Gastrointestinal Bleeding. Dig Dis Sci 68, 2264–2275 (2023). https://doi.org/10.1007/s10620-023-07823-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-023-07823-6