Abstract
Introduction
Patients with cirrhosis have a higher risk of severe COVID-19 and mortality and are high-priority patients for vaccination. However, cirrhotics were excluded from the phase 2/3 vaccine trials. Hence, we aimed to assess the antibody response and safety of Covishield (ChAdOx1nCoV-19) among patients with cirrhosis.
Methods
Patients who attended the tele-hepatology services at our institute from March 2020 to June 2021 and diagnosed with cirrhosis as per their medical records were telephonically interviewed in July 2021 using a pre-specified questionnaire. Patients who had completed 2 doses of ChAdOx1-nCOV (with the 2nd dose administered at least 2 weeks back) and without history of documented COVID-19 infection (pre- or post-vaccination) were tested for antibodies against the spike protein. Seropositive patients were divided into high, moderate, and low antibody responses based on the signal/cut-off.
Results
We interviewed 784 patients with cirrhosis. At least 1 dose of ChAdOx1-nCOV was received by 231 patients among whom 134 (58%) had received 2 doses. Documented COVID-19 was reported in 3.9% patients who received at least 1 dose of ChAdOx1-nCOV including breakthrough infections in 3.7% patients vaccinated with 2 doses. Local and systemic adverse events were reported by 42% and 22.1% patients. None developed anaphylaxis, acute decompensation, acute-on-chronic liver failure, or other serious adverse events requiring hospitalization. Seroconversion was documented in 81 (92%) out of 88 patients. No difference was observed in level of antibody response between patients with compensated and decompensated cirrhosis (p = 0.12).
Conclusion
Our preliminary data suggest that ChAdOx1-nCOV is safe with high seroconversion rates in patients with cirrhosis.
Similar content being viewed by others
Lay Summary
ChAdOx1-nCOV is safe with high seroconversion rates in patients with cirrhosis. Antibody response is not affected by the severity of liver disease.
Introduction
Vaccines have emerged as a primary line of defense against the scourge of COVID-19 which continues to rage across the world and India. In India, currently two vaccines namely ChAdOx1-nCOV (Covishield) and BBV-152 (Covaxin) are being administered by the government under national program in adults while several others are under regulatory consideration. ChAdOx1-nCOV uses a replication incapable chimpanzee adenovirus as a vector for transporting the gene encoding for the COVID-19 spike protein while BBV-152 is a whole-virion-inactivated vaccine [1]. Unlike the available mRNA vaccines (BNT162b2; BioNTech SE/Pfizer or mRNA-1273; Moderna Biotech), both these vaccines have less stringent storage requirements of 2–8 degrees centigrade which is a major advantage in resource constrained settings like India where maintenance of cold chain is a challenge [1].
Cirrhosis is characterized by immune dysregulation and rebalanced hemostasis with a prothrombotic tendency [2, 3]. Some evidence suggests that patients with cirrhosis may be at a higher risk of acquiring COVID-19 [4]. More importantly, overwhelming evidence suggests that there is a stepwise increase in the risk of severe COVID-19, hospitalization, and mortality with increasing severity of cirrhosis as assessed by Child-Turcotte-Pugh (CTP) and model for end-stage liver disease (MELD) scores [5, 6]. COVID-19 can also precipitate acute-on-chronic liver failure in these patients which portends a dismal prognosis [4,5,6,7]. Thus, patients with cirrhosis should be considered a high-priority population for vaccination against COVID-19 [1, 4, 8, 9].
Although cirrhosis should be considered a priority group for vaccination, there are little data on the safety and efficacy of COVID-19 vaccines in these patients as cirrhosis was an exclusion criterion in the phase 2/3 trials of these vaccines. Cirrhosis is a state of immune dysfunction and has been associated with impaired antibody response against other vaccines like Hepatitis B and pneumococcus [10, 11]. A similar poor response against COVID-19 vaccines may not be an unreasonable speculation [1, 8]. Thus, the assessment of safety and efficacy of COVID-19 vaccine in cirrhosis is an urgent unmet need and we aimed to assess the antibody response and safety of ChAdOx1-nCOV in Indian patients with cirrhosis.
Methods
All patients who had registered for tele-hepatology services at our institute in northern India from March 2020 to June 2021 and diagnosed with cirrhosis as per their medical records were considered for the study. Cirrhosis was diagnosed on the basis of history, blood investigations, imaging, or endoscopic findings. All these patients were contacted telephonically in July 2021 and were interviewed using a pre-specified proforma regarding history of documented COVID infection in self or family and its severity, COVID-19-specific symptoms, vaccination status (type and number of doses), adverse events following vaccination, history of clinical decompensations (ascites, variceal bleed and hepatic encephalopathy), presence of medical co-morbidities apart from cirrhosis, and medications. Medical records of the patients were also reviewed to ascertain the etiology of liver disease, presence of medical co-morbidities and the last available CTP and MELD scores within 1 month prior to vaccination. Patients who could not be contacted despite repeated telephonic attempts for 3 consecutive days were excluded from the study. Vaccination status, type of vaccine, and dates of vaccine administration were confirmed from the COVID-19 vaccination certificate issued by the Government of India.
All patients who had completed full course of ChAdOx1-nCOV vaccine (with the second dose being administered at least 2 weeks back) and without history of documented COVID-19 infection (pre- or post-vaccination) in self or immediate family members (residing with the patient) were asked to visit our institute physically and blood samples were collected for complete hemogram and liver function. IgG antibodies against the spike protein of COVID-19 were tested using an automated, chemiluminescent assay (Ortho Clinical Diagnostics) which has shown sensitivity and specificity of 97.3% and 99.6%, respectively, for the detection of antibodies in convalescent sera collected more than 2 weeks after positive reverse transcriptase PCR result [12]. This test has also been shown to exhibit relatively high linear regression with NT50 values in pseudo virus neutralization assays [13]. Informed consent was taken from all patients. The study was approved by the institutional ethics committee and has been reported in accordance with the STROBE guidelines.
Definitions
Documented COVID-19 infection was defined as positive test for SARS-CoV-2 using RT-PCR or rapid antigen tests. Patients who had received both doses of ChAdOx1-nCOV were considered as completely vaccinated. All adverse events following vaccination reported by the patient were noted irrespective of whether they were deemed to be related or co-incidental. Local adverse events were defined as complications at or around the injection site including pain, swelling, tenderness, redness, etc., while systemic adverse effects were defined as the new onset of systemic complaints including but not limited to fever, chills and rigor, headache, myalgia, fatigue, diarrhea, nausea, and vomiting. Serious adverse event was denoted as any event requiring hospitalization.
Breakthrough infections were defined as documented COVID-19 infection occurring after at least 2 weeks of complete vaccination. Severity of post-vaccination COVID-19 was graded as mild, moderate, or severe as per the ordinal scale recommended by the Indian Council of Medical Research. Briefly, mild COVID-19 includes patients without dyspnea or hypoxia who do not need hospitalization, moderate COVID-19 includes those with dyspnea with respiratory rate ≥ 24/min or arterial oxygen saturation of 90–93% (on room air) who require admission to hospital ward , while severe disease includes patients with respiratory rate > 30/min or arterial oxygen saturation of < 90% (on room air) who require admission to HDU or ICU.
Seroconversion post-vaccination was identified by the presence of antibody against spike protein with a signal/cut-off ratio of > 1 as per the manufacturer’s instructions (Ortho Clinical Diagnostics). Depending upon the signal/cut-off ratio, antibody response in seropositive patients was further subcategorized into low (signal/cut-off: 1 to ≤ 4.62), moderate (signal/cut-off: > 4.62 to ≤ 18.45) , and high (signal/cut-off > 18.45). The upper cut-off of 18.45 has been previously shown to have a specificity of 90% for the detection of neutralization at a dilution of 1:2560 or higher while the lower cut-off of 4.62 has a sensitivity of 90% for detecting neutralizing antibody titers of 1:160 or higher [14]. These cut-offs for categorization into low, moderate, and high antibody levels have been previously used for categorizing antibody titers in convalescent plasma [14].
Decompensated cirrhosis was defined as CTP class B or C or the presence of clinical decompensations (ascites, hepatic encephalopathy, or variceal bleed). Acute decompensation was defined as new onset or acute worsening of clinical decompensation. ACLF was defined as per the European Association for the Study of the Liver (EASL)–Chronic Liver Failure (CLIF) Consortium Acute-on-Chronic Liver Failure in Cirrhosis (CANONIC) criteria.
Outcomes
The primary outcome of our study was the seroconversion rate following complete vaccination with ChAdOx1-nCOV. Secondary outcomes included adverse events and documented COVID-19 infections after vaccination with ChAdOx1-nCOV (single and both doses) and level of antibody responses at least two weeks after administration of the second dose. Date of documented COVID-19 infection post-vaccination was verified from the RT-PCR or rapid antigen test reports.
Sample Size Calculation
In healthy individuals, seroconversion has been reported in > 95% patients after 2 doses of ChAdOx1-nCOV in various studies including those from the Indian [15,16,17,18,19]. To evaluate a similar proportion of 95% with a precision of estimate of 0.05 at a confidence level of 95%, the minimum required sample size was calculated as 83 patients.
Statistical Analysis
The data were analyzed using MedCalc® Statistical Software version 20.027 (Ostend, Belgium). Quantitative data have been expressed as mean ± standard deviation or median (range). Normality of data was assessed using D'Agostino-Pearson test. Qualitative data have been expressed as proportions and percentages. Quantitative data were compared using t-test or Mann–Whitney test as applicable. Qualitative data were assessed using Fischer’s exact test. Comparison of degree of antibody responses between patients with compensated and decompensated cirrhosis was done using Chi-squared test for trend. Correlations were assessed using Kendall’s tau and scatter diagrams. All statistical tests were run two sided and p value of < 0.05 was considered statistically significant.
Results
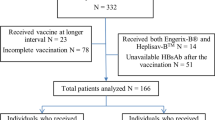
Out of 1037 patients with cirrhosis, 784 could be contacted telephonically for interview. Among them 501 patients were unvaccinated. Out of the 283 vaccinated patients, 52 (18.37%) had received BBV-152 (Supplementary Table 1). The remaining 231 (81.62%) patients had received ChAdOx1-nCOV and were the main focus of our study (Fig. 1).
Most of the patients who received at least one dose of ChAdOx1-nCOV (n = 231) were in the 5th decade with a mean age of 53.3 ± 10.08 years. Majority were males (76.2%). The commonest etiology was alcohol (31.6%) followed by non-alcoholic fatty liver disease (NAFLD) (27.3%) and chronic viral hepatitis (26%). The mean MELD score in the patients was 12.21 ± 1.69 and 182 (78.8%) patients had decompensated cirrhosis. The clinical and demographic characteristics of the patients who received at least a single dose of ChAdOx1-nCOV are shown in Table 1. One hundred and thirty-four (58%) of these 231 patients had received complete vaccination with two doses of ChAdOx1-nCOV with an interval of 35 (28–50) days between the two doses. The median interval between the administration of the second dose and day of telephonic interview in these 134 patients was 37 (22–73) days.
Among patients who had received at least one dose of ChAdOx1-nCOV, local adverse events were reported by 97 (42%) patients while systemic adverse events were reported by 51 (22.1%) patients. The most common systemic adverse events were fever in 35 patients (15.2%), myalgia in 15 (6.5%), flu-like symptoms in 8 (3.5%), and headache in 7 (3%) patients (Table 2). None of the patients had anaphylaxis. No serious adverse event requiring hospitalization was reported. All adverse events were self-limiting occurring and resolving within 72 h of vaccination. None of the patients developed acute decompensation or ACLF post-vaccination.
Documented COVID-19 after vaccination was seen in 9 (3.9%) out of the 231 patients who received at least a single dose of ChAdOx1-nCOV including 5 documented breakthrough infections (3.7%) in the 134 completely vaccinated patients. Seven of these 9 patients had decompensated cirrhosis. All patients had mild COVID-19, and none required oxygen supplementation or hospitalization. COVID-19 did not precipitate acute decompensation or ACLF in any of these patients with underlying cirrhosis. The interval between the administration of the second vaccine dose and the documentation of breakthrough COVID-19 was 31 (21–43) days.
All patients who were completely vaccinated with ChAdOx1-nCOV and did not have history of documented COVID-19 in self or immediate family (n = 112, Fig. 1) were invited to come to our institute for collection of blood samples. However, due to COVID-19-related mobility restrictions, only 88 patients turned up and were sampled (Table 1). Median duration between sampling and the last dose of ChAdOx1-nCOV was 39 (23–76) days. None of these patients were on immunosuppressive medications. Pre-vaccination CTP and MELD scores were available in all these patients. There was no difference in pre-vaccination and post-vaccination CTP (7.92 ± 1.09 vs 7.97 ± 1.11, p = 0.77) and MELD (12.33 ± 1.65 vs 12.54 ± 1.71, p = 0.81) scores in these patients. Antibodies against COVID-19 were detectable in 81 (92.1%) patients and the antibody response was graded as low, moderate, and high in 6 (6.8%), 68 (77.3%), and 7 (8%) patients, respectively. There was no difference in age, gender, etiology of cirrhosis, and liver disease severity scores between seroconverted patients and those without detectable antibodies (Table 3). In seroconverted patients, the average signal/cut-off ratio and the degree of antibody response did not differ between patients with compensated or decompensated cirrhosis (p < 0.05, Table 4). There was no correlation between the signal/cut-off ratio and CTP (tau: 0.11, p = 0.13) or MELD (tau: 0.09, p = 0.19) scores in seroconverted patients (Fig. 2).
Antibody screening was also done in 12 patients who had received 2 doses of BBV-152 and was detectable in 11 (91.7%) patients. Data of these patients are shown in Supplementary Table 2.
Discussion
India rolled out its national COVID-19 vaccination program on January 16, 2021. In the first phase, vaccines were administered only to healthcare and frontline workers. In the second phase which was started on March 1, 2021, vaccinations were started for elderly individuals above the age of 60 years and patients above 45 years of age with comorbidities (including cirrhosis). Since May 1, 2021, all adults have been made eligible for vaccination as part of the 3rd phase. Although cirrhosis should be considered a high-priority group for vaccination, there are limited data on the safety and efficacy of COVID-19 vaccines in cirrhosis as patients with advanced liver disease were excluded from the phase 2/3 vaccine trials [1, 9, 20]. This lack of data may have resulted in hesitancy among the patients which may partially account for our observation that 501 (63.9%) of the 784 patients with cirrhosis telephonically surveyed by us in July, 2021, had not received even a single dose of COVID-19 vaccine.
ChAdOx1-nCOV, available in India as Covishield, was granted emergency use authorization and is being used in India since January 16, 2021, as part of the mass national vaccination campaign. We observed a high proportion of seroconversion (92.1%) in patients with cirrhosis following 2 doses of ChAdOx1-nCOV vaccine. This is comparable to the high seroconversion rate of 98% reported in the recently published pan-India coronavirus vaccine-induced antibody titer (COVAT) study in healthcare workers following two doses of ChAdOx1-nCOV [19]. It should be noted that the interval between the 2 doses of ChAdOx1-nCOV in the completely vaccinated patients in our cohort was 35 (28–50) days. Although not reported, the interval between the two doses is likely to have been similar in the COVAT study which included healthcare workers vaccinated till May 15, 2021. However, the current recommendation by the Government of India is to administer two doses of ChAdOx1-nCOV 12–16 weeks apart which came into practice following a notification issued on May 13, 2021. The optimal duration between the two doses of ChAdOx1-nCOV has been a subject of much debate and it has been suggested that a shorter interval between the two doses may be more effective against the delta variant [21,22,23]. Importantly, the relation of antibody responses with varying dose intervals in patients with cirrhosis may not be similar to that in healthy individuals and remains an unexplored area which should be assessed in future studies.
Most of the published data on seroconversion rates in cirrhosis following COVID-19 vaccination are with mRNA vaccines (BNT162b2; BioNTech SE/Pfizer or mRNA-1273; Moderna Biotech) or whole-virion-inactivated vaccines (CoronaVac, BBIBP-CorV, or WIBP-CorV) and seroconversion rates following ChAdOx1-nCOV vaccine are relatively unexplored [24,25,26,27,28,29,30]. The seroconversion rate of 92.1% observed in our cohort of patients with cirrhosis is similar to the impressive seroconversion rate of 96–100% reported by various studies using two doses of mRNA vaccines in cirrhosis [24,25,26,27,28]. However, the seroconversion rate of 66.1–78.9% with whole-virion-inactivated vaccines (CoronaVac, BBIBP-CorV, or WIBP-CorV) reported in two multicentric studies from China appear to be substantially lower than what was observed by us with ChAdOx1-nCOV or has been previously reported with mRNA vaccines [29, 30]. However, firm conclusions cannot be drawn in the absence of head-to-head trials. None the less, this information is particularly relevant in the Indian context as BBV-152, which is the other major vaccine that is being used by the Government of India in the national immunization program, is also a whole-virion-inactivated vaccine. Although out of protocol, we assessed antibody response in 12 patients who had been completely vaccinated with BBV-152 and documented seroconversion in 91.7% of the patients. In light of these observations, larger studies assessing seroconversion following vaccination with BBV-152 among patients with cirrhosis is the need of the hour.
Some evidence suggests that the antibody titers induced by mRNA vaccines in patients with cirrhosis may be lower than that in healthy individuals without liver disease [26]. Further, Thuluvath et al. reported suboptimal antibody responses in 19% patients with optimal antibody levels in 77.2% of 79 patients with cirrhosis [24]. On the contrary, a study from Greece reported adequate neutralizing activity in 92.1% of the 38 patients with cirrhosis following two doses of mRNA vaccines [28]. In our study, undetectable and low antibody responses were seen in 7 (7.9%) and 6 (6.8%) patients, respectively. Majority (85.3%) of our sampled patients had moderate or high antibody responses following two doses of ChAdOx1-nCOV. The clinical significance of differing antibody levels remains speculative. Antibodies against the spike protein have been shown to have a high correlation with protective neutralizing antibodies and with in vitro plaque neutralization tests [31, 32]. However, the exact level of protective antibodies remains largely unknown [33, 34]. Moreover, the clinical efficacy of any vaccine will also possibly depend on the prevalent strain. Our study was conducted during the second wave of the pandemic in India when the predominant strain in circulation was the delta (SARS-CoV-2 B.1.617.2) variant [35]. As such, seroconversion may be considered a reasonable pre-requisite for efficacy and our observations suggest that patients with cirrhosis have high seroconversion rates following 2 doses of ChAdOx1-nCOV which appears to be comparable to thar of healthy individuals. Our data also suggest that seroconversion and the degree of antibody response do not depend on the severity of liver disease as assessed using the CTP and MELD scores with no differences being observed between those with compensated or decompensated cirrhosis. However, our observations should not be extrapolated to other vaccine types.
Breakthrough infections following complete vaccination is being increasingly recognized in the real-world setting although the severity is usually mild. Real-world data on breakthrough infections following ChAdOx1-nCOV administration in India mainly come from cohorts of healthcare and frontline workers who were prioritized for vaccination during the first phases of vaccine roll-out. In the aforementioned COVAT study, breakthrough infections were noted in 5.5% of 399 healthcare workers who had received two doses of ChAdOx1-nCOV [19]. A large study in almost 1.6 million healthcare and frontline workers in the Indian Armed Forces reported a 93% reduction in breakthrough infections following ChAdOx1-nCOV [36]. At our institute, we have previously reported breakthrough infections in 1.6% of 3000 healthcare workers following complete vaccination with ChAdOx1-nCOV [37]. In our study, which was conducted during the second wave of the pandemic in India, we documented COVID-19 infections in 3.9% patients who had received at least one dose of ChAdOx1-nCOV and breakthrough infections in 3.7% following two doses of ChAdOx1-nCOV. Importantly, none of the 9 patients (7 of whom had decompensated cirrhosis) with documented COVID-19 infection following at least a single dose of ChAdOx1-nCOV developed severe COVID-19, acute decompensation, or ACLF. Although our study was neither designed nor powered for clinical efficacy, our preliminary observations are clinically informative and encouraging for patients with cirrhosis and their caregivers. Available data on clinical outcomes following COVID-19 vaccination in patients with cirrhosis are mainly with the use of mRNA vaccines [25, 38]. A propensity score-matched, retrospective analysis of the US Veteran Health Administration data reported a 78.6% reduction in COVID-19 infections with 100% reduction in COVID-19–related hospitalization or death following the administration of two doses of mRNA vaccines (Pfizer BNT162b2 mRNA and Moderna mRNA-1273) in patients with cirrhosis [38]. Analysis of the Veterans Outcomes and Costs Associated with Liver Disease (VOCAL) cohort also revealed an independent reduction in mortality following partial or complete vaccination with the aforementioned mRNA vaccines [25].
Given the fragile homeostatic balance in patients with cirrhosis, the scarcity of safety data of COVID-19 vaccines in these patients is worrisome [39]. Overall, ChAdOx1-nCOV was well tolerated by our cohort of patients with cirrhosis. Although local and systemic adverse effects were common, they were self-limiting and transient. There were no anaphylactic reactions or hospitalizations. Vaccination did not result in a worsening of liver function scores and did not precipitate acute decompensation or ACLF in any patient. Although, we acknowledge the possibility of recall bias in reporting these adverse events we believe that this would not be of much significance for serious events including hospitalizations.
We acknowledge the limitations of our study including the small sample size and the lack of healthy controls. Gold standard for the diagnosis of cirrhosis is liver histopathology which was not available in our patients. Apart from being vaccine induced, seroconversion also occurs following natural infection. We not only excluded patients with documented COVID-19 but also excluded patients with documented COVID-19 in family members residing with the patient as they were at a higher risk of having acquired COVID-19. However, we acknowledge that some of the patients may have mounted antibody responses secondary to asymptomatic, undocumented COVID-19. Additional assessment of antibodies against the nucleocapsid antigen may have given us more granular information in this regard. Further, we did not assess for T-cell responses. Finally, inclusion of patients through tele-hepatology services may have induced a potential selection bias. Nevertheless, our preliminary findings are clinically informative and should encourage patients with cirrhosis to participate in the global vaccination drive with the ultimate aim of attaining the holy grail of herd immunity.
In conclusion, vaccination with ChAdOx1-nCOV is safe in patients with cirrhosis and is associated with high rates of seroconversion. Seroconversion and the degree of antibody response in cirrhotics are not affected by the severity of liver disease (CTP or MELD scores) or the presence of decompensations. Further larger studies are urgently needed to corroborate our findings and to optimize dosing schedules in patients with cirrhosis.
Data availability
The data that support the findings of this study are available from the corresponding author, upon reasonable request.
References
Sharma A, Patnaik I, Kumar A, Gupta R. COVID-19 vaccines in patients with chronic liver disease. J Clin Exp Hepatol. 2021;11:720–726.
Albillos A, Lario M, Álvarez-Mon M. Cirrhosis-associated immune dysfunction: distinctive features and clinical relevance. J Hepatol. 2014;61:1385–1396.
Zermatten MG, Fraga M, Moradpour D, Bertaggia Calderara D, Aliotta A, Stirnimann G et al. Hemostatic alterations in patients with cirrhosis: from primary hemostasis to fibrinolysis. Hepatology. 2020;71:2135–2148.
Marjot T, Webb GJ, Barritt AS 4th, Moon AM, Stamataki Z, Wong VW et al. COVID-19 and liver disease: mechanistic and clinical perspectives. Nat Rev Gastroenterol Hepatol. 2021;18:348–364.
Marjot T, Moon AM, Cook JA, Abd-Elsalam S, Aloman C, Armstrong MJ et al. Outcomes following SARS-CoV-2 infection in patients with chronic liver disease: an international registry study. J Hepatol. 2021;74:567–577.
Iavarone M, D’Ambrosio R, Soria A, Triolo M, Pugliese N, Del Poggio P et al. High rates of 30-day mortality in patients with cirrhosis and COVID-19. J Hepatol. 2020;73:1063–1071.
Mehtani R, De A, Mishra S, Roy A, Gandotra A, Verma N et al. Natural history of non-severe COVID-19 in patients with liver disease. Hepatology. 2021;74:332A.
Fix OK, Blumberg EA, Chang KM, Chu J, Chung RT, Goacher EK et al. American association for the study of liver diseases expert panel consensus statement: vaccines to prevent coronavirus disease 2019 infection in patients with liver disease. Hepatology. 2021;74:1049–1064.
Alqahtani SA, Barry M, Memish Z, Hashim A, Alfares MA, Alghamdi SA et al. Use of COVID-19 vaccines in patients with liver disease and post-liver transplantation: Position statement of the Saudi association for the study of liver diseases and transplantation. Saudi J Gastroenterol. 2021;27:201–207.
Aggeletopoulou I, Davoulou P, Konstantakis C, Thomopoulos K, Triantos C. Response to hepatitis B vaccination in patients with liver cirrhosis. Rev Med Virol. 2017. https://doi.org/10.1002/rmv.1942.
McCashland TM, Preheim LC, Gentry MJ. Pneumococcal vaccine response in cirrhosis and liver transplantation. J Infect Dis. 2000;181:757–760. https://doi.org/10.1086/315245.
Theel ES, Harring J, Hilgart H, Granger D. Performance characteristics of four high-throughput immunoassays for detection of igg antibodies against SARS-CoV-2. J Clin Microbiol. 2020;58:e01243-e1320.
Luchsinger LL, Ransegnola BP, Jin DK, Muecksch F, Weisblum Y, Bao W et al. Serological assays estimate highly variable SARS-CoV-2 neutralizing antibody activity in recovered COVID-19 patients. J Clin Microbiol. 2020;58:e02005-e2020. https://doi.org/10.1128/JCM.02005-20.
Joyner MJ, Carter RE, Senefeld JW, Klassen SA, Mills JR, Johnson PW et al. Convalescent plasma antibody levels and the risk of death from Covid-19. N Engl J Med. 2021;384:1015–1027. https://doi.org/10.1056/NEJMoa2031893.
Folegatti PM, Ewer KJ, Aley PK, Angus B, Becker S, Belij-Rammerstorfer S et al. Safety and immunogenicity of the ChAdOx1 nCoV-19 vaccine against SARS-CoV-2: a preliminary report of a phase 1/2, single-blind, randomised controlled trial. Lancet. 2020;396:467–478.
Asano M, Okada H, Itoh Y, Hirata H, Ishikawa K, Yoshida E et al. Immunogenicity and safety of AZD1222 (ChAdOx1 nCoV-19) against SARS-CoV-2 in Japan: a double-blind, randomized controlled phase 1/2 trial. Int J Infect Dis. 2022;114:165–174. https://doi.org/10.1016/j.ijid.2021.10.030.
Ramasamy MN, Minassian AM, Ewer KJ, Flaxman AL, Folegatti PM, Owens DR et al. Safety and immunogenicity of ChAdOx1 nCoV-19 vaccine administered in a prime-boost regimen in young and old adults (COV002): a single-blind, randomised, controlled, phase 2/3 trial. Lancet. 2021;396:1979–1993.
Hoque A, Barshan AD, Chowdhury FUH, Fardous J, Hasan MJ, Khan MAS et al. Antibody response to ChAdOx1-nCoV-19 vaccine among recipients in Bangladesh: a prospective observational study. Infect Drug Resist. 2021;19:5491–5500.
Singh AK, Phatak SR, Singh R, Bhattacharjee K, Singh NK, Gupta A et al. Antibody response after first and second-dose of ChAdOx1-nCOV (Covishield™®) and BBV-152 (Covaxin™®) among health care workers in India: the final results of cross-sectional coronavirus vaccine-induced antibody titre (COVAT) study. Vaccine. 2021;39:6492–6509.
Voysey M, Clemens SAC, Madhi SA, Weckx LY, Folegatti PM, Aley PK et al. Safety and efficacy of the ChAdOx1 nCoV-19 vaccine (AZD1222) against SARS-CoV-2: an interim analysis of four randomised controlled trials in Brazil, South Africa, and the UK. Lancet. 2021;397:99–111.
Humphreys IR, Godkin AJ. The potential risks of delaying the second vaccine dose during the SARS-CoV-2 pandemic. QJM. 2021;114:163–165.
Hung IFN, Poland GA. Single-dose Oxford-AstraZeneca COVID-19 vaccine followed by a 12-week booster. Lancet. 2021;397:854–855.
Voysey M, Costa Clemens SA, Madhi SA, Weckx LY, Folegatti PM, Aley PK et al. Single-dose administration and the influence of the timing of the booster dose on immunogenicity and efficacy of ChAdOx1 nCoV-19 (AZD1222) vaccine: a pooled analysis of four randomised trials. Lancet. 2021;397:881–891.
Thuluvath PJ, Robarts P, Chauhan M. Analysis of antibody responses after COVID-19 vaccination in liver transplant recipients and those with chronic liver diseases. J Hepatol. 2021;75:1434–1439.
John BV, Deng Y, Schwartz KB, Taddei TH, Kaplan DE, Martin P, Chao HH, Dahman B. Postvaccination COVID-19 infection is associated with reduced mortality in patients with cirrhosis. Hepatology. 2022. https://doi.org/10.1002/hep.32337.
Willuweit K, Frey A, Passenberg M, Korth J, Saka N, Anastasiou OE et al. Patients with liver cirrhosis show high immunogenicity upon COVID-19 vaccination but develop premature deterioration of antibody titers. Vaccines (Basel) 2022;10:377. https://doi.org/10.3390/vaccines10030377.
Ruether DF, Schaub GM, Duengelhoef PM, Haag F, Brehm TT, Fathi A et al. SARS-CoV2-specific humoral and t-cell immune response after second vaccination in liver cirrhosis and transplant patients. Clin Gastroenterol Hepatol. 2022;20:162-172.e9. https://doi.org/10.1016/j.cgh.2021.09.003.
Bakasis AD, Bitzogli K, Mouziouras D, Pouliakis A, Roumpoutsou M, Goules AV et al. Antibody responses after SARS-CoV-2 vaccination in patients with liver diseases. Viruses 2022;14:207. https://doi.org/10.3390/v14020207.
Ai J, Wang J, Liu D, Xiang H, Guo Y, Lv J, et al. Safety and Immunogenicity of SARS-CoV-2 Vaccines in Patients With Chronic Liver Diseases (CHESS-NMCID 2101): A Multicenter Study. Clin Gastroenterol Hepatol. 2021:S1542–3565(21)01346-X. https://doi.org/10.1016/j.cgh.2021.12.022.
Wang J, Zhang Q, Ai J, Liu D, Liu C, Xiang H, et al. Safety and immunogenicity of SARS-CoV-2 vaccines in Chinese patients with cirrhosis: a prospective multicenter study. Hepatol Int. 2022. doi: https://doi.org/10.1007/s12072-022-10332-9.
Poland GA, Ovsyannikova IG, Kennedy RB. SARS-CoV-2 immunity: review and applications to phase 3 vaccine candidates. Lancet. 2020;396:1595–1606.
Okba NMA, Müller MA, Li W, Wang C, GeurtsvanKessel CH, Corman VM et al. Severe acute respiratory syndrome coronavirus 2-specific antibody responses in coronavirus disease patients. Emerg Infect Dis. 2020;26:1478–1488.
Khoury DS, Cromer D, Reynaldi A, Schlub TE, Wheatley AK, Juno JA et al. Neutralizing antibody levels are highly predictive of immune protection from symptomatic SARS-CoV-2 infection. Nat Med. 2021;27:1205–1211.
Khoury DS, Cromer D, Reynaldi A, Sclub TE, Wheatley AK, Juno JA, et al. What level of neutralising antibody protects from COVID-19? medRxiv preprint doi: https://doi.org/10.1101/2021.03.09.21252641.
Mlcochova P, Kemp SA, Dhar MS, Papa G, Meng B, Ferreira IATM et al. SARS-CoV-2 B.1.617.2 Delta variant replication and immune evasion. Nature. 2021;599(7883):114–119. https://doi.org/10.1038/s41586-021-03944-y.
Ghosh S, Shankar S, Chatterjee K, Chatterjee K, Yadav AK, Pandya K et al. COVISHIELD (AZD1222) VaccINe effectiveness among healthcare and frontline Workers of INdian Armed Forces: interim results of VIN-WIN cohort study. Med J Armed Forces India. 2021;77:S264–S270.
Rana K, Mohindra R, Pinnaka L. Vaccine breakthrough infections with SARS-CoV-2 variants. N Engl J Med. 2021;385:e7.
John BV, Deng Y, Scheinberg A, Mahmud N, Taddei TH, Kaplan D et al. Association of BNT162b2 mRNA and mRNA-1273 vaccines with COVID-19 infection and hospitalization among patients with cirrhosis. JAMA Intern Med. 2021;181:1306–1314.
Marjot T, Webb GJ, Barritt AS, Ginès P, Lohse AW, Moon AM et al. SARS-CoV-2 vaccination in patients with liver disease: responding to the next big question. Lancet Gastroenterol Hepatol. 2021;6:156–158.
Funding
Partially funded by Society for the Study of Liver Diseases (SSLD).
Author information
Authors and Affiliations
Contributions
AS contributed to design of the study protocol, patient enrollment, data collection, and analysis. ArD contributed to conceptualization and design of the study, patient recruitment, data analysis and interpretation, and manuscript writing. MS contributed to data collection and serologic testing. RK and TK contributed to data collection and telephonic interviews. SR,NV, ST, and AD contributed to patient enrollment and data collection. MPK contributed to concept and design, patient enrollment, and data collection. VS contributed to conceptualization and design of the study, patient recruitment, data analysis and interpretation, manuscript writing, and study coordinator.
Corresponding author
Ethics declarations
Competing interests
All authors declare no competing interests.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Institutional Ethics Committee of Postgraduate Institute of Medical Education and Research, Chandigarh (Date 11.8.21; No. 001170).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
An editorial commenting on this article is available at https://doi.org/10.1007/s10620-022-07644-z
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Singh, A., De, A., Singh, M.P. et al. Antibody Response and Safety of ChAdOx1-nCOV (Covishield) in Patients with Cirrhosis: A Cross-Sectional, Observational Study. Dig Dis Sci 68, 676–684 (2023). https://doi.org/10.1007/s10620-022-07641-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-022-07641-2