Abstract
Background
There are limited real-world data characterizing perianal fistulae in patients with Crohn’s disease (CD).
Aim
To describe characteristics of patients with CD with and without perianal fistulae.
Methods
In this cross-sectional study, characteristics, treatment history, and health outcomes of patients with CD enrolled in the CorEvitas IBD Registry were described according to perianal fistula status (current/previous or none).
Results
Eight hundred and seventy-eight patients were included. Compared with patients with no perianal fistulae (n = 723), patients with current/previous perianal fistulae (n = 155) had longer disease duration since CD diagnosis (mean 16.5 vs 12.3 years; difference 4.3 years; 95% CI, 2.0, 6.6) and fewer had Harvey–Bradshaw Index scores indicative of remission (0–4, 56.8% vs 69.6%; difference − 12.9%; 95% CI, − 21.6, − 4.2). More patients with current/previous fistulae reported a history of IBD-related emergency room visits (67.7% vs 56.1%; difference 11.6%; 95% CI, 3.4, 19.8), hospitalizations (76.1% vs 58.4%; difference 17.7%; 95% CI, 10.1, 25.4), and surgeries (59.4% vs 27.7%; difference 31.7%; 95% CI, 23.3, 40.1), and a history of treatment with tumor necrosis factor inhibitors (81.3% vs 60.7%; difference 20.6%; 95% CI, 13.5, 27.7), immunosuppressants (51.6% vs 31.2%; difference 20.4%; 95% CI, 11.9, 29.0), and antibiotics (50.3% vs 23.7%; difference 26.6%; 95% CI, 18.2, 35.1) than patients without perianal fistulae.
Conclusions
Patients with CD with current/previous perianal fistulae have more symptomatic experiences of disease, higher medication use, hospitalization rates, and emergency room visits than patients without perianal fistulae. Interventions to prevent/reduce risk of developing fistulae may help improve outcomes in CD.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Crohn’s disease (CD) is a chronic condition characterized by transmural inflammation that often affects the terminal ileum, but also has the potential to occur in any part of the gastrointestinal tract in a non-contiguous pattern [1]. Addressing common symptoms caused by mucosal inflammation, including diarrhea, abdominal pain, and gastrointestinal bleeding, is the immediate goal of CD management, while prevention of related complications is an equal priority [2]. If insufficiently controlled, chronic inflammation can lead to long-term complications, such as fibrotic strictures, fistulae (although in some cases these may be present at the onset of CD and in up to 10% of patients may be the sole manifestation of the disease), intra-abdominal abscesses, and intestinal neoplasia [1, 3, 4]. For this reason, early and effective control of inflammation is essential.
Perianal fistulae can have a major impact on quality of life for patients with CD. Perianal fistulae are painful; they may also cause embarrassment, may impair physical, sexual, and psychological function, and may interfere with the patient’s ability to work [5]. In addition, perianal fistulae are associated with increased healthcare resource use and costs, and are a risk factor for future complications [6,7,8].
Perianal fistulae are common in patients with CD, and, as previously mentioned, in a small percentage of patients they can be the only manifestation of the disease and may precede intestinal manifestations of CD by several years [4]. A population-based study in Olmsted County, Minnesota, USA, found that perianal fistulae manifested before or at the time of diagnosis in 45% of patients with CD [9]. Similar results were reported in other population-based studies in Canterbury, New Zealand (28%), and Stockholm County, Sweden (23%) [10, 11]. More recently, a study in the Netherlands that involved 232 individuals with perianal fistulae reported that 28% of patients developed fistulae within 6 months after the onset of CD and 79% within 10 years after diagnosis of CD (median 7 years) [12].
The management and prevention of perianal fistulae can be challenging. Medical treatment includes tumor necrosis factor inhibitors (TNFi) and non-TNFi biologics [13]. However, even with optimal management, the best healing rates for perianal fistulae are approximately 50% [13, 14]. As a result, surgery is often required, which may include seton placement or, in some cases, intestinal diversion with an ostomy [13, 15, 16]. Some studies have shown additional benefit from combined placement of a seton and anti-TNF therapy, although insight into which patients will benefit from medical or surgical treatment alone, or in combination, is poor [17].
Currently, understanding of perianal fistulae is limited by an absence of real-world patient data. More information on how clinical outcome and disease course are related to fistulae could inform prevention strategies and treatment decisions, and may contribute to clinical studies for new therapies. The objective of this cross-sectional study from the inflammatory bowel disease (IBD) Registry is to describe the characteristics of patients with CD with and without perianal fistulae, including their sociodemographic characteristics, disease characteristics, comorbidities, treatments, and healthcare resource use.
Methods
Study Overview
Patients for this study were selected from the CorEvitas (formerly Corrona) IBD Registry, which was launched in May 2017, and is a prospective, non-interventional, US research-based registry that includes patients with IBD under the care of a certified gastroenterologist. As of December 31, 2019, the registry included 123 gastroenterologists practicing at 57 private and academic clinical sites in 20 states in the USA. In total, 85% of sites were private and 15% were academic.
Patients
Enrolled patients were required to be at least 18 years of age, diagnosed with CD or ulcerative colitis (UC) by a gastroenterologist and to have provided written consent for participation in the CorEvitas IBD Registry. Patients were excluded if they were participating or planning to participate in an interventional phase I–IV clinical trial with a non-marketed or marketed investigational drug. Enrollment and longitudinal follow-up data were collected by questionnaires from patients and their treating gastroenterologist during routine outpatient clinical encounters.
Questionnaires included questions on patient demographics, medical history, clinical characteristics, comorbidities, treatment history for IBD, healthcare encounters, and targeted safety outcomes. Blood collection, endoscopy, and other diagnostic tests were not required from participants; however, laboratory and imaging results performed as part of standard of care are reported when available.
Patients included in this analysis were those with a physician-confirmed diagnosis of CD who were enrolled in the IBD registry between May 3, 2017 and March 3, 2020. Patients with a diagnosis of UC, indeterminate colitis, and those whose diagnosis had been changed from CD at the initial visit to an alternative diagnosis at subsequent visits, were excluded from the analysis. Eligible patients were stratified into two mutually exclusive groups according to physician-reported status of perianal fistulae at the time of enrollment: with current or previous perianal fistulae (PF), or no current or previous perianal fistulae (NF).
Assessments
Variables assessed at the time of patient enrollment in the registry included demographic, health, and socioeconomic characteristics; clinical characteristics (comorbidities, extraintestinal manifestations, disease duration and location, Harvey–Bradshaw Index [HBI]; full description of HBI in the Supplementary Data Content 1); treatments received for IBD (medication and surgery); and healthcare resource utilization before enrollment (emergency room visits, hospitalization). HBI scores were collected at time of enrollment into the registry at routine outpatient clinical visits and are independent of disease status.
Statistical Analyses
Categorical variables were summarized using frequency counts and percentages; continuous variables were summarized by mean and standard deviation, and 95% confidence intervals (CIs) were reported for estimates of the unadjusted mean difference or unadjusted proportional mean difference between the PF and NF group for each variable. All variables were based on those collected at the enrollment visit; R version 4.0.4 (The R Foundation for Statistical Computing, Vienna, Austria) was used for analysis.
This was a descriptive analysis aiming to generate future research, and consequently, no formal statistical hypothesis testing was undertaken.
Results
Demographic, Health, and Socioeconomic Characteristics
In total, 878 patients with CD were included in this analysis, 155 (17.7%) in the PF group and 723 (82.3%) in the NF group (Table 1). The PF group was comprised largely of patients with a previous PF (n = 118), rather than current PF (n = 37).
Overall, 42.2% identified as male, 87.1% were white, and the mean duration of CD was 13.0 years (Tables 1 and 2). Although the majority of all patients identified as female, most patients in the PF group identified as male. The two groups were generally comparable in terms of body mass index, smoking status, and alcohol consumption; however, some differences were observed. The PF group was slightly younger than the NF group (mean 44.4 years vs 47.2 years; difference − 2.8 years; 95% CI, − 5.4, − 0.2) and had a higher proportion of men (55.5% vs 39.3%; difference 16.1%; 95% CI, 7.5, 24.7; Table 1). In addition, a larger proportion of patients in the PF group had private insurance (83.2% vs 71.9%; difference 11.3%; 95% CI, 4.6, 18.0) and full-time employment (64.5% vs 53.0%; difference 11.6%; 95% CI, 3.2, 19.9; Table 1).
Clinical Characteristics and Healthcare Resource Utilization
Patients in the PF group were younger at the age of CD onset compared with patients in the NF group (mean 27.9 years vs 34.9 years; difference − 7.0 years; 95% CI, − 9.6, − 4.4), and patients in the former group had longer disease duration since the onset of CD symptoms (mean 18.3 years vs 14.1 years; difference 4.2 years; 95% CI, 1.9, 6.6) or since diagnosis of CD (mean 16.5 years vs 12.3 years; difference 4.3 years; 95% CI, 2.0, 6.6; Table 2).
At enrollment, mean HBI scores were 4.4 for patients in the PF group and 3.8 for patients in the NF group (difference 0.6; 95% CI, 0.0, 1.3); furthermore, a lower proportion of patients in the PF group had HBI scores indicative of remission (0–4, 56.8% vs 69.6%; difference − 12.9%; 95% CI, − 21.6, − 4.2) compared with patients in the NF group (Table 3).
With respect to disease behavior, ileal disease was reported in 31% of patients in the PF group and 38.0% of patients in the NF group (difference − 7.1%; 95% CI, − 15.2, 1.0; Table 2).
Comorbidities and Infections
Patients in the PF or NF groups generally had similar histories of cardiovascular, autoimmune, respiratory, digestive/hepatic, and neurologic disease, as well as diabetes mellitus, depression, anxiety, and infections (Table 4). With respect to the extraintestinal manifestations of CD, eye involvement (5.8% vs 1.9%; difference 3.9; 95% CI, 0.1, 7.7) was more frequently reported by patients in the PF group than in the NF group.
Healthcare Resource Utilization
A higher proportion of patients in the PF group had a lifetime history of IBD-related hospitalizations (76.1% vs 58.4%; difference 17.7%; 95% CI, 10.1, 25.4) and emergency room visits (67.7% vs 56.1%; difference 11.6; 95% CI, 3.4, 19.8; Table 5).
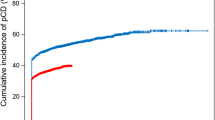
Medical and Surgical Interventions
A higher proportion of patients in the PF group than in the NF group had received prior treatment with biologics/Janus kinase inhibitors (JAKi) (87.7% vs 69.3%; difference 18.4%; 95% CI, 12.3, 24.7) in general, and with TNFi (81.3% vs 60.7%; difference 20.6%; 95% CI, 13.5, 27.7), non-TNFi biologics (34.2% vs 24.5%; difference 9.7%; 95% CI, 1.6, 17.8), immunosuppressants (51.6% vs 31.2%; difference 20.4%; 95% CI, 11.9, 29.0), and antibiotics (50.3% vs 23.7%; difference 26.6%; 95% CI, 18.2, 35.1; Fig. 1). In contrast, fewer patients in the PF group than the NF group had received corticosteroids during the previous 3 months (9.0% vs 15.6%; difference − 6.6%; 95% CI, − 11.8, − 1.4; Fig. 1).
History of medical management by perianal fistula status. Percentages were calculated based on the number of patients with a valid entry for the respective variables, which can differ from the total number of patients in each group due to missing values. aIncluding tapering doses. bEvery day or most days. cOn a few days only. 5ASA, 5-aminosalicylic acid; CI confidence interval; CS corticosteroid; JAKi Janus kinase inhibitor; NSAID non-steroidal anti-inflammatory drug; NF no previous or current perianal fistulae; PF current or previous perianal fistulae; TNFi tumor necrosis factor inhibitor
The pattern of ongoing (concomitant) therapy was generally similar; a higher proportion of patients in the PF group than in the NF group were receiving treatment with biologics/JAKi (76.8% vs 61.3%; difference 15.5%; 95% CI, 8.0, 23.0) overall, and with TNFi (48.4% vs 38.0%; difference 10.4%; 95% CI, 1.7, 19.0), and immunosuppressants (22.6% vs 14.7%; difference 7.9%; 95% CI, 0.9, 15.0) in particular (Fig. 1). In contrast, fewer patients in the PF group than the NF group were receiving concomitant treatment with 5-aminosalicylic acid-containing products (11.0% vs 21.3%; difference − 10.3%; 95% CI, − 16.1, − 4.6; Fig. 1). Despite marked differences in the types of therapy the two groups were receiving, the durations of current therapy were similar (2.2 years vs 2.4 years; difference − 0.2 years; 95% CI, − 0.8, 0.5; Table 2).
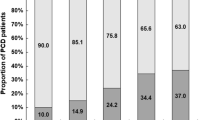
More patients in the PF group than in the NF group had a history of surgery for IBD (59.4% vs 27.7%; difference 31.7%; 95% CI, 23.3, 40.1), including resection (38.7% vs 24.8%; difference 13.9%; 95% CI, 5.7, 22.2), ostomy (17.4% vs 4.6%; difference 12.8%; 95% CI, 6.7, 19.0), and other surgery (27.7% vs 4.0%; difference 23.7%; 95% CI, 16.5, 30.9; Fig. 2). Moreover, a higher proportion of patients in the PF group than in the NF group had undergone more than one type of surgery for IBD (20.0% vs 4.4%; difference 15.6%; 95% CI, 9.1, 22.0; Fig. 2).
History of surgical management by perianal fistula status. Percentages were calculated based on the number of patients with a valid entry for the respective variables, which can differ from the total number of patients in each group due to missing values. CI confidence interval; IBD inflammatory bowel disease; NF no previous or current perianal fistulae; PF current or previous perianal fistulae
Discussion
This analysis of patients with CD in a real-world setting has identified several differences in the demographics, medication use, and symptomatic experience between patients with and without perianal fistulae. Patients with PF were more commonly male, younger, and as expected, had a longer duration of CD than patients with NF and more extensive exposure to biologic therapies and JAKi. In addition, patients with PF had a higher HBI, as well as more frequent utilization of emergency and hospital medical care, and need for IBD-related surgeries, reflecting higher disease burden. In total, this analysis demonstrates a considerable symptomatic and health outcome impact of perianal fistulae in patients with CD within real-world clinical practice settings.
Perianal fistulae have a clear association with worse symptoms and health outcomes in patients with CD. In this study, patients with PF had higher mean HBI scores, a higher proportion with moderate-to-severe disease activities as indicated by HBI score ≥ 8, and a lower proportion in remission as indicated by HBI score ≤ 4 at the time of being measured. However, despite the importance of perianal fistulae, the ability to assess this complication of CD is limited. Conventional disease assessment indices such as the Crohn’s Disease Activity Index or HBI capture general symptomatic burden and, in the case of the HBI, indicates the presence or absence of perianal disease, but lacks specificity for the unique impact on quality of life that perianal fistulae impose. As therapeutic pathways aim for improved personalization of treatment, both clinical trials and real-world practice would benefit from improved disease assessment tools that capture the particular symptoms and impact associated with perianal disease. Efforts are underway to develop new and specific patient-reported outcome measurement instruments that capture the burden of symptoms, and the impact of treatment on the well-being of patients with PF [5]. The Crohn’s Anal Fistula Quality of Life scale was developed by using data from 211 patients with the goal of capturing more granular and consistent fistula data to better tailor disease treatment and management strategies. The 28-item questionnaire exhibited excellent performance and has very good correlation with psychometric questionnaires (i.e., the UK Inflammatory Bowel Disease Questionnaire and Hospital Anxiety and Depression Scale). The data presented in our study clearly demonstrate the real-world impact of perianal fistulae; incorporation of improved knowledge of the experience and symptoms of perianal fistulae into care pathways for CD will be important in the future.
Treatment of perianal fistulizing disease remains a difficult challenge in the management of CD. Within our cohort, more patients with PF had received biologic (87.7% vs 69.3%) and immunosuppressant (51.6% vs 31.2%) therapies than those with NF. This high proportion of biologic use is not surprising, and although we did not investigate prescribing behavior, the finding suggests that practitioners may be prescribing biologics for patients with PF and that patients are readily using such drugs in greater proportions than in the past decade. Moreover, our understanding of the value of proactive versus reactive initiation of biologic therapy or combination therapy is incomplete. Combined medical and surgical therapy has been shown to yield the best clinical outcome (permanent fistula closure) in patients with perianal fistulae [14]. Yet, the combination of seton placement and biologic therapy has only about a 60–75% success rate in this regard [18, 19]. More work is needed to better understand the personalization of treatment selection, the optimization of drug therapy using serum concentrations and biomarkers, as well as the use of new treatments such as stem cell therapy and local injections of biologics to achieve the best outcomes for these patients [19, 20].
This study has several limitations that should be noted. Data from the CorEvitas IBD Registry are US based; therefore, results may not be applicable to populations residing outside the USA. In addition, the small number of participating specialist gastroenterologists throughout 20 states in the USA that are included within the registry places further geographical limitations within the USA. As the registry is not based on an inception cohort, misclassification due to recall bias is a potential limitation. There is also potential bias because patients enrolled in interventional trials were excluded from participating in the present study, although this is a common exclusion criterion for registry studies. Finally, this was a cross-sectional study with a descriptive analysis, so it is not possible to derive causal relationships. These limitations place some restrictions on the generalizability of the results. However, despite these limitations, the present study provides recent data further confirming the burden of perianal fistulizing CD in the real world.
Conclusion
In conclusion, the results of this cross-sectional analysis of data from the IBD Registry show that patients with PF have more severe disease activity, as indicated by more intensive pharmaceutical treatment histories marked by more frequent use of biologics, more extensive surgical treatment histories, and higher rates of hospitalization and emergency room visits compared with patients with NF. Further research is warranted to determine which interventions or therapies, if any, can prevent or reduce the incidence of perianal fistulae in patients with CD, to help patients avoid more intensive therapies and improve their health outcomes.
References
Chang JT. Pathophysiology of inflammatory bowel diseases. N Engl J Med. 2020;383:2652–2664.
Knowles SR, Keefer L, Wilding H et al. Quality of life in inflammatory bowel disease: A systematic review and meta-analyses-part II. Inflamm Bowel Dis. 2018;24:966–976.
Cushing K, Higgins PDR. Management of Crohn disease: A review. J Am Med Assoc. 2021;325:69–80.
Rubbino F, Greco L, di Cristofaro A et al. Journey through Crohn’s disease complication: From fistula formation to future therapies. J Clin Med. 2021;10:5548.
Adegbola SO, Dibley L, Sahnan K et al. Burden of disease and adaptation to life in patients with Crohn’s perianal fistula: A qualitative exploration. Health Qual Life Outcomes. 2020;18:370.
Tarrant KM, Barclay ML, Frampton CMA, Gearry RB. Perianal disease predicts changes in Crohn’s disease phenotype—results of a population-based study of inflammatory bowel disease phenotype. Am J Gastroenterol. 2008;103:3082–3093.
Thia KT, Sandborn WJ, Harmsen WS, Zinsmeister AR, Loftus EV Jr. Risk factors associated with progression to intestinal complications of Crohn’s disease in a population-based cohort. Gastroenterology. 2010;139:1147–1155.
Beaugerie L, Seksik P, Nion-Larmurier I, Gendre JP, Cosnes J. Predictors of Crohn’s disease. Gastroenterology. 2006;130:650–656.
Schwartz DA, Loftus EV Jr, Tremaine WJ et al. The natural history of fistulizing Crohn’s disease in Olmsted County Minnesota. Gastroenterology. 2002;122:875–880.
Eglinton TW, Barclay ML, Gearry RB, Frizelle FA. The spectrum of perianal Crohn’s disease in a population-based cohort. Dis Colon Rectum. 2012;55:773–777.
Hellers G, Bergstrand O, Ewerth S, Holmström B. Occurrence and outcome after primary treatment of anal fistulae in Crohn’s disease. Gut. 1980;21:525–527.
Molendijk I, Nuij VJ, van der Meulen-de Jong AE, van der Woude CJ. Disappointing durable remission rates in complex Crohn’s disease fistula. Inflamm Bowel Dis. 2014;20:2022–2028.
Kotze PG, Shen B, Lightner A et al. Modern management of perianal fistulas in Crohn’s disease: Future directions. Gut. 2018;67:1181–1194.
Yassin NA, Askari A, Warusavitarne J et al. Systematic review: The combined surgical and medical treatment of fistulising perianal Crohn’s disease. Aliment Pharmacol Ther. 2014;40:741–749.
Gecse KB, Bemelman W, Kamm MA et al. A global consensus on the classification, diagnosis and multidisciplinary treatment of perianal fistulising Crohn’s disease. Gut. 2014;63:1381–1392.
Panés J, Rimola J. Perianal fistulizing Crohn’s disease: Pathogenesis, diagnosis and therapy. Nat Rev Gastroenterol Hepatol. 2017;14:652–664.
de Groof EJ, Sahami S, Lucas C et al. Treatment of perianal fistula in Crohn’s disease: A systematic review and meta-analysis comparing seton drainage and anti-tumour necrosis factor treatment. Colorectal Dis. 2016;18:667–675.
Gaertner WB, Decanini A, Mellgren A et al. Does infliximab infusion impact results of operative treatment for Crohn’s perianal fistulas? Dis Colon Rectum. 2007;50:1754–1760.
Alessandroni L, Kohn A, Cosintino R et al. Local injection of infliximab in severe fistulating perianal Crohn’s disease: An open uncontrolled study. Tech Coloproctol. 2011;15:407–412.
Ma C, Fedorak RN, Kaplan GG et al. Clinical, endoscopic and radiographic outcomes with ustekinumab in medically-refractory Crohn’s disease: Real world experience from a multicentre cohort. Aliment Pharmacol Ther. 2017;45:1232–1243.
Acknowledgments
We would like to thank Denise Bennett for her contributions to the study. Blair Jarvis, MSc, and Tina Borg, PhD, of OPEN Health Communications provided medical writing support, editorial support, and formatting assistance, which was contracted and funded by Boehringer Ingelheim.
Funding
This study was sponsored by CorEvitas, LLC, and the analysis was funded by Boehringer Ingelheim. Access to study data was limited to CorEvitas, and CorEvitas statisticians completed all the analysis; all authors contributed to the interpretation of the results. The CorEvitas IBD Registry has been supported through contracted subscriptions in the last two years by AbbVie, Amgen, Boehringer Ingelheim, Bristol-Myers Squibb, Celgene, Chugai, Eli Lilly and Company, Genentech, Gilead, GlaxoSmithKline, Janssen, Novartis, Ortho Dermatologics, Pfizer, Inc., Regeneron, Sanofi, Sun, and UCB.
Author information
Authors and Affiliations
Contributions
YF and WCV were involved in the conception and trial design. PCM and MMC were involved in the acquisition of data. All authors contributed to the analysis and/or interpretation of the data, and drafting, critically revising, and commenting on previous versions and the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
This study design and conduct were the result of a collaborative effort between CorEvitas, LLC, and Boehringer Ingelheim. YF, SDA, and WCV are employed by Boehringer Ingelheim. PCM, JCJ, and MMC are employed by CorEvitas, LLC. RWS has received consultancy fees for AbbVie, Janssen, Merck, Takeda, Eli Lilly, Gilead, Exact Sciences, and CorEvitas, LLC, and has received investigator-initiated research support from AbbVie.
Data availability
The CorEvitas (formerly Corrona) LLC dataset is based on a large North American multicenter study adhering to a number of institutional review boards, with complex logistics. Patients did not provide consent to raw data sharing during the data collection for this purpose, and the CorEvitas data-sharing policies do not permit raw data sharing for this purpose. An aggregated limited dataset from the current approved analyses is available to qualified investigators with an approved protocol. Data requests may be sent to CorEvitas, LLC, represented by Dr. Jeffrey D. Greenberg MD, MPH, NYU School of Medicine, New York, NY, e-mail jgreenberg@corevitas.com.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Fan, Y., Delgado-Aros, S., Valdecantos, W.C. et al. Characteristics of Patients with Crohn’s Disease With or Without Perianal Fistulae in the CorEvitas Inflammatory Bowel Disease Registry. Dig Dis Sci 68, 214–222 (2023). https://doi.org/10.1007/s10620-022-07491-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-022-07491-y