Abstract
Introduction
Although coexistence of alcohol-related liver disease (ALD) and pancreatitis (ALP) is seen in clinical practice, a clear understanding of the overlap between these diseases is lacking. Moreover, the relative risks for certain population groups have not been studied. We determined the prevalence and coexistence of ALD and ALP in patients with an alcohol use disorder using retrospective analysis of a large patient cohort from Western Pennsylvania. We specifically emphasized the analysis of underrepresented populations, including women and blacks.
Methods
We identified all unique patients who received care in UPMC health system during 2006–2017 with at least one International Classification of Diseases versions 9 and/or 10 codes for alcohol misuse, ALD and pancreatitis. We noted their sex, race and age of first diagnosis and duration of contact.
Results
Among 89,774 patients that fit our criteria, the prevalence of ALD, ALP and coexistent ALD and ALP in patients with alcohol misuse was 11.7%, 7.4% and 2.5%, respectively. Prevalence of ALP in ALD was 16.4%, and ALD in ALP was 33.1%. Prevalence of ALP in ALD was slightly more prevalent in women (18.6% vs. 15.6%, p < 0.001). Prevalence of ALP in ALD was 2–4 folds greater in blacks than other races.
Discussion
A sizeable fraction of patients with ALD or ALP has coexistent disease. This is the first study to identify that blacks are at a higher risk for ALP in the presence of ALD. Future studies should define the clinical impact of coexistent disease on clinical presentation and short- and long-term outcomes.



Similar content being viewed by others
Abbreviations
- ALD:
-
Alcohol-related liver disease
- AAH:
-
Acute alcohol-related hepatitis
- ALC:
-
Alcohol-related liver cirrhosis
- AFLD:
-
Alcohol-related fatty liver disease
- AL:
-
Alcohol-related pancreatitis
- AAP:
-
Acute alcohol-related pancreatitis
- ACP:
-
Alcohol-related chronic pancreatitis
- AUD:
-
Alcohol use disorder
- DALYs:
-
Disease-adjusted life years
- ICD:
-
International Classification of Diseases
- UPMC:
-
University of Pittsburgh Medical Center
References
Carvalho AF, Heilig M, Perez A, Probst C, Rehm J. Alcohol use disorders. Lancet. 2019;394:781–792.
World Health Organization. Global Status Report on Alcohol and Health. Geneva, Switzerland: 2018. Available at: www.who.int/publications/i/item/9789241565639. Accessed January 20, 2021.
Murray CJ, Atkinson C, Bhalla K, Birbeck G, Burstein R, Chou D et al. The state of US health, 1990–2010: burden of diseases, injuries, and risk factors. JAMA. 2013;310:591–608.
Rehm J, Taylor B, Mohapatra S, Irving H, Baliunas D, Patra J et al. Alcohol as a risk factor for liver cirrhosis: a systematic review and meta-analysis. Drug Alcohol Rev. 2010;29:437–445.
Samokhvalov AV, Rehm J, Roerecke M. Alcohol consumption as a risk factor for acute and chronic pancreatitis: a systematic review and a series of meta-analyses. EBioMedicine. 2015;2:1996–2002.
Bataller R, Arteel GE, Moreno C, Shah V. Alcohol-related liver disease: time for action. J Hepatol. 2019;70:221–222.
Easler JJ, de-Madaria E, Nawaz H, Moya-Hoyo N, Koutroumpakis E, Rey-Riveiro M, et al. Patients with sentinel acute pancreatitis of alcoholic etiology are at risk for organ failure and pancreatic necrosis: a dual-center experience. Pancreas 2016;45:997–1002.
Yadav D, Timmons L, Benson JT, Dierkhising RA, Chari ST. Incidence, prevalence, and survival of chronic pancreatitis: a population-based study. Am J Gastroenterol. 2011;106:2192–2199.
Nojgaard C, Bendtsen F, Becker U, Andersen JR, Holst C, Matzen P. Danish patients with chronic pancreatitis have a four-fold higher mortality rate than the Danish population. Clin Gastroenterol Hepatol. 2010;8:384–390.
Whitcomb DC, LaRusch J, Krasinskas AM, Klei L, Smith JP, Brand RE et al. Common genetic variants in the CLDN2 and PRSS1-PRSS2 loci alter risk for alcohol-related and sporadic pancreatitis. Nat Genet. 2012;44:1349–1354.
Buch S, Stickel F, Trepo E, Way M, Herrmann A, Nischalke HD et al. A genome-wide association study confirms PNPLA3 and identifies TM6SF2 and MBOAT7 as risk loci for alcohol-related cirrhosis. Nat Genet. 2015;47:1443–1448.
Wilcox CM, Sandhu BS, Singh V, Gelrud A, Abberbock JN, Sherman S et al. Racial differences in the clinical profile, causes, and outcome of chronic pancreatitis. Am J Gastroenterol. 2016;111:1488–1496.
Dam MK, Flensborg-Madsen T, Eliasen M, Becker U, Tolstrup JS. Smoking and risk of liver cirrhosis: a population-based cohort study. Scand J Gastroenterol. 2013;48:585–591.
Rusyn I, Bataller R. Alcohol and toxicity. J Hepatol. 2013;59:387–388.
Singhvi A, Abromitis R, Althouse AD, Bataller R, Arteel GE, Yadav D. Coexistence of alcohol-related pancreatitis and alcohol-related liver disease: A systematic review and meta-analysis. Pancreatol. 2020;6:1069.
Yadav D, O’Connell M, Papachristou GI. Natural history following the first attack of acute pancreatitis. Am J Gastroenterol. 2012;107:1096–1103.
Seitz HK, Bataller R, Cortez-Pinto H, Gao B, Gual A, Lackner C et al. Alcoholic liver disease. Nat Rev Dis Dis Primers. 2018;4:16.
Pace A, de Weerth A, Berna M, Hillbricht K, Tsokos M, Bläker M et al. Pancreas and liver injury are associated in individuals with increased alcohol consumption. Clin Gastroenterol Hepatol. 2009;7:1241–1246.
Bellentani S, Saccoccio G, Costa G, Tiribelli C, Manenti F, Sodde M et al. Drinking habits as cofactors of risk for alcohol induced liver damage. The Dionysos Study Group. . Gut. 1997;41:845–850.
Yadav D, Eigenbrodt ML, Briggs MJ, Williams DK, Wiseman EJ. Pancreatitis: prevalence and risk factors among male veterans in a detoxification program. Pancreas. 2007;34:390–398.
Aoufi Rabih S, García Agudo R, Legaz Huidobro ML, Ynfante Ferrús M, González Carro P, Pérez Roldán F et al. Exocrine pancreatic insufficiency and chronic pancreatitis in chronic alcoholic liver disease: coincidence or shared toxicity? Pancreas. 2014;43:730–734.
Testino G, Leone S, Fagoonee S. Alcoholic liver disease and vitamin D deficiency. Minerva Med. 2018;109:341–343.
Takase M, Suda K, Suzuki F, Nakamura T, Futagawa S. A histopathologic study of localized portal hypertension as a consequence of chronic pancreatitis. Arch Pathol Lab Med. 1997;121:612–614.
Li H, Yang Z, Tian F. Clinical characteristics and risk factors for sinistral portal hypertension associated with moderate and severe acute pancreatitis: a seven-year single-center retrospective study. Med Sci Mon. 2019;25:5969–5976.
Rasineni K, Srinivasan MP, Balamurugan AN, Kaphalia BS, Wang S, Ding WX et al. Recent advances in understanding the complexity of alcohol-induced pancreatic dysfunction and pancreatitis development. Biomolecules 2020;10:669.
Nielsen JK, Olafsson S, Bergmann OM, Runarsdottir V, Hansdottir I, Sigurdardottir R et al. Lifetime drinking history in patients with alcoholic liver disease and patients with alcohol use disorder without liver disease. Scand J Gastroenterol. 2017;52:762–767.
Jeon CY, Whitcomb DC, Slivka A, Brand RE, Gelrud A, Tang G et al. Lifetime drinking history of persons with chronic pancreatitis. Alcohol Alcohol. 2019;54:615–624.
Yang AL, Vadhavkar S, Singh G, Omary MB. Epidemiology of alcohol-related liver and pancreatic disease in the United States. Arch Intern Med. 2008;168:649–656.
Anstee QM, Seth D, Day CP. Genetic factors that affect risk of alcoholic and nonalcoholic fatty liver disease. Gastroenterol. 2016;150:e7.
Gustot T, Jalan R. Acute-on-chronic liver failure in patients with alcohol-related liver disease. J Hepatol. 2019;70:319–327.
Acknowledgment
The authors thank the Enhancing MEntoring to Improve Research in GastroEnterology (EMERGE) Program of the Division of Gastroenterology, Hepatology and Nutrition, University of Pittsburgh, and the Collaborative Alliance of Pancreas Education and Research (CAPER) Scholars Program for supporting this project.
Funding
DY (UO1 DK108306, DoD PR 182623); AAD (R01 CA19710 (NIH), W81XWH-15-1-0663 (DoD), R01 CA235730-01 (NIH), U01 GM132133 (NIH), R61 HL144669-01 (NIH), R21 TR003094-01 (NIH), R34 HL132031—01A1 (NIH); GEA (R01AA021978, R01AA028436 and P30DK120531); RB (U01AA021908 and U01AA020821). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the Department of Defense.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Confilct of interest
The authors declare no relevant financial arrangement.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
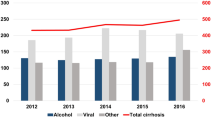
Supplementary Figure 1 Coexistence of alcohol-related diseases based on duration of contact and hospital type - a. ALD in patients diagnosed with AUD; b. ALP in patients diagnosed with AUD; c AUD in patients diagnosed with ALD; d. ALP in patients diagnosed with ALD; e. ALD in patients diagnosed with ALP. ***: <= 0.001, **: <= 0.01, *: <= 0.05.





Rights and permissions
About this article
Cite this article
Arteel, G.E., Singhvi, A., Feldman, R. et al. Coexistent Alcohol-Related Liver Disease and Alcohol-Related Pancreatitis: Analysis of a Large Health Care System Cohort. Dig Dis Sci 67, 2543–2551 (2022). https://doi.org/10.1007/s10620-021-07010-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-021-07010-5