Abstract
Background
The neutrophil–lymphocyte ratio (NLR) has been proposed as a prognostic biomarker for cirrhosis and non-liver malignancies. We aimed to evaluate the prognostic value of NLR in a diverse cohort of patients with hepatocellular carcinoma (HCC).
Methods
We performed a retrospective study of patients diagnosed with HCC between 2008 and 2017 at two large US health systems. We used Cox proportional hazard and multivariable ordinal logistic regression models to identify factors associated with overall survival and response to first HCC treatment, respectively. Primary variables of interest were baseline NLR and delta NLR, defined as the difference between pre- and post-treatment NLR.
Results
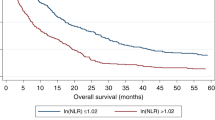
Among 1019 HCC patients, baseline NLR was < 5 in 815 (80.0%) and ≥ 5 in 204 (20.0%). Patients with NLR ≥ 5 had a higher proportion of infiltrative tumors (36.2% vs 22.3%), macrovascular invasion (39.6% vs 25.5%), metastatic disease (20.6% vs 11.4%), and AFP > 200 ng/mL (45.6% vs 33.8%). Baseline NLR ≥ 5 was independently associated with higher mortality (median survival 4.3 vs 15.1 months; adjusted HR 1.70, 95%CI 1.41–2.06), with differences in survival consistent across BCLC stages. After adjusting for baseline covariates including NLR, delta NLR > 0.26 was also independently associated with increased mortality (HR 1.42, 95%CI 1.14–1.78). In a secondary analysis, high NLR was associated with lower odds of response to HCC treatment (20.2% vs 31.6%; adjusted OR 0.55, 95%CI 0.32–0.95).
Conclusions
In a large Western cohort of patients with HCC, high baseline NLR and delta NLR were independent predictors of mortality.
Impact
NLR is an inexpensive test that may be a useful component of future HCC prognostic models.



Similar content being viewed by others
Abbreviations
- AASLD:
-
American Association for the Study of Liver Diseases
- AFP:
-
Alpha-fetoprotein
- ECOG:
-
Eastern Cooperative Oncology Group
- EMR:
-
Electronic medical record
- HBV:
-
Hepatitis B virus
- HCC:
-
Hepatocellular carcinoma
- HCV:
-
Hepatitis C virus
- HR:
-
Hazard ratio
- MELD:
-
Model for End-Stage Liver Disease
- NAFLD:
-
Nonalcoholic fatty liver disease
- NLR:
-
Neutrophil–lymphocyte ratio
References
El-Serag HB. Hepatocellular carcinoma. N Engl J Med 2011;365:1118–1127.
Llovet JM, Bru C, Bruix J. Prognosis of hepatocellular carcinoma: the BCLC staging classification. Semin Liver Dis 1999;19:329–338.
Xiao WK, Chen D, Li SQ et al. Prognostic significance of neutrophil-lymphocyte ratio in hepatocellular carcinoma: a meta-analysis. BMC Cancer 2014;14:117.
Duan J, Pan L, Yang M. Preoperative elevated neutrophil-to-lymphocyte ratio (NLR) and derived NLR are associated with poor prognosis in patients with breast cancer: a meta-analysis. Medicine (Baltimore) 2018;97:e13340.
Mowbray NG, Griffith D, Hammoda M et al. A meta-analysis of the utility of the neutrophil-to-lymphocyte ratio in predicting survival after pancreatic cancer resection. HPB (Oxford) 2018;20:379–384.
Tan DW, Fu Y, Su Q et al. Prognostic significance of neutrophil to lymphocyte ratio in oncologic outcomes of cholangiocarcinoma: a meta-analysis. Sci Rep 2016;6:33789.
Guthrie GJ, Charles KA, Roxburgh CS et al. The systemic inflammation-based neutrophil-lymphocyte ratio: experience in patients with cancer. Crit Rev Oncol Hematol 2013;88:218–230.
Zahorec R. Ratio of neutrophil to lymphocyte counts–rapid and simple parameter of systemic inflammation and stress in critically ill. Bratisl Lek Listy 2001;102:5–14.
Mano Y, Shirabe K, Yamashita Y et al. Preoperative neutrophil-to-lymphocyte ratio is a predictor of survival after hepatectomy for hepatocellular carcinoma: a retrospective analysis. Ann Surg 2013;258:301–305.
Huang ZL, Luo J, Chen MS et al. Blood neutrophil-to-lymphocyte ratio predicts survival in patients with unresectable hepatocellular carcinoma undergoing transarterial chemoembolization. J Vasc Interv Radiol 2011;22:702–709.
Oh BS, Jang JW, Kwon JH et al. Prognostic value of C-reactive protein and neutrophil-to-lymphocyte ratio in patients with hepatocellular carcinoma. BMC Cancer 2013;13:78.
Dan J, Zhang Y, Peng Z et al. Postoperative neutrophil-to-lymphocyte ratio change predicts survival of patients with small hepatocellular carcinoma undergoing radiofrequency ablation. PLOS ONE 2013;8:e58184.
Tayob N, Richardson P, White DL et al. Evaluating screening approaches for hepatocellular carcinoma in a cohort of HCV related cirrhosis patients from the Veteran’s Affairs Health Care System. BMC Med Res Methodol 2018;18:1–1.
Tayob N, Lok AS, Do KA et al. Improved detection of hepatocellular carcinoma by using a longitudinal alpha-fetoprotein screening algorithm. Clin Gastroenterol Hepatol 2016;14:e2.
White DL, Richardson P, Tayoub N et al. The updated model: an adjusted serum alpha-fetoprotein-based algorithm for hepatocellular carcinoma detection with hepatitis C virus-related cirrhosis. Gastroenterology 2015;149:1986–1987.
Lai Q, Inostroza M, Rico Juri JM et al. Delta-slope of alpha-fetoprotein improves the ability to select liver transplant patients with hepatocellular cancer. HPB Off J Int Hepato Pancreato Biliary Assoc 2015;17:1085–1095.
Pannu AK, Bhalla A, Rao C et al. Delta model for end-stage liver disease and delta clinical prognostic indicator as predictors of mortality in patients with viral acute liver failure. Int J Crit Ill Injury Sci 2017;7:252–255.
Yopp AC, Mansour JC, Beg MS et al. Establishment of a multidisciplinary hepatocellular carcinoma clinic is associated with improved clinical outcome. Ann Surg Oncol 2014;21:1287–1295.
Rich NE, Hester C, Odewole M et al. Racial and ethnic differences in presentation and outcomes of hepatocellular carcinoma. Clin Gastroenterol Hepatol 2019;17:e1.
Hester CA, Rich NE, Singal AG et al. Comparative analysis of nonalcoholic steatohepatitis-versus viral hepatitis- and alcohol-related liver disease-related hepatocellular carcinoma. J Natl Compr Canc Netw 2019;17:322–329.
Marrero JA, Kulik LM, Sirlin CB et al. Diagnosis, staging, and management of hepatocellular carcinoma: 2018 practice guidance by the american association for the study of liver diseases. Clin Liver Disease 2019;13:1–1.
Harris PA, Taylor R, Thielke R et al. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–381.
Harris PA, Taylor R, Thielke R et al. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–381.
Yopp AC, Mokdad A, Zhu H et al. Infiltrative hepatocellular carcinoma: natural history and comparison with multifocal, nodular hepatocellular carcinoma. Ann Surg Oncol 2015;22:1075–1082.
Lencioni R, Llovet JM. Modified RECIST (mRECIST) assessment for hepatocellular carcinoma. Semin Liver Dis 2010;30:52–60.
McNally ME, Martinez A, Khabiri H et al. Inflammatory markers are associated with outcome in patients with unresectable hepatocellular carcinoma undergoing transarterial chemoembolization. Ann Surg Oncol 2013;20:923–928.
Halazun KJ, Hardy MA, Rana AA et al. Negative impact of neutrophil-lymphocyte ratio on outcome after liver transplantation for hepatocellular carcinoma. Ann Surg 2009;250:141–151.
Walsh SR, Cook EJ, Goulder F et al. Neutrophil-lymphocyte ratio as a prognostic factor in colorectal cancer. J Surg Oncol 2005;91:181–184.
Zhou Q, Hong L, Zuo M-Z et al. Prognostic significance of neutrophil to lymphocyte ratio in ovarian cancer: evidence from 4910 patients. Oncotarget 2017;8:68938–68949.
Wong L, Bozhilov K, Hernandez B et al. Underlying liver disease and advanced stage liver cancer are associated with elevated neutrophil-lymphocyte ratio. Clin Mol Hepatol 2019;25:305–316.
Rich NE, John BV, Parikh ND et al. Hepatocellular Carcinoma Demonstrates Heterogeneous Growth Patterns in a Multicenter Cohort of Patients With Cirrhosis. Hepatol 2020;72:1654–1665.
Nathani P, Gopal P, Rich N et al. Hepatocellular carcinoma tumour volume doubling time: a systematic review and meta-analysis. Gut 2021;70:401–407. https://doi.org/10.1136/gutjnl-2020-321040.
Biyik M, Ucar R, Solak Y et al. Blood neutrophil-to-lymphocyte ratio independently predicts survival in patients with liver cirrhosis. Eur J Gastroenterol Hepatol 2013;25:435–441.
Rice J, Dodge JL, Bambha KM et al. Neutrophil-to-lymphocyte ratio associates independently with mortality in hospitalized patients with cirrhosis. Clin Gastroenterol Hepatol 2018;16:e1.
Moreau N, Wittebole X, Fleury Y et al. Neutrophil-to-lymphocyte ratio predicts death in acute-on-chronic liver failure patients admitted to the intensive care unit: a retrospective cohort study. Shock 2018;49:385–392.
Forrest EH, Storey N, Sinha R et al. Baseline neutrophil-to-lymphocyte ratio predicts response to corticosteroids and is associated with infection and renal dysfunction in alcoholic hepatitis. Aliment Pharmacol Ther 2019;50:442–453.
Lin J, Zhang W, Huang Y et al. Sarcopenia is associated with the neutrophil/lymphocyte and platelet/lymphocyte ratios in operable gastric cancer patients: a prospective study. Cancer Manag Res 2018;10:4935–4944.
Bonnel AR, Bunchorntavakul C, Reddy KR. Immune dysfunction and infections in patients with cirrhosis. Clin Gastroenterol Hepatol 2011;9:727–738.
Tazzyman S, Lewis CE, Murdoch C. Neutrophils: key mediators of tumour angiogenesis. Int J Exp Pathol 2009;90:222–231.
Fridman WH, Pagès F, Sautès-Fridman C et al. The immune contexture in human tumours: impact on clinical outcome. Nat Rev Cancer 2012;12:298.
Alkhouri N, Morris-Stiff G, Campbell C et al. Neutrophil to lymphocyte ratio: a new marker for predicting steatohepatitis and fibrosis in patients with nonalcoholic fatty liver disease. Liver Int 2012;32:297–302.
Seong YW, Han SJ, Jung W et al. Perioperative change in neutrophil-to-lymphocyte ratio (NLR) is a prognostic factor in patients with completely resected primary pulmonary sarcomatoid carcinoma. J Thorac Disease 2019;11:819–826.
Li Z, Zhao R, Cui Y et al. The dynamic change of neutrophil to lymphocyte ratio can predict clinical outcome in stage I–III colon cancer. Sci Rep 2018;8:9453.
Funding
Dr. Singal’s research was supported by National Cancer Institute R01 CA222900 and R01 MD12565. Dr. Hoshida was supported by Cancer Prevention and Research Institute of Texas RR180016. Dr. Marrero was supported by NIH R01 CA237659. Dr. Rich was supported by the Texas Health Resources Clinical Scholar Award. This research was supported in part by NIH UL-1TR001105 and CTSA NIH UL-1 RR024982. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
Drs. Singal and Rich had full access to all of the data in the study and take responsibility for the integrity of the data and accuracy of the data analysis and were involved in study concept and design and analysis and interpretation of the data; Rich, Parvathaneni, Sen, and Odewole performed acquisition of the data; Rich, Parvathaneni, and Singal drafted the manuscript; all authors provided critical revision of the manuscript for important intellectual content; Singal obtained funding and has given administrative, technical, and material support and supervised the study. Amit Singal is the guarantor of the article.
Corresponding author
Ethics declarations
Conflict of interest
Jorge Marrero has served as a consultant for Glycotest and received research funding from AstraZeneca. Amit Singal has been on advisory boards and served as a consultant for Wako Diagnostics, Roche, Exact Sciences, Glycotest, GRAIL, Bayer, Eisai, BMS, Exelixis, AstraZeneca, Genentech, and TARGET-RWE. Ju Dong Yang has served as a consultant for Exact Sciences, Gilead Sciences, and Eisai. The other authors have no relevant conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Nicole E. Rich and Aarthi Parvathaneni have contributed equally to this work.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Rich, N.E., Parvathaneni, A., Sen, A. et al. High Neutrophil–Lymphocyte Ratio and Delta Neutrophil–Lymphocyte Ratio Are Associated with Increased Mortality in Patients with Hepatocellular Cancer. Dig Dis Sci 67, 2666–2676 (2022). https://doi.org/10.1007/s10620-021-07001-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-021-07001-6