Abstract
Background and Aims
Information concerning deep radiological healing of perianal fistulas in Chinese patients with CD is limited. The present study aimed to establish the effectiveness of infliximab on CD-related perianal fistulas using magnetic resonance imaging (MRI) and identify predictors of deep radiological remission of fistulas.
Methods
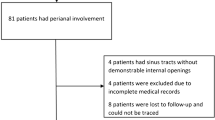
We retrospectively reviewed patients with CD with draining perianal fistulas treated with infliximab and included only those who underwent clinical assessment and MRI before and after infliximab therapy.
Results
Among 178 patients who underwent repeated MRI and clinical assessment, 65.2% had complex fistulas. Post-infliximab therapy, 55.1% of patients with perianal fistulizing CD showed clinical remission and 26.4% presented a clinical response; 38.2% had deep radiological remission, and 34.3% had a partial response based on the Ng score; the Van Assche scores decreased obviously compared with baseline. Prolonged infliximab infusion (18 times) presented higher radiological remission rates in patients with CD with complex fistulas. Concomitant treatment with azathioprine increased the fistula healing rate compared with infliximab alone (50% vs. 36.9%, P < 0.001). Younger age at diagnosis of CD, proctitis and requiring perianal surgery were identified as predictors of poor deep radiological remission of fistulas. Eight of ten patients who stopped infliximab and switched to an alternative agent retained a status of fistula healing in the first year of follow-up.
Conclusions
Infliximab induced deep radiological remission of perianal fistulas in Chinese patients with CD. Routine MRI should be used to monitor fistula healing. Patients with younger age at diagnosis of CD, proctitis, and/or requiring perianal surgery should receive combined therapy and careful monitoring.




Similar content being viewed by others
References
Molodecky NA, Soon IS, Rabi DM, et al. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology 2012;142:46–54 e42; quiz e30.
Park SH, Kim YJ, Rhee KH, et al. A 30-year trend analysis in the epidemiology of inflammatory bowel disease in the Songpa-Kangdong District of Seoul, Korea in 1986–2015. J Crohns Colitis. 2019;13:1410–1417.
Song EM, Lee HS, Kim YJ, et al. Incidence and outcomes of perianal disease in an asian population with Crohn’s disease: a Nationwide Population-Based Study. Dig Dis Sci. 2020;65:1189–1196.
Zhao J, Ng SC, Lei Y, et al. First prospective, population-based inflammatory bowel disease incidence study in mainland of China: the emergence of “western” disease. Inflamm Bowel Dis. 2013;19:1839–1845.
Zeng Z, Zhu Z, Yang Y, et al. Incidence and clinical characteristics of inflammatory bowel disease in a developed region of Guangdong Province, China: a prospective population-based study. J Gastroenterol Hepatol. 2013;28:1148–1153.
Mak WY, Mak OS, Lee CK, et al. Significant medical and surgical morbidity in perianal Crohn’s disease: results from a territory-wide study. J Crohns Colitis. 2018;12:1392–1398.
Beaugerie L, Seksik P, Nion-Larmurier I, et al. Predictors of Crohn’s disease. Gastroenterology. 2006;130:650–656.
Park SH, Aniwan S, Scott Harmsen W, et al. Update on the natural course of fistulizing perianal Crohn’s disease in a population-based cohort. Inflamm Bowel Dis. 2019;25:1054–1060.
Maconi G, Gridavilla D, Vigano C, et al. Perianal disease is associated with psychiatric co-morbidity in Crohn’s disease in remission. Int J Colorectal Dis. 2014;29:1285–1290.
Tozer PJ, Burling D, Gupta A, et al. Review article: medical, surgical and radiological management of perianal Crohn’s fistulas. Aliment Pharmacol Ther. 2011;33:5–22.
Kotze PG, Shen B, Lightner AY, et al. Modern management of perianal fistulas in Crohn’s disease: future directions. Gut. 2018;67:1181–1194.
Sands BE, Anderson FH, Bernstein CN, et al. Infliximab maintenance therapy for fistulizing Crohn’s disease. N Engl J Med. 2004;350:876–885.
Colombel JF, Sandborn WJ, Rutgeerts P, et al. Adalimumab for maintenance of clinical response and remission in patients with Crohn’s disease: the CHARM trial. Gastroenterology. 2007;132:52–65.
Biemans VBC, van der Meulen-de Jong AE, van der Woude CJ, et al. Ustekinumab for Crohn’s disease: results of the ICC Registry, a nationwide prospective observational cohort study. J Crohns Colitis. 2020;14:33–45.
Sandborn WJ, Feagan BG, Rutgeerts P, et al. Vedolizumab as induction and maintenance therapy for Crohn’s disease. N Engl J Med. 2013;369:711–721.
Louis E, Mary JY, Vernier-Massouille G, et al. Maintenance of remission among patients with Crohn’s disease on antimetabolite therapy after infliximab therapy is stopped. Gastroenterology 2012;142:63–70 e65; quiz e31.
Domenech E, Hinojosa J, Nos P, et al. Clinical evolution of luminal and perianal Crohn’s disease after inducing remission with infliximab: how long should patients be treated? Aliment Pharmacol Ther. 2005;22:1107–1113.
Gecse KB, Bemelman W, Kamm MA, et al. A global consensus on the classification, diagnosis and multidisciplinary treatment of perianal fistulising Crohn’s disease. Gut. 2014;63:1381–1392.
Gecse KB, Sebastian S, Hertogh G, et al. Results of the fifth scientific workshop of the ECCO [II]: clinical aspects of perianal fistulising Crohn’s disease-the unmet needs. J Crohns Colitis. 2016;10:758–765.
Gionchetti P, Dignass A, Danese S, et al. 3rd European evidence-based consensus on the diagnosis and management of Crohn’s Disease 2016: part 2: surgical management and special situations. J Crohns Colitis. 2017;11:135–149.
Tozer P, Ng SC, Siddiqui MR, et al. Long-term MRI-guided combined anti-TNF-alpha and thiopurine therapy for Crohn’s perianal fistulas. Inflamm Bowel Dis. 2012;18:1825–1834.
Chambaz M, Verdalle-Cazes M, Desprez C, et al. Deep remission on magnetic resonance imaging impacts outcomes of perianal fistulizing Crohn’s disease. Dig Liver Dis. 2019;51:358–363.
Yan X, Zhu M, Feng Q, et al. Evaluating the effectiveness of infliximab on perianal fistulizing Crohn’s disease by magnetic resonance imaging. Gastroenterol Rep (Oxf). 2019;7:50–56.
Silverberg MS, Satsangi J, Ahmad T, et al. Toward an integrated clinical, molecular and serological classification of inflammatory bowel disease: report of a Working Party of the 2005 Montreal World Congress of Gastroenterology. Can J Gastroenterol.. 2005;19:5A–36A.
Committee American Gastroenterological Association Clinical Practice. American Gastroenterological Association medical position statement: perianal Crohn’s disease. Gastroenterology. 2003;125:1503–1507.
Present DH, Rutgeerts P, Targan S, et al. Infliximab for the treatment of fistulas in patients with Crohn’s disease. N Engl J Med. 1999;340:1398–1405.
Ng SC, Plamondon S, Gupta A, et al. Prospective evaluation of anti-tumor necrosis factor therapy guided by magnetic resonance imaging for Crohn’s perineal fistulas. Am J Gastroenterol. 2009;104:2973–2986.
Van Assche Gert, Vanbeckevoort Dirk, Bielen Didier, et al. Magnetic resonance imaging of the effects of infliximab on perianal fistulizing Crohn’s disease. Am J Gastroenterol. 2003;98:332–339.
Ng SC, Plamondon S, Gupta A, et al. Prospective assessment of the effect on quality of life of anti-tumour necrosis factor therapy for perineal Crohn’s fistulas. Aliment Pharmacol Ther. 2009;30:757–766.
Li Y, Chen B, Gao X, et al. Current diagnosis and management of Crohn’s disease in China: results from a multicenter prospective disease registry. BMC Gastroenterol. 2019;19:145.
Bouguen G, Siproudhis L, Gizard E, et al. Long-term outcome of perianal fistulizing Crohn’s disease treated with infliximab. Clin Gastroenterol Hepatol. 2013;11(975–981):e971–e974.
Zeitz J, Fournier N, Labenz C, et al. Risk factors for the development of fistulae and stenoses in Crohn disease patients in the swiss inflammatory bowel disease cohort. Inflamm Intest Dis. 2017;1:172–181.
Hanauer SB, Feagan BG, Lichtenstein GR, et al. Maintenance infliximab for Crohn’s disease: the ACCENT I randomised trial. The Lancet. 2002;359:1541–1549.
Tougeron D, Savoye G, Savoye-Collet C, et al. Predicting factors of fistula healing and clinical remission after infliximab-based combined therapy for perianal fistulizing Crohn’s disease. Dig Dis Sci. 2009;54:1746–1752.
Castaño-Milla C, Chaparro M, Saro C, et al. Effectiveness of adalimumab in perianal fistulas in crohn’s disease patients naive to anti-TNF therapy. J Clin Gastroenterol. 2015;49:34–40.
Schoepfer A, Santos J, Fournier N, et al. Systematic analysis of the impact of diagnostic delay on bowel damage in paediatric versus adult onset Crohn’s disease. J Crohns Colitis. 2019;13:1334–1342.
Lionetti P, Bronzini F, Salvestrini C, et al. Response to infliximab is related to disease duration in paediatric Crohn’s disease. Aliment Pharmacol Ther. 2003;18:425–431.
Franke A, McGovern DP, Barrett JC, et al. Genome-wide meta-analysis increases to 71 the number of confirmed Crohn’s disease susceptibility loci. Nat Genet. 2010;42:1118–1125.
Medrano LM, Taxonera C, Gonzalez-Artacho C, et al. Response to infliximab in Crohn’s disease: genetic analysis supporting expression profile. Mediators Inflamm. 2015;2015:318207.
Arijs I, Quintens R, Van Lommel L, et al. Predictive value of epithelial gene expression profiles for response to infliximab in Crohn’s disease. Inflamm Bowel Dis. 2010;16:2090–2098.
Cosnes J, Cattan S, Blain A, et al. Long-term evolution of disease behavior of Crohn’s disease. Inflamm Bowel Dis. 2002;8:244–250.
Lukin DJ. predictors of perianal fistula relapse in Crohn’s disease. Inflamm Bowel Dis. 2019;. https://doi.org/10.1093/ibd/izz198.
Osamura A, Suzuki Y. Fourteen-year anti-TNF therapy in Crohn’s disease patients: clinical characteristics and predictive factors. Dig Dis Sci. 2018;63:204–208.
Yassin NA, Askari A, Warusavitarne J, et al. Systematic review: the combined surgical and medical treatment of fistulising perianal Crohn’s disease. Aliment Pharmacol Ther. 2014;40:741–749.
Colombel JF, Reinisch W, Mantzaris GJ, et al. Randomised clinical trial: deep remission in biologic and immunomodulator naive patients with Crohn’s disease—a SONIC post hoc analysis. Aliment Pharmacol Ther. 2015;41:734–746.
Gomollon F, Dignass A, Annese V, et al. 3rd European evidence-based consensus on the diagnosis and management of Crohn’s disease 2016: Part 1: diagnosis and medical management. J Crohns Colitis. 2017;11:3–25.
Jones JL, Kaplan GG, Peyrin-Biroulet L, et al. Effects of concomitant immunomodulator therapy on efficacy and safety of anti-tumor necrosis factor therapy for Crohn’s disease: a meta-analysis of placebo-controlled trials. Clin Gastroenterol Hepatol 2015;13:2233–2240 e2231–2232; quiz e2177–2238.
Qian X, Wang T, Shen J, Ran Z. Low dose of azathioprine is effective to induce and maintain remission in active Crohn disease: a prospective observational study. Medicine (Baltimore). 2018;97:e11814.
Feng T, Chen B, Ungar B, et al. Association of infliximab levels with mucosal healing is time-dependent in Crohn’s disease: higher drug exposure is required postinduction than during maintenance treatment. Inflamm Bowel Dis. 2019;25:1813–1821.
El-Matary W, Walters TD, Huynh HQ, et al. Higher postinduction infliximab serum trough levels are associated with healing of fistulizing perianal Crohn’s disease in children. Inflamm Bowel Dis. 2019;25:150–155.
Davidov Y, Ungar B, Bar-Yoseph H, et al. Association of induction infliximab levels with clinical response in perianal Crohn’s disease. J Crohns Colitis. 2017;11:549–555.
Plevris N, Jenkinson PW, Arnott ID, et al. Higher anti-tumor necrosis factor levels are associated with perianal fistula healing and fistula closure in Crohn’s disease. Eur J Gastroenterol Hepatol. 2020;32:32–37.
Funding
This work was supported by a grant from the National Natural Science Foundation of China (Nos. 81302095, 81670497, 81701746)
Author information
Authors and Affiliations
Contributions
MMZ and XTX designed the research study, prepared the manuscript, and analyzed data. MMZ, XTX, ZC, and TRW contributed to acquisition and interpretation of data. QF analyzed and calculated the MRI data. YQY provided partial MRI data. ZHR contributed to the study design, revising it critically for important intellectual content, and gave final approval of the version to be submitted.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhu, M., Xu, X., Feng, Q. et al. Effectiveness of Infliximab on Deep Radiological Remission in Chinese Patients with Perianal Fistulizing Crohn’s Disease. Dig Dis Sci 66, 1658–1668 (2021). https://doi.org/10.1007/s10620-020-06398-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-020-06398-w