Abstract
Recent studies have raised interest in the possibility that dysbiosis of the gut microbiome (i.e., the communities of bacteria residing in the intestine) in HIV-infected patients could contribute to chronic immune activation, and, thus, to elevated mortality and increased risk of inflammation-related clinical diseases (e.g., stroke, cardiovascular disease, cancer, long-bone fractures, and renal dysfunction) found even in those on effective antiretroviral therapy. Yet, to date, a consistent pattern of HIV-associated dysbiosis has not been identified. What is becoming clear, however, is that status as a man who has sex with men (MSM) may profoundly impact the structure of the gut microbiota, and that this factor likely confounded many HIV-related intestinal microbiome studies. However, what factor associated with MSM status drives these gut microbiota-related changes is unclear, and what impact, if any, these changes may have on the health of MSM is unknown. In this review, we outline available data on changes in the structure of the gut microbiome in HIV, based on studies that controlled for MSM status. We then examine what is known regarding the gut microbiota in MSM, and consider possible implications for research and the health of this population. Lastly, we discuss knowledge gaps and needed future studies.
Similar content being viewed by others
References
Kazal HL, Sohn N, Carrasco JI, Robilotti JG, Delaney WE. The gay bowel syndrome: clinico-pathologic correlation in 260 cases. Ann Clin Lab Sci. 1976;6:184–192.
Cooper F, Barber T. ’Gay bowel syndrome’: relic or real (and returning) phenomenon? Curr Opin Infect Dis. 2014;27:84–89.
Weller IV. The gay bowel. Gut. 1985;26:869–875.
Quinn TC, Corey L, Chaffee RG, Schuffler MD, Brancato FP, Holmes KK. The etiology of anorectal infections in homosexual men. Am J Med. 1981;71:395–406.
Quinn TC, Goodell SE, Mkrtichian E, et al. Chlamydia trachomatis proctitis. N Engl J Med. 1981;305:195–200.
Laughon BE, Druckman DA, Vernon A, et al. Prevalence of enteric pathogens in homosexual men with and without acquired immunodeficiency syndrome. Gastroenterology. 1988;94:984–993.
Zeitz M, Ullrich R, Schneider T, Kewenig S, Hohloch K, Riecken EO. HIV/SIV enteropathy. Ann N Y Acad Sci. 1998;859:139–148.
Egger M, May M, Chene G, et al. Prognosis of HIV-1-infected patients starting highly active antiretroviral therapy: a collaborative analysis of prospective studies. Lancet. 2002;360:119–129.
Klatt NR, Funderburg NT, Brenchley JM. Microbial translocation, immune activation, and HIV disease. Trends Microbiol. 2013;21:6–13.
Zevin AS, McKinnon L, Burgener A, Klatt NR. Microbial translocation and microbiome dysbiosis in HIV-associated immune activation. Curr Opin HIV AIDS. 2016;11:182–190.
Gootenberg DB, Paer JM, Luevano JM, Kwon DS. HIV-associated changes in the enteric microbial community: potential role in loss of homeostasis and development of systemic inflammation. Curr Opin Infect Dis. 2017;30:31–43.
Guillen Y, Noguera-Julian M, Rivera J, et al. Low nadir CD4 + T-cell counts predict gut dysbiosis in HIV-1 infection. Mucosal Immunol. 2019;12:232–246.
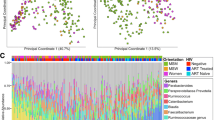
Armstrong AJS, Shaffer M, Nusbacher NM, et al. An exploration of prevotella-rich microbiomes in HIV and men who have sex with men. Microbiome. 2018;6:198.
Noguera-Julian M, Rocafort M, Guillen Y, et al. Gut microbiota linked to sexual preference and HIV infection. EBioMedicine. 2016;5:135–146.
Kehrmann J, Menzel J, Saeedghalati M, et al. Gut microbiota in human immunodeficiency virus-infected individuals linked to coronary heart disease. J Infect Dis. 2019;219:497–508.
Hensley-McBain T, Wu MC, Manuzak JA, et al. Increased mucosal neutrophil survival is associated with altered microbiota in HIV infection. PLoS Pathog. 2019;15:e1007672.
Kelley CF, Kraft CS, de Man TJ, et al. The rectal mucosa and condomless receptive anal intercourse in HIV-negative MSM: implications for HIV transmission and prevention. Mucosal Immunol. 2017;10:996–1007.
Li SX, Sen S, Schneider JM, et al. Gut microbiota from high-risk men who have sex with men drive immune activation in gnotobiotic mice and in vitro HIV infection. PLoS Pathog. 2019;15:e1007611.
Neff CP, Krueger O, Xiong K, et al. Fecal microbiota composition drives immune activation in HIV-infected individuals. EBioMedicine. 2018;30:192–202.
Pescatore NA, Pollak R, Kraft CS, Mulle JG, Kelley CF. Short communication: anatomic site of sampling and the rectal mucosal microbiota in HIV negative men who have sex with men engaging in condomless receptive anal intercourse. AIDS Res Hum Retrovir. 2018;34:277–281.
Marcus JL, Chao CR, Leyden WA, et al. Narrowing the gap in life expectancy between HIV-infected and HIV-uninfected individuals with access to care. J Acquir Immune Defic Syndr. 2016;73:39–46.
Coghill AE, Pfeiffer RM, Shiels MS, Engels EA. Excess mortality among HIV-infected individuals with cancer in the United States. Cancer Epidemiol Biomark Prev. 2017;26:1027–1033.
Kroeze S, Wit FW, Rossouw TM, et al. Plasma biomarkers of HIV-related systemic inflammation and immune activation in sub-Saharan Africa before and during suppressive antiretroviral therapy. J Infect Dis. 2019;220:1029–1033.
Kelesidis T, Kendall MA, Yang OO, Hodis HN, Currier JS. Biomarkers of microbial translocation and macrophage activation: association with progression of subclinical atherosclerosis in HIV-1 infection. J Infect Dis. 2012;206:1558–1567.
Manner IW, Baekken M, Kvale D, et al. Markers of microbial translocation predict hypertension in HIV-infected individuals. HIV Med. 2013;14:354–361.
Pedersen KK, Pedersen M, Troseid M, et al. Microbial translocation in HIV infection is associated with dyslipidemia, insulin resistance, and risk of myocardial infarction. J Acquir Immune Defic Syndr. 2013;64:425–433.
Tuddenham S, Sears CL. The intestinal microbiome and health. Curr Opin Infect Dis. 2015;28:464–470.
Safety of FMT Using Oral Encapsulated PRIM-DJ2727 in HIV. https://ClinicalTrials.gov/show/NCT03329560. Accessed August 1, 2019.
Vujkovic-Cvijin I, Dunham RM, Iwai S, et al. Dysbiosis of the gut microbiota is associated with HIV disease progression and tryptophan catabolism. Sci Transl Med. 2013;5:193ra91.
Vujkovic-Cvijin I, Rutishauser RL, Pao M, et al. Limited engraftment of donor microbiome via one-time fecal microbial transplantation in treated HIV-infected individuals. Gut Microbes. 2017;8:440–450.
Overton ET, Yeh E, Presti R, et al. Assessing the probiotic effect in treated HIV: results of ACTG A5350. Abstract #35. In: Conference on retroviruses and opportunistic infections. Seattle, USA, 2019.
Villar-García J, Güerri-Fernández R, Moya A, et al. Impact of probiotic Saccharomyces boulardii on the gut microbiome composition in HIV-treated patients: a double-blind, randomised, placebo-controlled trial. PLoS ONE. 2017;12:e0173802.
Ceccarelli G, Brenchley JM, Cavallari EN, et al. Impact of high-dose multi-strain probiotic supplementation on neurocognitive performance and central nervous system immune activation of HIV-1 infected individuals. Nutrients. 2017;9:1269.
Serrano-Villar S, de Lagarde M, Vazquez-Castellanos J, et al. Effects of immunonutrition in advanced human immunodeficiency virus disease: a randomized placebo-controlled clinical trial (promaltia study). Clin Infect Dis. 2019;68:120–130.
Schunter M, Chu H, Hayes TL, et al. Randomized pilot trial of a synbiotic dietary supplement in chronic HIV-1 infection. BMC Complement Altern Med. 2012;12:84.
Kim CJ, Walmsley SL, Raboud JM, et al. Can probiotics reduce inflammation and enhance gut immune health in people living with HIV: study designs for the probiotic visbiome for inflammation and translocation (PROOV IT) pilot trials. HIV Clin Trials. 2016;17:147–157.
Meyer-Myklestad MH, Kummen M, Stiksrud B, et al. Assessing the probiotic effect in treated HIV: results of ACTG A5350. Abstract #209. In: Conference on retroviruses and opportunistic infections. Seattle, USA (2019).
Stiksrud B, Nowak P, Nwosu FC, et al. Reduced levels of D-dimer and changes in gut microbiota composition after probiotic intervention in HIV-infected individuals on stable ART. J Acquir Immune Defic Syndr. 2015;70:329–337.
d’Ettorre G, Ceccarelli G, Giustini N, et al. Probiotics reduce inflammation in antiretroviral treated, HIV-infected individuals: results of the “Probio-HIV” clinical trial. PloS ONE. 2015;10:e0137200.
The role of probiotics in HIV patients with immunological non-responder. https://ClinicalTrials.gov/show/NCT03568812. Accessed August 1, 2019.
Clinical Trial to Evaluate the Addition to an Antiretroviral Treatment of a Probiotic. https://ClinicalTrials.gov/show/NCT03542786. Accessed August 1, 2019.
The Effect of Probiotics on Microbial Translocation and Inflammation in HIV-infected Patients. https://ClinicalTrials.gov/show/NCT02764684. Accessed August 1, 2019.
Pilot Study of Oral Probiotic Bacteria Supplementation to Reduce Chronic Immune Activation in HIV-infected Malian Women. https://ClinicalTrials.gov/show/NCT02448238. Accessed August 1, 2019.
Fecal Microbiota Transplantation in HIV (FMT-HIV).https://ClinicalTrials.gov/show/NCT02256592. Accessed August 1, 2019.
Microbiota Restoration Therapy in HIV With Repeated Low-Dose Interventions (REFRESH). https://ClinicalTrials.gov/show/NCT03008941. Accessed August 1, 2019.
Missailidis C, Sorensen N, Ashenafi S, et al. Vitamin D and phenylbutyrate supplementation does not modulate gut derived immune activation in HIV-1. Nutrients. 2019;11:1675.
Gori A, Rizzardini G, Van’t Land B, et al. Specific prebiotics modulate gut microbiota and immune activation in HAART-naive HIV-infected adults: results of the “COPA” pilot randomized trial. Mucosal Immunol. 2011;4:554–563.
Wolf BW, Wheeler KB, Ataya DG, Garleb KA. Safety and tolerance of Lactobacillus reuteri supplementation to a population infected with the human immunodeficiency virus. Food Chem Toxicol. 1998;36:1085–1094.
Hummelen R, Hemsworth J, Changalucha J, et al. Effect of micronutrient and probiotic fortified yogurt on immune-function of anti-retroviral therapy naive HIV patients. Nutrients. 2011;3:897–909.
Dubourg G, Lagier JC, Hue S, et al. Gut microbiota associated with HIV infection is significantly enriched in bacteria tolerant to oxygen. BMJ Open Gastroenterol. 2016;3:e000080.
Mutlu EA, Keshavarzian A, Losurdo J, et al. A compositional look at the human gastrointestinal microbiome and immune activation parameters in HIV infected subjects. PLoS Pathog. 2014;10:e1003829.
Nowak P, Troseid M, Avershina E, et al. Gut microbiota diversity predicts immune status in HIV-1 infection. AIDS. 2015;29:2409–2418.
Pinto-Cardoso S, Lozupone C, Briceno O, et al. Fecal Bacterial Communities in treated HIV infected individuals on two antiretroviral regimens. Sci Rep. 2017;7:43741.
Villanueva-Millan MJ, Perez-Matute P, Recio-Fernandez E, Lezana Rosales JM, Oteo JA. Differential effects of antiretrovirals on microbial translocation and gut microbiota composition of HIV-infected patients. J Int AIDS Soc. 2017;20:21526.
Yu G, Fadrosh D, Ma B, Ravel J, Goedert JJ. Anal microbiota profiles in HIV-positive and HIV-negative MSM. AIDS. 2014;28:753–760.
Sun Y, Ma Y, Lin P, et al. Fecal bacterial microbiome diversity in chronic HIV-infected patients in China. Emerg Microbes Infect. 2016;5:e31.
Vazquez-Castellanos JF, Serrano-Villar S, Latorre A, et al. Altered metabolism of gut microbiota contributes to chronic immune activation in HIV-infected individuals. Mucosal Immunol. 2015;8:760–772.
Monaco CL, Gootenberg DB, Zhao G, et al. Altered virome and bacterial microbiome in human immunodeficiency virus-associated acquired immunodeficiency syndrome. Cell Host Microbe. 2016;19:311–322.
Vesterbacka J, Rivera J, Noyan K, et al. Richer gut microbiota with distinct metabolic profile in HIV infected elite controllers. Sci Rep. 2017;7:6269.
Dillon SM, Lee EJ, Kotter CV, et al. An altered intestinal mucosal microbiome in HIV-1 infection is associated with mucosal and systemic immune activation and endotoxemia. Mucosal Immunol. 2014;7:983.
Volpe GE, Ward H, Mwamburi M, et al. Associations of cocaine use and HIV infection with the intestinal microbiota, microbial translocation, and inflammation. J Stud Alcohol Drugs. 2014;75:347–357.
Dinh DM, Volpe GE, Duffalo C, et al. Intestinal microbiota, microbial translocation, and systemic inflammation in chronic HIV infection. J Infect Dis. 2015;211:19–27.
Lozupone CA, Rhodes ME, Neff CP, Fontenot AP, Campbell TB, Palmer BE. HIV-induced alteration in gut microbiota: driving factors, consequences, and effects of antiretroviral therapy. Gut Microbes. 2014;5:562–570.
Lozupone CA, Li M, Campbell TB, et al. Alterations in the gut microbiota associated with HIV-1 infection. Cell Host Microbe. 2013;14:329–339.
Nowak RG, Bentzen SM, Ravel J, et al. Rectal microbiota among HIV-uninfected, untreated HIV, and treated HIV-infected in Nigeria. AIDS. 2017;31:857–862.
Serrano-Villar S, Vasquez-Dominguez E, Perez-Molina JA, et al. HIV, HPV, and microbiota: partners in crime? AIDS. 2017;31:591–594.
Pérez-Santiago J, Gianella S, Massanella M, et al. Gut Lactobacillales are associated with higher CD4 and less microbial translocation during HIV infection. AIDS (Lond Engl). 2013;27:1921–1931.
Serrano-Villar S, Vazquez-Castellanos JF, Vallejo A, et al. The effects of prebiotics on microbial dysbiosis, butyrate production and immunity in HIV-infected subjects. Mucosal Immunol. 2017;10:1279–1293.
Fulcher JA, Hussain SK, Cook R, et al. Effects of substance use and sex practices on the intestinal microbiome during HIV-1 infection. J Infect Dis. 2018;218:1560–1570.
Rhoades N, Mendoza N, Jankeel A, et al. Altered immunity and microbial dysbiosis in aged individuals with long-term controlled HIV infection. Front Immunol. 2019;10:463.
Moon JY, Zolnik CP, Wang Z, et al. Gut microbiota and plasma metabolites associated with diabetes in women with, or at high risk for HIV infection. EBioMedicine. 2018;37:392–400.
Machiavelli A, Duarte RTD, Pires MMS, Zarate-Blades CR, Pinto AR. The impact of in utero HIV exposure on gut microbiota, inflammation, and microbial translocation. Gut Microbes. 2019;10:1–16.
Williams B, Weber K, Chlipala G, Evans C, Morack R, French A. HIV status does not affect rectal microbiome composition, diversity, or stability over time: a Chicago Women’s interagency HIV study. AIDS Res Hum Retrovir. 2019;35:260–266.
Lee SC, Chua LL, Yap SH, et al. Enrichment of gut-derived Fusobacterium is associated with suboptimal immune recovery in HIV-infected individuals. Sci Rep. 2018;8:14277.
Cook RR, Fulcher JA, Tobin NH, et al. Effects of HIV viremia on the gastrointestinal microbiome of young MSM. AIDS. 2019;33:793–804.
Lu W, Feng Y, Jing F, et al. Association between gut microbiota and CD4 recovery in HIV-1 infected patients. Front Microbiol. 2018;9:1451.
Nowak RG, Bentzen SM, Ravel J, et al. Anal microbial patterns and oncogenic human papillomavirus in a pilot study of Nigerian men who have sex with men at risk for or living with HIV. AIDS Res Hum Retrovir. 2019;35:267–275.
Chang JY, Antonopoulos DA, Kalra A, et al. Decreased diversity of the fecal microbiome in recurrent clostridium difficile-associated diarrhea. J Infect Dis. 2008;197:435–438.
Ni J, Wu GD, Albenberg L, Tomov VT. Gut microbiota and IBD: causation or correlation? Nat Rev Gastroenterol Hepatol. 2017;14:573–584.
Taur Y, Jenq RR, Perales MA, et al. The effects of intestinal tract bacterial diversity on mortality following allogeneic hematopoietic stem cell transplantation. Blood. 2014;124:1174–1182.
Turnbaugh PJ, Hamady M, Yatsunenko T, et al. A core gut microbiome in obese and lean twins. Nature. 2009;457:480–484.
Li SX, Armstrong A, Neff CP, Shaffer M, Lozupone CA, Palmer BE. Complexities of gut microbiome dysbiosis in the context of HIV infection and antiretroviral therapy. Clin Pharmacol Ther. 2016;99:600–611.
Ling Z, Jin C, Xie T, Cheng Y, Li L, Wu N. Alterations in the fecal microbiota of patients with HIV-1 infection: an observational study in a Chinese population. Sci Rep. 2016;6:30673.
Dillon SM, Lee EJ, Kotter CV, et al. Gut dendritic cell activation links an altered colonic microbiome to mucosal and systemic T-cell activation in untreated HIV-1 infection. Mucosal Immunol. 2016;9:24–37.
Maurice JB, Garvey L, Tsochatzis EA, et al. Monocyte-macrophage activation is associated with nonalcoholic fatty liver disease and liver fibrosis in HIV monoinfection independently of the gut microbiome and bacterial translocation. AIDS. 2019;33:805–814.
Tuddenham SA, Koay WLA, Zhao N, et al. The Impact of HIV infection on gut microbiota alpha-diversity: an individual level meta-analysis. Clin Infect Dis. 2020;70:615–627.
Gianella S, Chaillon A, Mutlu EA, et al. Effect of cytomegalovirus and Epstein-Barr virus replication on intestinal mucosal gene expression and microbiome composition of HIV-infected and uninfected individuals. AIDS. 2017;31:2059–2067.
Dillon SM, Lee EJ, Donovan AM, et al. Enhancement of HIV-1 infection and intestinal CD4 + T cell depletion ex vivo by gut microbes altered during chronic HIV-1 infection. Retrovirology. 2016;13:5.
Dillon SM, Kibbie J, Lee EJ, et al. Low abundance of colonic butyrate-producing bacteria in HIV infection is associated with microbial translocation and immune activation. AIDS. 2017;31:511–521.
Deusch S, Serrano-Villar S, Rojo D, et al. Effects of HIV, antiretroviral therapy and prebiotics on the active fraction of the gut microbiota. AIDS. 2018;32:1229–1237.
Missailidis C, Neogi U, Stenvinkel P, Troseid M, Nowak P, Bergman P. The microbial metabolite trimethylamine-N-oxide in association with inflammation and microbial dysregulation in three HIV cohorts at various disease stages. AIDS. 2018;32:1589–1598.
San-Juan-Vergara H, Zurek E, Ajami NJ, et al. A Lachnospiraceae-dominated bacterial signature in the fecal microbiota of HIV-infected individuals from Colombia, South America. Sci Rep. 2018;8:4479.
Zhou Y, Ou Z, Tang X, et al. Alterations in the gut microbiota of patients with acquired immune deficiency syndrome. J Cell Mol Med. 2018;22:2263–2271.
Liu J, Johnson R, Dillon S, et al. Among older adults, age-related changes in the stool microbiome differ by HIV-1 serostatus. EBioMedicine. 2019;40:583–594.
Rocafort M, Noguera-Julian M, Rivera J, et al. Evolution of the gut microbiome following acute HIV-1 infection. Microbiome. 2019;7:73.
McHardy IH, Li X, Tong M, et al. HIV Infection is associated with compositional and functional shifts in the rectal mucosal microbiota. Microbiome. 2013;1:26.
Vazquez-Castellanos JF, Serrano-Villar S, Jimenez-Hernandez N, et al. Interplay between gut microbiota metabolism and inflammation in HIV infection. ISME J. 2018;12:1964–1976.
Qing Y, Xie H, Su C, et al. Gut microbiome, short-chain fatty acids, and mucosa injury in young adults with human immunodeficiency virus infection. Dig Dis Sci. 2019;64:1830–1843. https://doi.org/10.1007/s10620-018-5428-2.
Paquin-Proulx D, Ching C, Vujkovic-Cvijin I, et al. Bacteroides are associated with GALT iNKT cell function and reduction of microbial translocation in HIV-1 infection. Mucosal Immunol. 2017;10:69–78.
Tincati C, Merlini E, Braidotti P, et al. Impaired gut junctional complexes feature late-treated individuals with suboptimal CD4 + T-cell recovery upon virologically suppressive combination antiretroviral therapy. AIDS. 2016;30:991–1003.
Hoenigl M, Perez-Santiago J, Nakazawa M, et al. (1– > 3)-beta-d-Glucan: a biomarker for microbial translocation in individuals with acute or early HIV infection? Front Immunol. 2016;7:404.
Hoel H, Hove-Skovsgaard M, Hov JR, et al. Impact of HIV and tyype 2 diabetes on gut microbiota diversity, tryptophan catabolism and endothelial dysfunction. Sci Rep. 2018;8:6725.
Arnbjerg CJ, Vestad B, Hov JR, et al. Effect of Lactobacillus rhamnosus GG supplementation on intestinal inflammation assessed by PET/MRI scans and gut microbiota composition in HIV-infected individuals. J Acquir Immune Defic Syndr. 2018;78:450–457.
Ji Y, Zhang F, Zhang R, et al. Changes in intestinal microbiota in HIV-1-infected subjects following cART initiation: influence of CD4 + T cell count. Emerg Microbes Infect. 2018;7:113.
Zhang F, Yang J, Ji Y, et al. Gut microbiota dysbiosis is not independently associated with neurocognitive impairment in people living with HIV. Front Microbiol. 2018;9:3352.
Sortino O, Hullsiek KH, Richards E, et al. The effects of recombinant human lactoferrin on immune activation and the intestinal microbiome among persons living with human immunodeficiency virus and receiving antiretroviral therapy. J Infect Dis. 2019;219:1963–1968.
Shenoy MK, Fadrosh DW, Lin DL, et al. Gut microbiota in HIV-pneumonia patients is related to peripheral CD4 counts, lung microbiota, and in vitro macrophage dysfunction. Microbiome. 2019;7:37.
Storm-Larsen C, Stiksrud B, Eriksen C, et al. Microbial translocation revisited: targeting the endotoxic potential of gut microbes in HIV-infected individuals. AIDS. 2019;33:645–653.
Tett A, Huang KD, Asnicar F, et al. The Prevotella copri complex comprises four distinct clades underrepresented in westernized populations. Cell Host Microbe. 2019;26:666–679.
Yatsunenko T, Rey FE, Manary MJ, et al. Human gut microbiome viewed across age and geography. Nature. 2012;486:222–227.
Schnorr SL, Candela M, Rampelli S, et al. Gut microbiome of the Hadza hunter-gatherers. Nat Commun. 2014;5:3654.
De Filippo C, Cavalieri D, Di Paola M, et al. Impact of diet in shaping gut microbiota revealed by a comparative study in children from Europe and rural Africa. Proc Natl Acad Sci USA. 2010;107:14691–14696.
Jain A, Li XH, Chen WN. Similarities and differences in gut microbiome composition correlate with dietary patterns of Indian and Chinese adults. AMB Exp. 2018;8:104.
Habel MA, Leichliter JS, Dittus PJ, Spicknall IH, Aral SO. Heterosexual anal and oral sex in adolescents and adults in the United States, 2011–2015. Sex Transm Dis. 2018;45:775–782.
Benson LS, Martins SL, Whitaker AK. Correlates of heterosexual anal intercourse among women in the 2006–2010 national survey of family growth. J Sex Med. 2015;12:1746–1752.
Rolle CP, Bolton MD, Kelley CF. Use of a prospective sex diary to study anal lubricant and enema use among high risk men who have sex with men-implications for human immunodeficiency virus prevention. Sex Transm Dis. 2016;43:476–478.
Fuchs EJ, Lee LA, Torbenson MS, et al. Hyperosmolar sexual lubricant causes epithelial damage in the distal colon: potential implication for HIV transmission. J Infect Dis. 2007;195:703–710.
Maierhofer C, Rice CE, Wang SH, Fields KS, Ervin M, Turner AN. Lubricant use and rectal chlamydial and gonococcal infections among men who engage in receptive anal intercourse. Sex Transm Dis. 2016;43:423–428.
Haaland RE, Fountain J, Hu Y, et al. Repeated rectal application of a hyperosmolar lubricant is associated with microbiota shifts but does not affect PrEP drug concentrations: results from a randomized trial in men who have sex with men. J Int AIDS Soc. 2018;21:e25199.
Hassan A, Blumenthal JS, Dube MP, et al. Effect of rectal douching/enema on rectal gonorrhoea and chlamydia among a cohort of men who have sex with men on HIV pre-exposure prophylaxis. Sex Transm Infect. 2018;94:508–514.
Vanhommerig JW, Lambers FA, Schinkel J, et al. Risk factors for sexual transmission of hepatitis C virus among human immunodeficiency virus-infected men who have sex with men: a case-control study. Open Forum Infect Dis. 2015;2:ofv115.
Cornelisse VJ, Fairley CK, Read TRH, et al. Associations between anorectal chlamydia and oroanal sex or saliva use as a lubricant for anal sex: a cross-sectional survey. Sex Transm Dis. 2018;45:506–510.
Chow EPF, Cornelisse VJ, Read TRH, et al. Saliva use as a lubricant for anal sex is a risk factor for rectal gonorrhoea among men who have sex with men, a new public health message: a cross-sectional survey. Sex Transm Infect. 2016;92:532–536.
Lundmark A, Hu YOO, Huss M, Johannsen G, Andersson AF, Yucel-Lindberg T. Identification of salivary microbiota and its association with host inflammatory mediators in periodontitis. Front Cell Infect Microbiol. 2019;9:216.
Palmer CD, Tomassilli J, Sirignano M, et al. Enhanced immune activation linked to endotoxemia in HIV-1 seronegative MSM. AIDS. 2014;28:2162–2166.
Wang J, Hausermann M, Vounatsou P, Aggleton P, Weiss MG. Health status, behavior, and care utilization in the Geneva Gay Men’s Health Survey. Prev Med. 2007;44:70–75.
Hatzenbuehler ML, McLaughlin KA, Slopen N. Sexual orientation disparities in cardiovascular biomarkers among young adults. Am J Prev Med. 2013;44:612–621.
De Filippis F, Pellegrini N, Vannini L, et al. High-level adherence to a Mediterranean diet beneficially impacts the gut microbiota and associated metabolome. Gut. 2016;65:1812–1821.
Kovatcheva-Datchary P, Nilsson A, Akrami R, et al. Dietary fiber-induced improvement in glucose metabolism is associated with increased abundance of prevotella. Cell Metab. 2015;22:971–982.
De Vadder F, Kovatcheva-Datchary P, Zitoun C, Duchampt A, Backhed F, Mithieux G. Microbiota-produced succinate improves glucose homeostasis via intestinal gluconeogenesis. Cell Metab. 2016;24:151–157.
De Angelis M, Montemurno E, Vannini L, et al. Effect of whole-grain barley on the human fecal microbiota and metabolome. Appl Environ Microbiol. 2015;81:7945–7956.
Vitaglione P, Mennella I, Ferracane R, et al. Whole-grain wheat consumption reduces inflammation in a randomized controlled trial on overweight and obese subjects with unhealthy dietary and lifestyle behaviors: role of polyphenols bound to cereal dietary fiber. Am J Clin Nutr. 2015;101:251–261.
Larsen JM. The immune response to Prevotella bacteria in chronic inflammatory disease. Immunology. 2017;151:363–374.
Kasselman LJ, Vernice NA, DeLeon J, Reiss AB. The gut microbiome and elevated cardiovascular risk in obesity and autoimmunity. Atherosclerosis. 2018;271:203–213.
Kelly TN, Bazzano LA, Ajami NJ, et al. Gut microbiome associates with lifetime cardiovascular disease risk profile among bogalusa heart study participants. Circ Res. 2016;119:956–964.
Li J, Zhao F, Wang Y, et al. Gut microbiota dysbiosis contributes to the development of hypertension. Microbiome. 2017;5:14.
Gregory JC, Buffa JA, Org E, et al. Transmission of atherosclerosis susceptibility with gut microbial transplantation. J Biol Chem. 2015;290:5647–5660.
Pedersen HK, Gudmundsdottir V, Nielsen HB, et al. Human gut microbes impact host serum metabolome and insulin sensitivity. Nature. 2016;535:376–381.
Scher JU, Sczesnak A, Longman RS, et al. Expansion of intestinal Prevotella copri correlates with enhanced susceptibility to arthritis. Elife. 2013;2:e01202.
Alpizar-Rodriguez D, Lesker TR, Gronow A, et al. Prevotella copri in individuals at risk for rheumatoid arthritis. Ann Rheum Dis. 2019;78:590–593.
Maeda Y, Kurakawa T, Umemoto E, et al. Dysbiosis contributes to arthritis development via activation of autoreactive T cells in the intestine. Arthritis Rheumatol. 2016;68:2646–2661.
Zhang Y, Zhen M, Zhan Y, Song Y, Zhang Q, Wang J. Population-genomic insights into variation in Prevotella intermedia and Prevotella nigrescens isolates and its association with periodontal disease. Front Cell Infect Microbiol. 2017;7:409.
Deng ZL, Szafranski SP, Jarek M, Bhuju S, Wagner-Dobler I. Dysbiosis in chronic periodontitis: key microbial players and interactions with the human host. Sci Rep. 2017;7:3703.
Beamer MA, Austin MN, Avolia HA, Meyn LA, Bunge KE, Hillier SL. Bacterial species colonizing the vagina of healthy women are not associated with race. Anaerobe. 2017;45:40–43.
Gosmann C, Anahtar MN, Handley SA, et al. Lactobacillus-deficient cervicovaginal bacterial communities are associated with increased HIV acquisition in young South African women. Immunity. 2017;46:29–37.
De Filippis F, Pasolli E, Tett A, et al. Distinct genetic and functional traits of human intestinal Prevotella copri strains are associated with different habitual diets. Cell Host Microbe. 2019;25:444–453.
Kenyon C, Osbak K. Certain attributes of the sexual ecosystem of high-risk MSM have resulted in an altered microbiome with an enhanced propensity to generate and transmit antibiotic resistance. Med Hypotheses. 2014;83:196–202.
Ceccarani C, Marangoni A, Severgnini M, et al. Rectal microbiota associated with Chlamydia trachomatis and Neisseria gonorrhoeae infections in men having sex with other men. Front Cell Infect Microbiol. 2019;9:358.
Ziklo N, Huston WM, Taing K, Katouli M, Timms P. In vitro rescue of genital strains of Chlamydia trachomatis from interferon-gamma and tryptophan depletion with indole-positive, but not indole-negative Prevotella spp. BMC Microbiol. 2016;16:286.
Town K, Obi C, Quaye N, Chisholm S, Hughes G, Group GC. Drifting towards ceftriaxone treatment failure in gonorrhoea: risk factor analysis of data from the Gonococcal Resistance to Antimicrobials Surveillance Programme in England and Wales. Sex Transm Infect. 2017;93:39–45.
Kirkcaldy RD, Harvey A, Papp JR, et al. Neisseria gonorrhoeae antimicrobial susceptibility surveillance—the gonococcal isolate surveillance project, 27 Sites, United States, 2014. MMWR Surveill Summ. 2016;65:1–19.
Molina JM, Charreau I, Spire B, et al. Efficacy, safety, and effect on sexual behaviour of on-demand pre-exposure prophylaxis for HIV in men who have sex with men: an observational cohort study. Lancet HIV. 2017;4:e402–e410.
Kaur US, Shet A, Rajnala N, et al. High abundance of genus prevotella in the gut of perinatally HIV-infected children is associated with IP-10 levels despite therapy. Sci Rep. 2018;8:17679.
Funding
ST is supported by NIH grant K23-AI125715 (PI: Tuddenham). CLS is supported, in part, by funds of the Johns Hopkins University School of Medicine and Department of Medicine. ST and CLS’ work on HIV and gut microbiome has been supported by a Willowcroft Foundation grant (to ST) and two developmental Grants (to ST and to CLS) from the Johns Hopkins University Center for AIDS Research (JHU-CFAR), an NIH-funded program (P30AI094189). WK’s work on HIV and gut microbiome is supported by developmental grants from the Clinical Translational Science Institution at Children’s National (CTSI-CN) and the District of Columbia CFAR (DC CFAR), an NIH-funded program (AI117970). Both JHU-CFAR and DC CFAR are supported by the following NIH Co-Funding and Participating Institutes and Centers: NIAID, NCI, NICHD, NHLBI, NIDA, NIMH, NIA, FIC, NIGMS, NIDDK, and OAR. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
ST has consulted for Biofire Diagnostics and Roche Molecular Diagnostics and has received a speaker honorarium from Roche Molecular Diagnostics. CLS receives unrelated research support from Bristol Myers Squibb and Janssen and received a speaker honorarium from Merck in 2019.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Tuddenham, S., Koay, W.L. & Sears, C. HIV, Sexual Orientation, and Gut Microbiome Interactions. Dig Dis Sci 65, 800–817 (2020). https://doi.org/10.1007/s10620-020-06110-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-020-06110-y