Abstract
Background/Aims
While stress has been implicated in functional dyspepsia (FD), the mechanisms by which stress results in symptoms are not well defined. The aim of the current study was to assess gastric myoelectric and autonomic changes in response to a physical stressor in youth with FD.
Methods
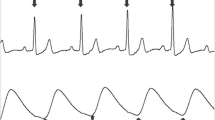
In a group of healthy controls and pediatric FD subjects, we recorded ECG and EGG signals 30 min before and 60 min after, a cold pressor task (CPT). Gastric EGG and heart rate variability (HRV) parameters were calculated in pre- and post-CPT stages and in short intervals.
Results
The pre-CPT percent tachygastria was higher in FD subjects as compared to controls. However, CPT did not induce any EGG changes in either controls or FD subjects and the two groups did not differ from each other post-CPT. The CPT resulted in an increase in HRV and standard deviation of NN intervals in controls; there was no change in any HRV parameter in FD subjects.
Conclusions
Acute physical stress does not appear to induce gastric electrical abnormalities in youth with FD. Youth with FD appear to lack the normal flexible autonomic response to a physical stressor.







Similar content being viewed by others
References
Chitkara DK, Rawat DJ, Talley NJ. The epidemiology of childhood recurrent abdominal pain in western countries: a systematic review. Am J Gastroenterol. 2005;100:1868–1875. https://doi.org/10.1111/j.1572-0241.2005.41893.x.
Rasquin A, Di Lorenzo C, Forbes D, et al. Childhood functional gastrointestinal disorders: child/adolescent. Gastroenterology. 2006;130:1527–1537. https://doi.org/10.1053/j.gastro.2005.08.063.
Hyams JS, Di Lorenzo C, Saps M, Shulman RJ, Staiano A, Van Tilburg M. Childhood functional gastrointestinal disorders: child/adolescent. Gastroenterology. 2016;150:1456–1468. https://doi.org/10.1053/j.gastro.2016.02.015.
Walker LS, Lipani TA, Greene JW, et al. Recurrent abdominal pain symptom subtypes based on the Rome II criteria for pediatric functional gastrointestinal disorders. J Pediatr Gastroenterol Nutr. 2004;38:187–191.
Schurman JV, Friesen CA, Danda CE, et al. Diagnosing functional abdominal pain with the Rome II criteria: parent, child, and clinician agreement. J Pediatr Gasroenterol Nutr. 2005;41:291–295. https://doi.org/10.1097/01.mpg.0000178438.64675.c4.
Edwards T, Friesen C, Schurman JV. Classification of pediatric functional gastrointestinal disorders related to abdominal pain using Rome III versus Rome IV criterions. BMC Gastroenterol. 2018;18:41. https://doi.org/10.1186/s12876-018-0769-z.
Robin SG, Keller C, Zwiener R, et al. Prevalence of pediatric functional gastrointestinal disorders utilizing the Rome IV criteria. J Pediatr. 2018;195:134–139. https://doi.org/10.1016/j.jpeds.2017.12.012.
Koloski NA, Jones M, Talley NJ. Evidence that independent gut-to-brain and brain-to-gut pathways operate in the irritable bowel syndrome and functional dyspepsia: a 1-year population-based prospective study. Aliment Pharmacol Ther. 2016;44:592–600. https://doi.org/10.1111/apt.13738.
Tougas G, Kamath M, Watteel G, et al. Modulation of neurocardiac function by esophageal stimulation in humans. Clin Soc. 1997;92:167–174. https://doi.org/10.1042/cs0920167.
Tougas G. The autonomic nervous system in functional bowel disorder. Gut. 2000;47:iv78–iv80. https://doi.org/10.1136/gut.47.suppl_4.iv78.
Bharucha AE, Camilleri M, Low PA, Zinsmeister AR. Autonomic dysfunction In gastrointestinal motility disorder. Gut. 1993;34:397–401. https://doi.org/10.1136/gut.34.3.397.
Kamath VK, Fallen EL. Power spectral analysis of heart rate variability: a non-invasive signature of cardiac autonomic function. Crit Rev Biomed Eng. 1993;21:245–311.
Shaffer F, Ginsberg JP. An overview of heart rate variability metrics and norms. Front Public Health. 2017;5:258. https://doi.org/10.3389/fpubh.2017.00258.
Pagani M, Lombardi F, Guzzetti S, et al. Power spectral analysis of heart rate and arterial pressure variabilities as a marker of sympatho-vagal interaction in man and conscious dog. Circ Res. 1986;59:178–193. https://doi.org/10.1161/01.res.59.2.178.
Akselrod S, Gordon D, Ubel FA, Shannon DC, Berger AC, Cohen RJ. Power spectral analysis of heart rate fluctuations: a quantitative probe of beat-to-beat cardiovascular control. Science. 1981;213:220–222. https://doi.org/10.1126/science.6166045.
Mazurak N, Seredyuk N, Sauer H, Teufel M, Enck P. Heart rate variability in the irritable bowel syndrome: a review of the literature. Neurogastroenterol Motil. 2012;24:206–216. https://doi.org/10.1111/j.1365-2982.2011.01866.x.
Arlt J, Jahn H, Kellner M, Ströhle A, Yassouridis A, Wiedemann K. Modulation of Sympathetic activity by corticotrophin-releasing hormone and atrial natriuretic peptide. Neuropeptides. 2003;37:362–368. https://doi.org/10.1016/j.npep.2003.09.006.
Walker LS, Stone AL, Smith CA, et al. Interacting influences of gender and chronic pain status on parasympathetically-mediated heart rate variability in adolescents and young adults. Pain. 2017;158:1509–1516. https://doi.org/10.1097/j.pain.0000000000000942.
Friesen CA, Lin Z, Schurman JV, Andre L, McCallum RW. Autonomic nervous system response to a solid meal and water loading in healthy children: its relation to gastric myoelectric activity. Neurogastroenterol Motil. 2007;19:376–382. https://doi.org/10.1111/j.1365-2982.2007.00906.x.
Chen J, Richards R, McCallum RW. Identification of gastric contraction from the cutaneous electrogastrogram. Am J Gastroenterol. 1994;89:79–85.
Friesen CA, Lin Z, Hyman PE, et al. Electrogastrography in pediatric functional dyspepsia: relationship to gastric emptying and symptom severity. J Pediatr Gastroenterol Nutr. 2006;42:265–269. https://doi.org/10.1097/01.mpg.0000189367.99416.5e.
Chen JD, Lin X, Zhang M, Torres-Pinedo RB, Orr WC. Gastric myoelectrical activity in healthy children and children with functional dyspepsia. Dig Dis Sci. 1998;43:2384–2391. https://doi.org/10.1023/A:1026661627304.
Friesen CA, Lin Z, Garola R, et al. Chronic gastritis is not associated with gastric dysrhythmia or delayed solid emptying in children with dyspepsia. Dig Dis Sci. 2005;50:1012–1018. https://doi.org/10.1007/s10620-005-2696-4.
Leung MWY, Wong BPY, Chao NSY, Chung KW, Kwok WK, Liu KKW. Electrogastrography in the management of pediatric functional dyspepsia and motility disorder. J Pediatr Surg. 2006;41:2069–2072. https://doi.org/10.1016/j.jpedsurg.2006.08.008.
Riezzo G, Chiloiro M, Guerra V, Borrelli O, Salvia G, Cucchiara S. Comparison of gastric electrical activity and gastric emptying in healthy and dyspeptic children. Dig Dis Sci. 2000;45:517–524. https://doi.org/10.1023/A:1005493123557.
Von Baeyer CL, Piira T, Chambers CT, Trapanotto M, Zeltzer LK. Guidelines for the cold pressor task as an experimental pain stimulus for use with children. J Pain. 2005;6:218–227. https://doi.org/10.1016/j.jpain.2005.01.349.
Birnie KA, Petter M, Boerner KE, Noel M, Chambers CT. Contemporary use of the cold pressor task in pediatric pain research: a systematic review of methods. J Pain. 2012;13:817–826. https://doi.org/10.1016/j.jpain.2012.06.005.
Riezzo G, Porcelli P, Guerra V, Giorgio I. Effects of different psychophysiological stressors on the cutaneous electrogastrogram in healthy subjects. Acch Physiol Biochem. 1996;104:282–286. https://doi.org/10.1076/apab.104.3.282.12899.
Homma S. Correlations between anxiety and the stress responses of electrogastrography (EGG) induced by the mirror drawing test (MDT). J Smooth Muscle Res. 2014;50:1–7. https://doi.org/10.1540/jsmr.50.1.
De Giorgi F, Sarnelli G, Cirillo C, et al. Increased severity of dyspeptic symptoms related to mental stress is associated with sympathetic hyperactivity and enhanced endocrine response in patients with postprandial distress syndrome. Neurogastroenterol Motil. 2013;25:31-e3. https://doi.org/10.1111/nmo.12004.
Homma S. Correlations between the responses of electrogastrograms, heart rate and respiratory rate to the stress of the mirror drawing test in human subjects. J Smooth Muscle Res. 2006;42:9–19. https://doi.org/10.1540/jsmr.42.9.
Homma S. Local differences in electrogastrographic responses ti the stress of the mirror drawing test (MDT) as determined by multichannel electrogastrography. J Smooth Muscle Res. 2012;48:47–57. https://doi.org/10.1540/jsmr.48.47.
Dal K, Deveci OS, Kucukazman M, et al. Decreased parasympathetic activity in patients with functional dyspepsia. Eur J Gastroenterol Hepatol. 2014;26:748–752. https://doi.org/10.1097/meg.0000000000000111.
Lorena SL, Figueiredo MJ, Almeida JR, Mesquita MA. Autonomic function in patients with functional dyspepsia assessed by 24-h heart rate variability. Dig Dis Sci. 2002;47:27–31. https://doi.org/10.1023/A:1013246900041.
Jarrett M, Heitkemper M, Czyzewski D, Zeltzer L, Shulman RJ. Autonomic nervous system function in young children with functional abdominal pain or irritable bowel syndrome. J Pain. 2012;13:477–484. https://doi.org/10.1016/j.jpain.2012.02.007.
Puzanovova M, Arbogast PG, Smith CA, Anderson J, Diedrich A, Walker LS. Autonomic activity and somatic symptoms in response to success versus failure on a cognitive task: a comparison of chronic abdominal pain patients and well children. J Psychosom Res. 2009;67:235–243. https://doi.org/10.1016/j.jpsychores.2009.02.007.
Sharma RK, Balhara YP, Sagar R, Deepak KK, Mehta M. Heart rate variability study of childhood anxiety disorders. J Cardiovasc Dis Res. 2011;2:115–122. https://doi.org/10.4103/0975-3583.83040.
Schurman JV, Friesen CA. Identifying potential pediatric chronic abdominal pain triggers using ecological momentary assessment. Clin Pract Pediatr Psychol. 2015;3:131–141. https://doi.org/10.1037/cpp0000095.
Schurman JV, Danda CE, Friesen CA, Hyman PE, Simon SD, Cocjin JT. Variations in psychological profile among children with recurrent abdominal pain. J Clin Psychol Med Settings. 2008;15:241–251. https://doi.org/10.1007/s10880-008-9120-0.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments.
Informed consent
Assent was obtained from each participant, and consent was obtained from the legal guardian of each participant.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Vargas-Luna, F.M., Huerta-Franco, M.R., Schurman, J.V. et al. Heart Rate Variability and Gastric Electrical Response to a Cold Pressor Task in Youth with Functional Dyspepsia. Dig Dis Sci 65, 1074–1081 (2020). https://doi.org/10.1007/s10620-019-05848-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-019-05848-4