Abstract
Background
Traditionally in Asia, hepatitis B (HBV) accounts for the majority of hepatocellular carcinoma (HCC), but increasingly, non-viral or nonalcoholic steatohepatitis (NASH) etiology may play a more prominent role with current socioeconomic changes. There remains a paucity in data comparing NASH–HCC to HBV-related HCC. In this study, we explored the differences in clinical characteristics between HBV- and cryptogenic-related HCC.
Methods
Patients with HCC seen in the Department of Gastroenterology and Hepatology, Singapore General Hospital were enrolled in an ongoing database since 1980. Patients with HCC attributed to HBV or cryptogenic etiology were identified. Comparison of clinical characteristics was performed between the two groups.
Results
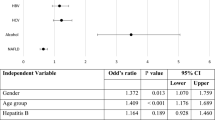
There were 916 HBV–HCC patients and 163 cryptogenic HCC patients, accounting for 70.9% and 12.6% of the total HCC cases (1292 patients), respectively. Out of the total cohort enrolled from 1980 to 2005, the ratio of cryptogenic to HBV patients was 1:6.7, while from 2006 to the current year, the ratio of cryptogenic to HBV patients has increased significantly to 1:3.9. Relative to patients with HBV, cryptogenic HCC patients were older (67.6 vs. 59.4 years old; p < 0.001), had lower proportion of male patients (69.9% vs. 83.8%; p < 0.001), and had higher incidence of smoking (32.2% vs. 25.8%; p = 0.008). HBV group had higher alanine transaminase (60.9 ± 85.7 U/L vs. 48.0 ± 52.1 U/L; p = 0.003), hemoglobin (12.7 ± 2.28 g/dL vs. 12.0 ± 2.46 g/dL, p < 0.001), albumin (32.9 ± 6.8 g/L vs. 31.3 ± 7.7 g/L; p = 0.007), and prothrombin time (13.2 ± 2.95 s vs. 12.7 ± 2.01 s, p = 0.023), as compared to the cryptogenic group. Cryptogenic HCC patients presented more frequently with unifocal HCC (55.2% vs. 46.5%; p = 0.002). There was no difference in the proportions of patients receiving surgical resection in both groups (23.5% in HBV group vs. 17.9% in cryptogenic group; p = 0.202). Cox regression analysis revealed no survival difference between cryptogenic-related HCC and HBV-related HCC (p = 0.367).
Conclusion
Temporal trends suggest that HCC attributed to HBV is on the decline, while cryptogenic- or NASH-related HCC is an emerging clinical entity. A paradigm shift in approach to screening, surveillance, and management of HCC may be required in view of the changing landscape of HCC epidemiology into an increasing non-viral etiology.


Similar content being viewed by others
References
Ferlay J, Soerjomataram I, Ervik M, et al. GLOBOCAN 2012 v1.1, Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 11 [Internet]. Lyon, France: International Agency for Research on Cancer; 2014. Available from: http://globocan.iarc.fr. Accessed April 24, 2018.
Bosch FX, Ribes J, Cleries R, et al. Epidemiology of hepatocellular carcinoma. Clin Liver Dis. 2005;9(191–211):v.
El-Serag HB, Rudolph KL. Hepatocellular carcinoma: epidemiology and molecular carcinogenesis. Gastroenterology. 2007;132:2557–2576.
Dyson J, Jaques B, Chattopadyhay D, et al. Hepatocellular cancer: the impact of obesity, type 2 diabetes and a multidisciplinary team. J Hepatol. 2014;60:110–117.
Loomba R, Sanyal AJ. The global NAFLD epidemic. Nat Rev Gastroenterol Hepatol. 2013;10(11):686–690.
Goh GB, McCullough AJ. Natural history of nonalcoholic fatty liver disease. Dig Dis Sci. 2016;61(5):1226–1233.
Younossi ZM, Koenig AB, Abdelatif D, et al. Global epidemiology of nonalcoholic fatty liver disease: metaanalytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64:73–84.
Goh GBB, Chang PE, Tan CK. Changing epidemiology of hepatocellular carcinoma in Asia. Best Pract Res Clin Gastroenterol. 2015;29(6):919–928.
Bugianesi E, Leone N, Vanni E, et al. Expanding the natural history of nonalcoholic steatohepatitis: from cryptogenic cirrhosis to hepatocellular carcinoma. Gastroenterology. 2002;123(1):134–140.
Regimbeau JM, Colombat M, Mognol P, et al. Obesity and diabetes as a risk factor for hepatocellular carcinoma. Liver Tx. 2004;10(2 Suppl 1):S69–S73.
Poonawala A, Nair SP, Thuluvah PJ. Prevalence of obesity and diabetes in patients with cryptogenic cirrhosis: a case-control study. Hepatology. 2000;32(4 Pt 1):689–692.
Yoshioka Y, Hashimoto E, Yatsuji S, et al. Nonalcoholic steatohepatitis: cirrhosis, hepatocellular carcinoma, and burnt-out NASH. J Gastroenterol. 2004;39:1215–1218.
Giannini EG, Marabotto E, Savarino V, et al. Hepatocellular carcinoma in patients with cryptogenic cirrhosis. Clin Gastroenterol Hepatol. 2009;7:580–585.
Yatsuji S, Hashimoto E, Tobari M, et al. Clinical features and outcomes of cirrhosis due to non-alcoholic steatohepatitis compared with cirrhosis caused by chronic hepatitis C. J Gastroenterol Hepatol. 2009;24(2):248–254.
Piscaglia F, Svegliati-Baroni G, Barchetti A, et al. Clinical patterns of hepatocellular carcinoma in nonalcoholic fatty liver disease: A multicenter prospective study. Hepatology. 2016;63:827–838.
Sanyal AJ, Banas C, Sargeant C, et al. Similarities and differences in outcomes of cirrhosis due to nonalcoholic steatohepatitis and hepatitis C. Hepatology. 2006;43:682–689.
Weinmann A, Alt Y, Koch S, et al. Treatment and survival of non-alcoholic steatohepatitis associated hepatocellular carcinoma. BMC Cancer. 2015;15:210.
Goh GB, Li JW, Chang PE, et al. Deciphering the epidemiology of hepatocellular carcinoma through the passage of time: A study of 1,401 patients across 3 decades. Hepatol Commun. 2017;1(6):564–571.
European Association for the Study of the Liver. EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma. J Hepatol. (2018), https://doi.org/10.1016/j.jhep.2018.03.019. Accessed May 24, 2018.
Cancer Survival in Singapore 1968-2002. Singapore Cancer Registry, National Registry of Diseases Office. Ministry of Health, Singapore.
Kwak HW, Park JW, Koh YH, et al. Clinical characteristics of patients with cryptogenic hepatocellular carcinoma in a hepatitis B virus-endemic area. Liver Cancer. 2016;5(1):21–36.
Hashimoto E, Tokushige K. Prevalence, gender, ethnic variations, and prognosis of NASH. J Gastroenterol. 2011;46(Suppl 1):63–69.
Kawamura Y, Arase Y, Ikeda K, et al. Large-scale long-term follow-up study of Japanese patients with non-alcoholic fatty liver disease for the onset of hepatocellular carcinoma. Am J Gastroenterol. 2012;107:253–261.
Sadler EM, Mehta N, Bhat M, et al. Liver transplantation for NASH-related hepatocellular carcinoma versus non-NASH etiologies of hepatocellular carcinoma. Transplantation. 2018;102(4):640–647.
Ertle J, Dechene A, Sowa JP, et al. Non-alcoholic fatty liver disease progresses to hepatocellular carcinoma in the absence of apparent cirrhosis. Int J Cancer. 2011;128(10):2436–2443.
Paradis V, Zalinski S, Chelbi E, et al. Hepatocellular carcinomas in patients with metabolic syndrome often develop without significant liver fibrosis: a pathological analysis. Hepatology. 2009;49:851–859.
Yasui K, Hashimot o E, Komorizono Y, et al. Characteristics of patients with nonalcoholic steatohepatitis who develop hepatocellular carcinoma. Clin Gastroenterol Hepatol. 2011; 9:428–433, quiz e50.
Mittal S, Sada YH, El-Serag HB, et al. Temporal trends of nonalcoholic fatty liver disease-related hepatocellular carcinoma in the veteran affairs population. Clin Gastroenterol Hepatol. 2015;13:594–601.
Baffy G, Brunt EM, Caldwell SH. Hepatocellular carcinoma in non-alcoholic fatty liver disease: an emerging menace. J Hepatol. 2012;56(6):1384–1391.
D’Avola D, Labgaa I, Villanueva A. Natural history of nonalcoholic steatohepatitis/nonalcoholic fatty liver disease-hepatocellular carcinoma: Magnitude of the problem from a hepatology clinic perspective. Clinical Liver Disease. 2016;8:100–104.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflict of interest.
Rights and permissions
About this article
Cite this article
Liew, ZH., Goh, G.BB., Hao, Y. et al. Comparison of Hepatocellular Carcinoma in Patients with Cryptogenic Versus Hepatitis B Etiology: A Study of 1079 Cases Over 3 Decades. Dig Dis Sci 64, 585–590 (2019). https://doi.org/10.1007/s10620-018-5331-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-018-5331-x