Abstract
Background
The fatty acid profile of the fecal metabolome and its association with colorectal cancer (CRC) has not been fully evaluated.
Aims
We aimed to compare the fecal fatty acid profiles of CRC patients and healthy controls.
Methods
We enrolled 26 newly diagnosed CRC patients and 28 healthy individuals between July 2014 and August 2014 from our institute. Long- and short-chain fatty acids were extracted from fecal samples and analyzed using gas chromatography–mass spectrometry.
Results
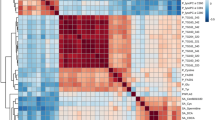
Regarding fecal long-chain fatty acids, the levels of total ω-6 polyunsaturated fatty acids and, particularly, of linoleic acid (C18:2ω-6) were significantly higher in male CRC patients than in healthy men (2.750 ± 2.583 vs. 1.254 ± 0.966 µg/mg feces, P = 0.040; 2.670 ± 2.507 vs. 1.226 ± 0.940 µg/mg feces, P = 0.034, respectively). In addition, the levels of total monounsaturated fatty acid and, particularly, of oleic acid (C18:1ω-9) were significantly higher in male CRC patients than in healthy men (1.802 ± 1.331 vs. 0.977 ± 0.625 µg/mg feces, P = 0.027; 1.749 ± 1.320 vs. 0.932 ± 0.626 µg/mg feces, P = 0.011, respectively). However, those differences were not shown in female gender. The level of fecal short-chain fatty acids was not different between CRC patients and healthy controls.
Conclusions
There were changes in the profiles of fecal fatty acid metabolomes in CRC patients compared to healthy controls, implying that fecal fatty acids could be used as a novel screening tool for CRC.

Similar content being viewed by others
References
Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. CA Cancer J Clin. 2005;55:74–108.
Haggar FA, Boushey RP. Colorectal cancer epidemiology: incidence, mortality, survival, and risk factors. Clin Colon Rectal Surg. 2009;22:191–197.
Bingham SA. Diet and colorectal cancer prevention. Biochem Soc Trans. 2000;28:12–16.
Park SY, Boushey CJ, Wilkens LR, Haiman CA, Le Marchand L. High-quality diets associate with reduced risk of colorectal cancer: analyses of diet quality indexes in the multiethnic cohort. Gastroenterology. 2017;153:386–394.
Das S, Martinez LR, Ray S. Phospholipid remodeling and eicosanoid signaling in colon cancer cells. Indian J Biochem Biophys. 2014;51:512–519.
Bamia C, Lagiou P, Buckland G, et al. Mediterranean diet and colorectal cancer risk: results from a European cohort. Eur J Epidemiol. 2013;28:317–328.
De Filippo C, Cavalieri D, Di Paola M, et al. Impact of diet in shaping gut microbiota revealed by a comparative study in children from Europe and rural Africa. Proc Natl Acad Sci U S A. 2010;107:14691–14696.
Walker AW, Ince J, Duncan SH, et al. Dominant and diet-responsive groups of bacteria within the human colonic microbiota. ISME J. 2011;5:220–230.
Xiao L, Sonne SB, Feng Q, et al. High-fat feeding rather than obesity drives taxonomical and functional changes in the gut microbiota in mice. Microbiome. 2017;5:43.
Quigley EM. Gut bacteria in health and disease. Gastroenterol Hepatol (N Y). 2013;9:560–569.
Sobhani I, Tap J, Roudot-Thoraval F, et al. Microbial dysbiosis in colorectal cancer (CRC) patients. PLoS One. 2011;6:e16393.
Castellarin M, Warren RL, Freeman JD, et al. Fusobacterium nucleatum infection is prevalent in human colorectal carcinoma. Genome Res. 2012;22:299–306.
Jacob H, Toyonaga T, Ohara Y, et al. Endoscopic submucosal dissection of cecal lesions in proximity to the appendiceal orifice. Endoscopy. 2016;48:829–836.
Wisniewski JR, Dus-Szachniewicz K, Ostasiewicz P, Ziolkowski P, Rakus D, Mann M. Absolute proteome analysis of colorectal mucosa, adenoma, and cancer reveals drastic changes in fatty acid metabolism and plasma membrane transporters. J Proteome Res. 2015;14:4005–4018.
Jacobs DM, Deltimple N, van Velzen E, et al. (1)H NMR metabolite profiling of feces as a tool to assess the impact of nutrition on the human microbiome. NMR Biomed. 2008;21:615–626.
Matsumoto M, Benno Y. Consumption of Bifidobacterium lactis LKM512 yogurt reduces gut mutagenicity by increasing gut polyamine contents in healthy adult subjects. Mutat Res. 2004;568:147–153.
Awad AB, Chattopadhyay JP, Danahy ME. Effect of dietary fat composition on rat colon plasma membranes and fecal lipids. J Nutr. 1989;119:1376–1382.
Park Y, Lee J, Oh JH, Shin A, Kim J. Dietary patterns and colorectal cancer risk in a Korean population: a case-control study. Medicine (Baltimore). 2016;95:e3759.
Folch J, Lees M, Sloane Stanley GH. A simple method for the isolation and purification of total lipides from animal tissues. J Biol Chem. 1957;226:497–509.
Pickens CA, Albuquerque Pereira MF, Fenton JI. Long-chain omega-6 plasma phospholipid polyunsaturated fatty acids and association with colon adenomas in adult men: a cross-sectional study. Eur J Cancer Prev. 2017;26:497–505.
McEntee MF, Whelan J. Dietary polyunsaturated fatty acids and colorectal neoplasia. Biomed Pharmacother. 2002;56:380–387.
Hodge AM, Williamson EJ, Bassett JK, MacInnis RJ, Giles GG, English DR. Dietary and biomarker estimates of fatty acids and risk of colorectal cancer. Int J Cancer. 2015;137:1224–1234.
Weijenberg MP, Luchtenborg M, de Goeij AF, et al. Dietary fat and risk of colon and rectal cancer with aberrant MLH1 expression, APC or KRAS genes. Cancer Causes Control. 2007;18:865–879.
Cottet V, Collin M, Gross AS, et al. Erythrocyte membrane phospholipid fatty acid concentrations and risk of colorectal adenomas: a case-control nested in the French E3 N-EPIC cohort study. Cancer Epidemiol Biomarkers Prev. 2013;22:1417–1427.
Macquart-Moulin G, Riboli E, Cornee J, Charnay B, Berthezene P, Day N. Case-control study on colorectal cancer and diet in Marseilles. Int J Cancer. 1986;38:183–191.
Bartoli R, Fernandez-Banares F, Navarro E, et al. Effect of olive oil on early and late events of colon carcinogenesis in rats: modulation of arachidonic acid metabolism and local prostaglandin E(2) synthesis. Gut. 2000;46:191–199.
Audano M, Maldini M, De Fabiani E, Mitro N, Caruso D. Gender-related metabolomics and lipidomics: from experimental animal models to clinical evidence. J Proteomics. 2017. https://doi.org/10.1016/j.jprot.2017.11.001.
Psihogios NG, Gazi IF, Elisaf MS, Seferiadis KI, Bairaktari ET. Gender-related and age-related urinalysis of healthy subjects by NMR-based metabonomics. NMR Biomed. 2008;21:195–207.
Krumsiek J, Mittelstrass K, Do KT, et al. Gender-specific pathway differences in the human serum metabolome. Metabolomics. 2015;11:1815–1833.
Jove M, Mate I, Naudi A, et al. Human aging is a metabolome-related matter of gender. J Gerontol A Biol Sci Med Sci. 2016;71:578–585.
Gonzalez-Covarrubias V, Beekman M, Uh HW, et al. Lipidomics of familial longevity. Aging Cell. 2013;12:426–434.
Farshidfar F, Weljie AM, Kopciuk KA, et al. A validated metabolomic signature for colorectal cancer: exploration of the clinical value of metabolomics. Br J Cancer. 2016;115:848–857.
Xie G, Wang X, Zhao A, et al. Sex-dependent effects on gut microbiota regulate hepatic carcinogenic outcomes. Sci Rep. 2017;7:45232.
Ridlon JM, Ikegawa S, Alves JM, et al. Clostridium scindens: a human gut microbe with a high potential to convert glucocorticoids into androgens. J Lipid Res. 2013;54:2437–2449.
Weir TL, Manter DK, Sheflin AM, Barnett BA, Heuberger AL, Ryan EP. Stool microbiome and metabolome differences between colorectal cancer patients and healthy adults. PLoS One. 2013;8:e70803.
Bornet FR, Brouns F, Tashiro Y, Duvillier V. Nutritional aspects of short-chain fructooligosaccharides: natural occurrence, chemistry, physiology and health implications. Dig Liver Dis. 2002;34:S111–S120.
Wong JM, de Souza R, Kendall CW, Emam A, Jenkins DJ. Colonic health: fermentation and short chain fatty acids. J Clin Gastroenterol. 2006;40:235–243.
Wang T, Cai G, Qiu Y, et al. Structural segregation of gut microbiota between colorectal cancer patients and healthy volunteers. ISME J. 2012;6:320–329.
Deda O, Gika H, Panagoulis T, Taitzoglou I, Raikos N, Theodoridis G. Impact of exercise on fecal and cecal metabolome over aging: a longitudinal study in rats. Bioanalysis. 2017;9:21–36.
Author information
Authors and Affiliations
Contributions
EMS, JSB, and JYJ designed the study; SML, HJY, SJK, SHL, KJC, SWH, and DHY collected, interpreted, and analyzed the data; EMS performed the statistical analysis; SHL, KJC, SWH, and DHY cared for the patients and critically reviewed the manuscript; EMS, JSB, and JYJ drafted the manuscript; and JSB and JYJ are the guarantors of the article and approved the final manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
Eun Mi Song, Jeong-Sik Byeon, Sun Mi Lee, Hyun Ju Yoo, Su Jung Kim, Sun-Ho Lee, Kiju Chang, Sung Wook Hwang, Dong-Hoon Yang, and Jin-Yong Jeong have no conflict of interest or financial ties to declare.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Song, E.M., Byeon, JS., Lee, S.M. et al. Fecal Fatty Acid Profiling as a Potential New Screening Biomarker in Patients with Colorectal Cancer. Dig Dis Sci 63, 1229–1236 (2018). https://doi.org/10.1007/s10620-018-4982-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-018-4982-y