Abstract
Background
Young age and thiopurine therapy are risk factors for lymphoproliferative disease among patients with inflammatory bowel disease (IBD).
Aims
The aims of this study were to evaluate the prevalence of seropositivity for the Epstein–Barr virus (EBV) and human cytomegalovirus (CMV) among children and adolescents with IBD, to assess the viral load of EBV, CMV, and BK and JC polyomaviruses (BKV, JCV) in these patients, and to assess the influence of different therapeutic regimens on seroprevalence and viral load.
Methods
Children who had been followed in our center were tested for EBV, CMV, BKV, and JCV in a cross-sectional study. One hundred and six children were included who had Crohn’s disease (68 %), ulcerative colitis (29 %), and unclassified IBD (3 %).
Results
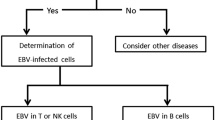
We found that 64 % of patients were EBV seropositive. The proportion of EBV seropositive patients increased during childhood. Azathioprine therapy (p = 0.003) was associated with EBV seropositivity in a multiple logistic regression model, after adjusting for gender, age, and disease activity at determination. We found a significant association between the number of polymerase chain reaction copies and infliximab dose (p = 0.023). We did not find any significant association between CMV serology and CMV, BKV, or JCV viral load, or any other therapeutic regimen or clinical characteristics.
Conclusions
Treatment with azathioprine appears to be a risk factor for early EBV seropositivity in children with IBD, and the infliximab dose was associated with a higher EBV viral load.



Similar content being viewed by others
References
Magro F, Peyrin-Biroulet L, Sokol H, et al. Extra-intestinal malignancies in inflammatory bowel disease: results of the 3rd ECCO Pathogenesis Scientific Workshop (III). J Crohns Colitis. 2014;8:31–44.
Pietersma F, Piriou E, van Baarle D. Immune surveillance of EBV-infected B cells and the development of non-Hodgkin lymphomas in immunocompromised patients. Leuk Lymphoma. 2008;49:1028–1041.
Baecklund E, Iliadou A, Askling J, et al. Association of chronic inflammation, not its treatment, with increased lymphoma risk in rheumatoid arthritis. Arthritis Rheum. 2006;54:692–701.
Beaugerie L, Brousse N, Bouvier AM, et al. Lymphoproliferative disorders in patients receiving thiopurines for inflammatory bowel disease: a prospective observational cohort study. Lancet. 2009;374:1617–1625.
Kandiel A, Fraser AG, Korelitz BI, Brensinger C, Lewis JD. Increased risk of lymphoma among inflammatory bowel disease patients treated with azathioprine and 6-mercaptopurine. Gut. 2005;54:1121–1125.
Dayharsh GA, Loftus EV Jr, Sandborn WJ, et al. Epstein–Barr virus-positive lymphoma in patients with inflammatory bowel disease treated with azathioprine or 6-mercaptopurine. Gastroenterology. 2002;122:72–77.
Shale M, Kanfer E, Panaccione R, Ghosh S. Hepatosplenic T cell lymphoma in inflammatory bowel disease. Gut. 2008;57:1639–1641.
Mackey AC, Green L, Leptak C, Avigan M. Hepatosplenic T cell lymphoma associated with infliximab use in young patients treated for inflammatory bowel disease: update. J Pediatr Gastroenterol Nutr. 2009;48:386–388.
Kotlyar DS, Blonski W, Diamond RH, Wasik M, Lichtenstein GR. Hepatosplenic T-cell lymphoma in inflammatory bowel disease: a possible thiopurine-induced chromosomal abnormality. Am J Gastroenterol. 2010;105:2299–2301.
Biank VF, Sheth MK, Talano J, et al. Association of Crohn’s disease, thiopurines, and primary Epstein–Barr virus infection with hemophagocytic lymphohistiocytosis. J Pediatr. 2011;159:808–812.
Bosetti C, Levi F, Ferlay J, Lucchini F, Negri E, La Vecchia C. Incidence and mortality from non-Hodgkin lymphoma in Europe: the end of an epidemic? Int J Cancer. 2008;123:1917–1923.
Stevens SJ, Verschuuren EA, Pronk I, et al. Frequent monitoring of Epstein–Barr virus DNA load in unfractionated whole blood is essential for early detection of posttransplant lymphoproliferative disease in high-risk patients. Blood. 2001;97:1165–1171.
Love KA, Henderson P, Garrick V, Barclay AR, McGrogan P, Russell RK. Letter: Epstein–Barr virus status may be especially important in paediatric IBD populations. Aliment Pharmacol Ther. 2013;39:231–232.
Comar M, Delbue S, Lepore L, et al. Latent viral infections in young patients with inflammatory diseases treated with biological agents: prevalence of JC virus genotype 2. J Med Virol. 2013;85:716–722.
Sari I, Birlik M, Gonen C, et al. Cytomegalovirus colitis in a patient with Behcet’s disease receiving tumor necrosis factor alpha inhibitory treatment. World J Gastroenterol. 2008;14:2912–2914.
Torre-Cisneros J, Fortun J, Aguado JM, et al. Consensus document from GESITRA-SEIMC on the prevention and treatment of cytomegalovirus infection in transplanted patients. Enferm Infecc Microbiol Clin. 2005;23:424–437.
Lavagna A, Bergallo M, Daperno M, et al. Infliximab and the risk of latent viruses reactivation in active Crohn’s disease. Inflamm Bowel Dis. 2007;13:896–902.
Giannecchini S, Clausi V, Vultaggio A, et al. Assessment of the risk of polyomavirus JC reactivation in patients with immune-mediated diseases during long-term treatment with infliximab. J Neurovirol. 2012;18:55–61.
Van Assche G, Van Ranst M, Sciot R, et al. Progressive multifocal leukoencephalopathy after natalizumab therapy for Crohn’s disease. N Engl J Med. 2005;353:362–368.
Dalianis T, Hirsch HH. Human polyomaviruses in disease and cancer. Virology. 2013;437:63–72.
Kimura H, Morita M, Yabuta Y, et al. Quantitative analysis of Epstein–Barr virus load by using a real-time PCR assay. J Clin Microbiol. 1999;37:132–136.
Leung AY, Chan M, Tang SC, Liang R, Kwong YL. Real-time quantitative analysis of polyoma BK viremia and viruria in renal allograft recipients. J Virol Methods. 2002;103:51–56.
McNees AL, White ZS, Zanwar P, Vilchez RA, Butel JS. Specific and quantitative detection of human polyomaviruses BKV, JCV, and SV40 by real time PCR. J Clin Virol. 2005;34:52–62.
Pongers-Willemse MJ, Verhagen OJ, Tibbe GJ, et al. Real-time quantitative PCR for the detection of minimal residual disease in acute lymphoblastic leukemia using junctional region specific TaqMan probes. Leukemia. 1998;12:2006–2014.
Fay MP, Shaw PA. Exact and asymptotic weighted logrank tests for interval censored data: the interval R package. J Stat Softw. 2010;36:1–34.
Linton MS, Kroeker K, Fedorak D, Dieleman L, Fedorak RN. Prevalence of Epstein–Barr virus in a population of patients with inflammatory bowel disease: a prospective cohort study. Aliment Pharmacol Ther. 2013;38:1248–1254.
Cara CJ, Pena AS, Sans M, et al. Reviewing the mechanism of action of thiopurine drugs: towards a new paradigm in clinical practice. Med Sci Monit. 2004;10:RA247–RA254.
Balfour HH Jr, Sifakis F, Sliman JA, Knight JA, Schmeling DO, Thomas W. Age-specific prevalence of Epstein–Barr virus infection among individuals aged 6–19 years in the United States and factors affecting its acquisition. J Infect Dis. 2013;208:1286–1293.
Dowd JB, Palermo T, Brite J, McDade TW, Aiello A. Seroprevalence of Epstein–Barr virus infection in U.S. children ages 6–19, 2003–2010. PLoS One. 2013;8:e64921.
Iida T, Ikeya K, Watanabe F, et al. Looking for endoscopic features of cytomegalovirus colitis: a study of 187 patients with active ulcerative colitis, positive and negative for cytomegalovirus. Inflamm Bowel Dis. 2013;19:1156–1163.
Roblin X, Pillet S, Oussalah A, et al. Cytomegalovirus load in inflamed intestinal tissue is predictive of resistance to immunosuppressive therapy in ulcerative colitis. Am J Gastroenterol. 2011;106:2001–2008.
Rahier JF, Magro F, Abreu C, et al. Second European evidence-based consensus on the prevention, diagnosis and management of opportunistic infections in inflammatory bowel disease. J Crohns Colitis. 2014;8:443–468.
Staras SA, Dollard SC, Radford KW, Flanders WD, Pass RF, Cannon MJ. Seroprevalence of cytomegalovirus infection in the United States, 1988–1994. Clin Infect Dis. 2006;43:1143–1151.
Magro F, Santos-Antunes J, Albuquerque A, et al. Epstein–Barr virus in inflammatory bowel disease-correlation with different therapeutic regimens. Inflamm Bowel Dis. 2013;19:1710–1716.
Gulley ML, Tang W. Using Epstein–Barr viral load assays to diagnose, monitor, and prevent posttransplant lymphoproliferative disorder. Clin Microbiol Rev. 2010;23:350–366.
Raman V, Hollister M, Umer S, et al. A27: polyomavirus excretion in children with rheumatic diseases on immunosuppressive therapy. Arthritis Rheumatol. 2014;66:S42.
Acknowledgments
Supported by the Project (Ministry of Health, Czech Republic) for Conceptual Development of Research Organization 00064203 (University Hospital Motol, Prague, Czech Republic) and Project GA UK No. 136215 by the Charles University in Prague.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hradsky, O., Copova, I., Zarubova, K. et al. Seroprevalence of Epstein–Barr Virus, Cytomegalovirus, and Polyomaviruses in Children with Inflammatory Bowel Disease. Dig Dis Sci 60, 3399–3407 (2015). https://doi.org/10.1007/s10620-015-3764-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-015-3764-z